Nepalda sog'liq - Health in Nepal
Nepalda sog'liqni saqlash xizmatlari ham davlat, ham xususiy sektor tomonidan taqdim etiladi va umuman qondirilmagan deb hisoblanadi xalqaro standartlar. Kasallikning tarqalishi sezilarli darajada yuqori Nepal boshqalarga qaraganda Janubiy Osiyo mamlakatlar, ayniqsa qishloq joylarida.[1][2] Bundan tashqari, mamlakatning topografik va sotsiologik xilma-xilligi davriy yuqumli kasalliklar epidemiyasini keltirib chiqaradi, epizootiya kabi tabiiy xatarlar toshqinlar, o'rmon yong'inlari, ko'chkilar va zilzilalar.[2] Aholining katta qismi, ayniqsa qishloq qashshoqligida yashovchilar yuqumli kasalliklar yuqishi va o'lim xavfi ostida, to'yib ovqatlanmaslik va sog'liq bilan bog'liq boshqa tadbirlar.[2] Shunga qaramay, sog'liqni saqlash sohasidagi ba'zi yaxshilanishlarga guvoh bo'lish mumkin; eng muhimi, onalar salomatligini muhofaza qilish sohasida sezilarli yaxshilanishlar mavjud. Ushbu yaxshilanishlarga quyidagilar kiradi:[3]
- Inson taraqqiyoti indeksi (HDI) 2011 yilda 0,458 gacha o'sdi[4] 1975 yildagi 0,291 dan.[5][6]
- O'lim darajasi davomida tug'ish 1990 yilda 100000 onadan 850 dan 2013 yilda 100000 onadan 190 ga vafot etgan.[7]
- O'lim besh yoshgacha bo'lganlar 2005 yilda 1000 tirik tug'ilgan chaqaloqqa 61,5 dan 2018 yilda 1000 tirik tug'ilgan chaqaloqqa 31,4 ga kamaydi.[8]
- Bolalar o'limi 1990 yildagi 97,70 dan 2015 yilda 29,40 gacha kamaydi.[9]
- Bolalarda to'yib ovqatlanmaslik: Besh yoshgacha bo'lgan bolalar orasida 37% o'sishni to'xtatish, 11% ni yo'qotish va 30% vazn etishmasligi.[10]
- O'rtacha umr ko'rish 2005 yilda 66 yoshdan 2018 yilda 71,5 yoshga ko'tarildi.[11][12]
| Aholining o'sishi | 1.74[13] |
| O'rtacha umr ko'rish | 71.5 [14] |
| Fertillik | 2.18[15] |
| Bolalar o'limi | 29.40[16] |
| Aholi jon boshiga sog'liq uchun umumiy xarajatlar (2014 yil, AQSh dollar) | 137[17] |
| Sog'liqni saqlash xarajatlari yalpi ichki mahsulotga nisbatan% (2014) | 5.8[17] |
Sog'liqni saqlash xarajatlari
2002 yilda sog'liqni saqlashni davlat tomonidan moliyalashtirish har bir kishiga taxminan 2,30 AQSh dollarini tashkil etdi. Sog'liqni saqlash xarajatlarining taxminan 70% o'z mablag'lari hisobidan qilingan. Sog'liqni saqlashga davlat tomonidan ajratilgan mablag '2009 yilda byudjetning taxminan 5,8 foizini tashkil etdi.[18] 2012 yilda Nepal hukumati mamlakatning beshta tumanida universal tibbiy sug'urta bo'yicha sinov dasturini boshladi.[19]
2014 yilga kelib, Nepalning aholi jon boshiga sog'liqni saqlashga harajatlari 137 AQSh dollarini tashkil etdi.[20]
Sog'liqni saqlash infratuzilmasi
2011 yilgacha bo'lgan ma'lumotlarga ko'ra Nepalda 102 kasalxona mavjud. Sog'liqni saqlash xizmatlari, gigiena, oziqlanish va sanitariya Nepalda sifatsiz va aholining katta qismini, xususan qishloq joylarini qamrab ololmaydi.[21] Kambag'allarning asosiy xarajatlari, arzonligi, tibbiy ma'lumotlarning etishmasligi va qarama-qarshi an'anaviy e'tiqodlar tufayli asosiy tibbiy xizmatdan foydalanish imkoniyati cheklangan.[22] Reproduktiv tibbiy yordam cheklangan va ayollar uchun qiyin. Birlashgan Millatlar Tashkilotining 2009 yilgi inson taraqqiyoti to'g'risidagi hisobotida Nepalda fuqaroligi yo'q shaxslar marginallashtirilishi shaklida ijtimoiy tashvish kuchayib borayotgani va hukumatning ijtimoiy nafaqalaridan foydalanish huquqidan mahrum etilganligi ta'kidlangan.[23][24][25]
Ushbu muammolar ko'plab davlat va nodavlat tashkilotlarni (NNTlar ) oilani rejalashtirish, kontratseptsiya vositalaridan foydalanish, turmush o'rtog'i bilan aloqa qilish va xavfsiz onalik amaliyoti, masalan, tug'ruq paytida malakali tug'ruqxona xodimlaridan foydalanish va zudlik bilan emizish kabi odamlarni sog'lom xulq-atvorga chorlaydigan aloqa dasturlarini amalga oshirish.[26]
Mikro-oziq moddalar etishmovchiligi keng tarqalgan bo'lib, homilador ayollarning deyarli yarmi va besh yoshgacha bo'lgan bolalar, shuningdek reproduktiv yoshdagi ayollarning 35% kamqonlik bilan kasallangan. Bolalarning atigi 24% temirga boy oziq-ovqat iste'mol qiladi, bolalarning 24% minimal qabul qilinadigan parhezni qondiradi va homilador ayollarning faqat yarmi homiladorlik paytida tavsiya etilgan temir qo'shimchasini qabul qiladi. Oziqlanishning yomonlashishiga yordam beruvchi omil yuqori diareya tegishli sanitariya sharoitlaridan foydalanishning etishmasligi va Nepalda ochiq defekatsiya amaliyotining keng tarqalgan amaliyoti (44%) tufayli kuchaygan kasalliklar bilan kasallanish.[27]
5 yoshgacha bo'lgan bolalarning ovqatlanishi[28]
Iqtisodiy o'sishning to'xtab qolish davri va siyosiy beqarorlik oziq-ovqat etishmovchiligiga va yuqori darajadagi stavkalarga yordam berdi to'yib ovqatlanmaslik, asosan o'rta va uzoq g'arbiy mintaqalarning tepaliklarida va tog'larida zaif ayollar va bolalar ta'sir qiladi. O'sishi sustlashgan va tezligi past bo'lgan odamlar sonining kamayganiga qaramay, so'nggi yetti yil ichida faqat emizishni ko'payishi bilan birga, besh yoshgacha bo'lgan bolalarning 41 foizi o'sishning sustlashuvidan aziyat chekmoqda, bu esa o'sib bormoqda g'arbiy tog'larda 60% gacha. DHS 2016 hisobotida shuni ko'rsatdiki, Nepalda bolalarning 36 foizi bo'yi past (2 darajadan past), 12 foizi og'ir bo'yi past (3 darajadan past), 5 yoshgacha bo'lgan bolalarning 27 foizi vaznsiz va 5 % og'ir vaznga ega. 5 yoshgacha bo'lgan bolalarning vazni past va vazni kam bo'lgan bolalar foizining o'zgarishini Nepalning shahar va qishloq mintaqalari bilan taqqoslash mumkin, qishloq joylari shaharlarga qaraganda ko'proq ta'sir qiladi (40 foiz o'sish va 31 foiz kam vazn) (32 foiz o'sish va 23 foiz kam vazn). Uy xo'jaliklarida oziq-ovqat iste'mol qilish ko'rsatkichlari va ularning tarqalish darajasi pastligi o'rtasida ijobiy bog'liqlik mavjud qoloqlik, kam vazn va isrof qilish. Xavfsiz oziq-ovqat xonadonidagi bolalar eng past ko'rsatkichga ega (33%), xavfsiz bo'lmagan oilalardagi bolalar esa eng yuqori ko'rsatkichga ega (49%). Xuddi shunday, onalik ta'limi bolalikning sustligi bilan teskari aloqaga ega. Bundan tashqari, vaznning pastligi va qoloqlik masalalari ham ularning kapital mulkiga teskari bog'liqdir. Eng kam boylik kvintilidagi bolalar eng yuqori kvintil (17% bo'yi past va 12% kam vaznli) bolalariga qaraganda bo'yi past (49%) va vazni kam (33%).[29]
So'nggi yigirma yil ichida Nepalda bolalarning ovqatlanish holati yaxshilandi. O'sishi sustlashgan va vazni kam bo'lgan bolalarning pasayish tendentsiyalari 2001 yildan beri kuzatilmoqda. Nepalda bo'yi past bolalar ulushi 2001-2006 yillarda 14%, 2006-2011 yillarda 16%, 2011-2016 yillarda esa 12% ni tashkil etdi.[29] Xuddi shunday tendentsiya kam vaznli bolalar uchun ham kuzatilishi mumkin. Ushbu tendentsiyalar Mingyillik rivojlanish maqsadlari (MRM) maqsadiga erishish yo'lidagi taraqqiyotni namoyish etadi. Biroq, 2017 yilga kelib 5 yoshgacha bo'lgan bolalar orasida o'sishni pasaytirishni 31 foizgacha va vaznning kamligini 25 foizgacha kamaytirish bo'yicha SDG maqsadini bajarish uchun hali ko'p yo'l bor (Milliy rejalashtirish komissiyasi 2015).[iqtibos kerak ]
Mikro-oziq moddalar etishmovchiligi keng tarqalgan bo'lib, homilador ayollarning deyarli yarmi va besh yoshgacha bo'lgan bolalar, shuningdek reproduktiv yoshdagi ayollarning 35% kamqonlik bilan kasallangan. Bolalarning atigi 24% temirga boy oziq-ovqat iste'mol qiladi, bolalarning 24% minimal qabul qilinadigan parhezni qondiradi va homilador ayollarning faqat yarmi homiladorlik paytida tavsiya etilgan temir qo'shimchasini qabul qiladi. Oziqlanishning yomonlashuviga sabab bo'lgan omil yuqori diareya kasalligi bo'lib, u sanitariya sharoitidan foydalanishning etishmasligi va Nepalda odatdagi ochiq defekatsiya amaliyoti (44%) bilan kuchaygan.[27]
| Shahar hududlari | Qishloq joylar | Umuman olganda | |
|---|---|---|---|
| Bo'shashgan | 27% | 42% | 41% |
| Bekor qilingan | 8% | 11% | 11% |
| Kam vazn | 17% | 30% | 29% |
Geografik cheklovlar
Ko'p qishloq Nepal tog'li yoki tog'li hududlarda joylashgan. Nepalning notekis relyefi va tegishli infratuzilmaning etishmasligi, uni juda qiyin qilib qo'yadi, bu ko'plab qishloq tog'li hududlarida tibbiy yordamni cheklaydi.[30] Ko'pgina qishloqlarda transportning yagona usuli piyoda. Bu davolanishni kechiktirishga olib keladi, bu shoshilinch tibbiy yordamga muhtoj bemorlarga zarar etkazishi mumkin.[31] Nepal sog'liqni saqlash muassasalarining aksariyati shaharlarda to'plangan. Qishloq sog'liqni saqlash muassasalari ko'pincha etarli mablag'ga ega emaslar.[32]
2003 yilda Nepalda qishloqlarga xizmat ko'rsatadigan 10 ta sog'liqni saqlash markazi, 83 ta kasalxona, 700 ta tibbiyot punkti va 3158 ta "pastki tibbiyot punktlari" mavjud edi. Bundan tashqari, ularning soni 1259 kishini tashkil etdi shifokorlar, har 18,400 kishiga bitta.[18] 2000 yilda sog'liqni saqlash masalalari bo'yicha hukumat tomonidan moliyalashtirish kishi boshiga taxminan 2,30 AQSh dollarini tashkil etdi va sog'liqni saqlash xarajatlarining taxminan 70 foizi badallar hisobiga tushdi. Sog'liqni saqlash uchun hukumat tomonidan ajratilgan mablag'lar 2004 yil moliya yili uchun byudjetning 5,1 foizini tashkil etdi va xorijiy donorlar sog'liqni saqlash xarajatlari uchun jami byudjetning taxminan 30 foizini ta'minladilar.[5]
Siyosiy ta'sirlar
Nepal sog'liqni saqlash muammolari asosan uning siyosiy kuchi va resurslari asosan poytaxtda joylashganligi bilan bog'liq, Katmandu, natijada Nepalning boshqa qismlari ijtimoiy jihatdan chetlashtirildi. Qayta tiklash demokratiya 1990 yilda mahalliy institutlarni mustahkamlashga imkon berdi. 1999 yilgi Mahalliy o'zini o'zi boshqarish to'g'risidagi qonun sog'liqni saqlash, ichimlik suvi va qishloq infratuzilmasi kabi asosiy xizmatlarni berishni o'z ichiga olgan, ammo dastur sog'liqni saqlash sohasida sezilarli yaxshilanishlarni ta'minlamagan. Siyosiy iroda etishmasligi tufayli,[33] Nepal to'liq markazsizlashtirishga erisha olmadi, shu bilan siyosiy, ijtimoiy va jismoniy imkoniyatlarini chekladi.[23]
Sog'liqni saqlash holati
O'rtacha umr ko'rish
2010 yilda o'rtacha nepalliklar 65,8 yilgacha yashagan. Oxirgi ma'lumotlarga ko'ra JSSV 2012 yilda nashr etilgan ma'lumotlar, Nepalda umr ko'rish davomiyligi 68 yoshni tashkil etadi. Ikkala jinsdagi tug'ilish umri 2010 va 2012 yillarga nisbatan 6 yilga oshdi. 2012 yilda har ikki jinsdagi sog'lom umr ko'rish umr ko'rish davomiyligidan 9 yilga past bo'ldi tug'ilish paytida. Ushbu yo'qolgan sog'lom hayot davomiyligi kasallik va nogironlik bilan o'tgan yillar davomida yo'qolgan to'liq 9 sog'liqni saqlash yilini anglatadi[11]
Kasallik yuki
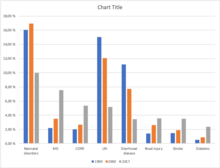
Ga ko'ra Kasalliklarning global yukini o'rganish 2017 yilda Nepalda kasallanish (o'lim) va o'lim (o'lim) ning sakkizta asosiy sabablari quyidagilardir: Neonatal kasalliklar[34] (9.97%), Ishemik yurak kasalligi (7.55%), KOAH (5.35%), Pastki nafas yo'li infektsiyasi (5.15%), Diareya kasalligi (3,42%), yo'l shikastlanishi[35] (3.56%), Qon tomir (3.49%), Qandli diabet (2.35%).[36]
Grafikda ma'lum vaqt oralig'ida Nepalda kasalliklar tarqalishining og'irligi ko'rsatilgan. 1990 yildan 2017 yilgacha bo'lgan davrda neonatal buzuqlik, pastki nafas yo'llari infektsiyasi va diareya kasalliklari tarqalishining bosqichma-bosqich pasayib borishini ko'rsatmoqda. Bunday kamayish sababi hukumat tomonidan sog'liqni saqlash dasturlarini amalga oshirish bilan bog'liq. kabi boshqa xalqaro tashkilotlar JSSV va UNICEF ona va bola salomatligi uchun, chunki bu kasalliklar bolalar orasida juda keng tarqalgan. Shu bilan birga, yurak ishemik kasalligi (IHD), surunkali obstruktiv o'pka kasalligi (KOAH), yo'l shikastlanishi, qon tomir va diabet kabi boshqa kasalliklar sonining sezilarli darajada o'sishi kuzatilmoqda.
Ishemik yurak kasalligi
Ishemik yurak kasalligi (IHD) asta-sekin Nepalda sog'liqni saqlashning asosiy muammolaridan biri sifatida paydo bo'lmoqda. Bu yurak xastaligining eng keng tarqalgan turi va infarkt sababidir. Hayot tarzining tez o'zgarishi, zararli odatlar (chekish, kamharakat turmush tarzi va boshqalar) va iqtisodiy rivojlanish o'sish uchun javobgardir. Kamayganiga qaramay Ishemik yurak kasalligi o'lim rivojlangan mamlakatlar, Nepal kabi rivojlanayotgan mamlakatlarda sezilarli o'sish kuzatildi. IHD past va o'rta daromadli mamlakatlardan, shuningdek yuqori daromadli mamlakatlardan kattalar o'limining birinchi raqamli sababidir. 1990-2020 yillarda rivojlangan mamlakatlarda IHD bilan kasallanish darajasi ayollarda taxminan 29% ga va erkaklarda 48% ga ko'payishi kutilmoqda.
2017 yilda Nepalda jami 182 751 o'lim taxmin qilinmoqda. Yuqumli bo'lmagan kasalliklar (NCD) o'limning asosiy sabablari hisoblanadi - o'limning uchdan ikki qismi (66%) KNK tufayli, qo'shimcha ravishda 9% jarohatlar tufayli. Qolgan 25% yuqumli kasalliklar tufayli, onalik, neonatal va ozuqaviy (CMNN) kasalliklar. Ishemik yurak kasalligi (o'limning 16,4%), Surunkali obstruktiv o'pka kasalligi (KOAH) (umumiy o'limning 9,8%), Diareya kasalliklari (Umumiy o'limning 5,6%), Pastki nafas yo'llarining infektsiyalari (Umumiy o'limning 5,1%), va İntereerebral qon ketish (Jami o'limlarning 3,8%), 2017 yilda o'limning eng yaxshi beshta sababi bo'lgan[37]
Ishemik yurak kasalligi ikkinchi o'rinda turadi kasallik yuki va o'limning asosiy sababi Nepal 2002 yildan 2017 yilgacha IHD tufayli o'lim 100000 kishi boshiga o'limning 65,82 dan 100,45 gacha bo'lgan xavfini ko'paytirmoqda.[38] Shunday qilib, juda ko'p epidemiologik tadqiqotlar Nepalda IHD bilan kasallanish va tarqalishini aniqlash va muammoning kattaligini aniqlash uchun zarur, shunda o'z vaqtida birlamchi va ikkilamchi oldini olish amalga oshirilishi mumkin. Bu juda yuqori darajada oldini olish mumkinligi sababli xavf omili kabi bizning turmush tarzimiz bilan bog'liq; chekish, semirish, nosog'lom ovqatlanish va boshqalar. IHDning oldini olishda ushbu xavf omillari to'g'risida bilim va xabardorlik muhim ahamiyatga ega. Shahid Gangalal nomidagi Milliy yurak markazi Nepalning turli qismida yurak lageri 2008 yil sentyabrdan 2011 yil iyuligacha o'tkazilgan. Yurak kasalligining tarqalishi gipertoniya asosiy qismini talab qiladigan qishloq joylariga qaraganda shaharlarda yuqori bo'lgan. Ulkan ulushi gipertoniya har bir lagerda Nepal yaqin kelajakda IHDning katastrofik ta'sirini oldini olish uchun yurak xastaligining profilaktika dasturlariga ehtiyoj sezmoqda. Shuningdek, ushbu tadqiqotga ko'ra IHD ulushi 0,56% (Tikapur ) 15,12% gacha (Birgunj ) Nepalda.[39]
Ular orasida JSST mintaqasi Evropa mintaqasida, Afrika mintaqasida, Amerika mintaqasida va Sharqiy O'rta er dengizi o'lim darajasi pasayish tendentsiyasida, G'arbiy Tinch okeani, Janubi-Sharqiy Osiyoda esa o'sib bormoqda.
[38] Jadval 1: Nepal, Global va JSSTning 6 mintaqasi o'rtasida yurak ishemik kasalligi sababli 100000 kishi o'limini taqqoslash
| Yil | Global | Nepal | Evropa mintaqasi | Afrika mintaqasi | G'arbiy Tinch okeani mintaqasi | Janubi-Sharqiy Osiyo mintaqasi | Amerika mintaqasi | Sharqiy O'rta er dengizi |
| 1990 | 108,72 | 62,72 | 270,32 | 46,77 | 57,29 | 69,11 | 142,27 | 117,37 |
| 2004 | 108,33 | 69,05 | 278,53 | 45,53 | 77,75 | 74 | 114,73 | 114,51 |
| 2010 | 111,15 | 85,32 | 255,58 | 41,26 | 97,39 | 90,74 | 105,73 | 109,89 |
| 2017 | 116,88 | 100,45 | 245,3 | 39,26 | 115,94 | 103,47 | 111,91 | 112,63 |
Yoshi va jinsiga qarab taqsimlash :
IHD bilan kasallanish 35 yoshdan 45 yoshgacha bo'lgan erkaklarda uchraydi. 65 yoshdan keyin erkaklar va ayollar bilan kasallanish tenglashtirmoqda, ammo IHD bilan kasallangan ayollarning ko'payishi sababli ilgari ko'proq ko'rilganligini ko'rsatadigan dalillar mavjud stress, chekish va menopauza.IHD xavfi yosh oshgani sayin ortadi. O'rta yoshdagi kattalar asosan IHD kasalligiga chalinadi .Erkaklar uchun xavf taxminan 45 yoshdan ko'tarila boshlaydi va 55 yoshga kelib xavf ikki baravar ko'payadi. U 85 yoshga qadar o'sishda davom etmoqda. Ayollar uchun IHD xavfi ham yoshga qarab ko'tariladi, ammo bu tendentsiya erkaklarnikiga qaraganda taxminan 10 yil o'tgach boshlanadi va ayniqsa, menopauza
Sil kasalligi
Sil kasalligi (Nepal: Har doim), dunyodagi eng jiddiy xalq salomatligi muammo yuqumli hisoblanadi bakterial kasallik Bacillus tomonidan kelib chiqqan Mikobakteriya.[40] Eng keng tarqalgan bo'lsa-da Mikobakteriya sil kasalligini keltirib chiqaradigan turlar M. sil kasalligi, Sil kasalligi ham sabab bo'ladi M. bovis va M. africanum va vaqti-vaqti bilan fursatparast Mikobakteriyalar: M. Kansaii, M. malmoense, M. simiae, M. szulgai, M. xenopi, M. avium-intracellulare, M. scrofulacum, va M. chelonei.[41]
Sil kasalligi ning eng keng tarqalgan sababi o'lim bitta tufayli organizm yilda 5 yoshdan katta odamlar orasida kam daromadli mamlakatlar. Bundan tashqari, 80% o'limlar sababli sil kasalligi yosh va o'rta yoshdagi erkaklar va ayollarda uchraydi.[42] The kasallanish Jamiyatdagi kasalliklarga ko'plab omillar ta'sir qilishi mumkin, shu jumladan aholi zichligi, haddan tashqari zichlik darajasi va turmush darajasi va sog'liqni saqlashning umumiy darajasi. Qochqinlar kabi ba'zi guruhlar, OIV yuqtirgan, jismoniy va psixologik stressli odam, qariyalar uyi aholisi va qashshoqlashgan sil kasalligini rivojlanish xavfi yuqori. [43]
Uchinchi maqsad ichida 3.3 Barqaror rivojlanish maqsadlari davlatlar "epidemiyalarini tugatish OITS, sil kasalligi, bezgak va tropik kasalliklar va kurashni e'tiborsiz qoldirdi gepatit, suv bilan yuqadigan kasalliklar va boshqalar yuqumli kasalliklar "Va silning so'nggi strategiyasiga bog'liq bo'lgan maqsadlar quyidagilardir:
- Balg'am smear-musbat sil kasalligining 100% holatlarini aniqlang va ushbu holatlarning kamida 85 foizini davolang.
- 2050 yilgacha sil kasalligini jamoat salomatligi muammosi sifatida bartaraf etish (million aholiga <1 ta holat).[44]
Yilda Nepal, Umumiy aholining 45% tashkil etadi kasallangan sil kasalligi bilan kasallangan bo'lib, ulardan 60% samarali yosh guruhiga kiradi (15-45). Har yili 40 ming odam sil kasalligini rivojlantiradi, ulardan 20 ming nafari yuqumli o'pka kasalligiga chalingan.[45] Sil kasalligi tarqalishi bo'yicha milliy tadqiqot natijalariga ko'ra 2018 yilda 69 ming kishi sil kasalligini rivojlantirgan. Bundan tashqari, Nepalda 117 ming kishi ushbu kasallik bilan kasallangan. [46]
| Yosh guruhi | Erkak (%) | Ayol (%) | % | |
| 10-14 | 0.4 | 0.7 | 0.5 | |
| 15-19 | 8.8 | 15.8 | 10.8 | |
| 20-24 | 16.6 | 20.1 | 17.6 | |
| 25-29 | 15.8 | 10.8 | 14.4 | |
| 30-34 | 9.8 | 14.0 | 11 | |
| 35-39 | 10.6 | 9.3 | 10.3 | |
| 40-44 | 8.4 | 9.7 | 8.7 | |
| 45-49 | 8.2 | 6.5 | 7.7 | |
| 50-54 | 8.7 | 7.5 | 8.3 | |
| 55-59 | 8.1 | 5.4 | 7.3 | |
| 60-64 | 1.1 | 0.4 | 0.9 | |
| 65 va undan yuqori | 0.7 | 0.4 | 0.5 | |
| Eslatib o'tilmagan | 2.0 | 0.0 | 2.0 | |
| Jami | 100 | 100 | 100 |
624 mikroskopiya markazi ro'yxatdan o'tgan, Milliy sil kasalligi bo'yicha ma'lumotnoma laboratoriyalari, Milliy sil kasalligi markazi va GENETUP Nepalda madaniyat va giyohvandlikka moyillikni tekshirish xizmatini ko'rsatmoqda.[48]

Silni nazorat qilish milliy dasturi (NTP) to'g'ridan-to'g'ri kuzatiladigan davolash strategiyasini (DOTS) qo'llaydi. 1995 yilda, Jahon Sog'liqni saqlash tashkiloti DOTS-ni eng arzon narxlardan biri sifatida tavsiya qildi samarali sil kasalligini nazorat qilish uchun mavjud strategiyalar. DOTS - bu dorilarni berish orqali davolash natijalarini yaxshilash strategiyasi bemorlar to'g'ridan-to'g'ri kuzatuv ostida sog'liqni saqlash xodimlari. DOTS sil kasalligini nazorat qilish uchun 100% samarali ekanligi aniqlandi. Nepalda 4323 ga yaqin silni davolash markazlari mavjud.[48] DOTS-ning joriy etilishi o'lim sonini kamaytirgan bo'lsa-da, har yili 5000-7000 kishi o'lishni davom ettiradi.[49]
Silga dori-darmonlarga chidamliligi har yili 1500 ga yaqin (0.84 dan 2.4 gacha) holatlarga to'g'ri keladi. Ammo har yili silga qarshi dori-darmonlarning 350 dan 450 tagacha ko'pligi xabar qilinadi. Shunday qilib, 2016-2021 yillarda NTP strategik rejasida asosiy maqsad 2021 yilgacha 100% sil kasali sil kasalligini tashxislash va ushbu holatlarning kamida 75% ni muvaffaqiyatli davolashdir.[48]
OIV / OITS
Taxminan 40,723 kishilik aholining taxminan 8,1 foizini tashkil etgan bo'lsa, 2013 yilda Nepalda OIV bilan kasallangan 14 yoshdagi yoki undan kichik 3282 bola bor edi. 50 yosh va undan yuqori yoshdagi aholi orasida 3385 ta infektsiya mavjud (jami sonning 8,3%). aholi). Jins bo'yicha erkaklarga infektsiyalarning uchdan ikki qismi (66%) to'g'ri keladi, qolganlarning uchdan bir qismidan ko'prog'i (34%) ayollarga to'g'ri keladi, ularning 92,2% atrofida reproduktiv yosh guruhi 15‐ 49 yil. Umumiy infektsiyaning erkak va ayol jinsiy nisbati 2006 yildagi 2,15 dan 2013 yilda 1,95 gacha kamaydi va 2020 yilga kelib 1,86 bo'lishi kutilmoqda.[50] Nepaldagi epidemiya ukolni giyohvand moddalar iste'molchilari, migrantlar, jinsiy aloqa xodimlari va ularning mijozlari va MSM tomonidan boshqariladi. 2007 yildagi IDUlar o'rtasida Integratsiyalashgan Bio-Behavioral Surveillance Study (IBBS) natijalari. Katmandu, Poxara va Sharq va G'arb Teray shuni ko'rsatadiki, eng yuqori tarqalish darajasi shahar IUlari orasida topilgan, ularning 6,8% dan 34,7% gacha bo'lgan joyiga qarab OIV bilan kasallanganlar. Mutlaq sonlar bo'yicha Nepalning 1,5 milliondan 2 milliongacha mehnat muhojirlari Nepalning OIV bilan kasallangan aholisining aksariyat qismini tashkil qiladi. Bitta kichik guruhda qaytib kelgan migrantlarning 2,8% Mumbay, Hindiston, 2006 yil muhojirlar orasida IBBS ma'lumotlariga ko'ra, OIV bilan kasallangan.[51]
2007 yil holatiga ko'ra, ayol jinsiy aloqa xodimlari va ularning mijozlari orasida OIV tarqalishi mos ravishda 2% va 1% dan kam bo'lib, shaharlik MSM orasida 3,3% ni tashkil etdi. OIV infeksiyasi ayollarga qaraganda erkaklar orasida, shuningdek, shahar va uzoq g'arbiy Nepalda muhojirlar mehnati ko'proq uchraydi. Mehnat muhojirlari Nepalda ma'lum bo'lgan OIV infektsiyasining 41 foizini tashkil qiladi, undan keyin jinsiy aloqa bilan shug'ullanadiganlar (15,5 foiz) va IDU (10,2 foiz) mijozlari.[51]
Diareya kasalliklari
Diareya kasalligi asosan bakterial, virusli yoki parazitar organizmlar tomonidan kelib chiqadigan global o'limning asosiy sabablaridan biridir. Bundan tashqari, boshqa omillarga to'yib ovqatlanmaslik, ifloslangan suv va oziq-ovqat manbalari, hayvonlarning najaslari va yomon gigiena sharoitlari tufayli odamdan yuqish kiradi. Diareya ichak trakti infektsiyasining ko'rsatkichidir, bu bo'shashgan yoki suyuq najasni kuniga uch yoki undan ko'p marta yoki odatdagi o'tishdan ko'proq o'tishi bilan tavsiflanadi. Ushbu kasallikning oldini olish uchun bir qator choralar ko'rish mumkin, shu jumladan ifloslangan suv va oziq-ovqat manbalariga kirish, sovun va suv bilan qo'l yuvish, shaxsiy gigiena va sanitariya, bolani kamida olti oy emizish, emlash Rotavirus va odamlar o'rtasida umumiy xabardorlik. Davolash og'iz orqali regidratsiya tuzi (ORS) eritmasi bilan regidratatsiya orqali amalga oshiriladi, foydalanish rux qo'shimchalari, qattiq suvsizlanish yoki shok holatida tomir ichiga suyuqlik yuborish va ozuqaviy moddalarga boy oziq-ovqat mahsulotlarini etkazib berish, ayniqsa, to'yib ovqatlanmaydigan bolalar uchun.[52]
Kasalliklarning global yukini o'rganish shuni ko'rsatadiki, 2017 yilda Nepalning barcha yosh guruhlari orasida diareya kasalliklari umumiy o'limning 5,91 foizini tashkil qilgan. Shu yili ma'lumotlar 5 yosh guruhida diareya kasalliklari o'limning eng yuqori sababini 9,14 foizga etkazganligini ko'rsatmoqda. -14 yoshdan keyin 70 yoshdan kattalar guruhida 8,91% o'lim.[53]
Tadqiqot mavjudligini ko'rsatdi enteropatogenlar diareya najasining uchdan ikki qismidan ko'prog'ida.[54] Katmanduda o'tkazilgan so'rovnoma mavjudligini ko'rsatdi Giardiya sinovdan o'tgan suv namunalarining 43 foizida kistalar.[55] Xuddi shunday, diareya va dizenteriya kabi bakteriyalarni keltirib chiqaradi Escherichia coli, Shigella turlari, Kampilobakter turlari, Vibrio vabo Nepalning ifloslangan ichimlik suvida ko'proq uchraydi. [56] 2009 yilda katta vabo Jajarkot va unga qo'shni tumanlarda o'ttiz mingga yaqin odam va besh yuzdan ziyod odamning o'limiga duchor bo'lgan kasallik tarqaldi va bu Nepalning turli joylarida uzoq vaqtdan beri keng tarqalgan.[57] Virusli diareya asosan sabab bo'ladi Rotavirus ammo bir nechta holatlar Norovirus va Adenovirus o'rganish turida ham kuzatilgan. [58]
2006, 2011 va 2016 yillarda Nepalning beshta rivojlanish mintaqasida besh yoshgacha bo'lgan bolalar orasida diareya tarqalishi quyidagi jadvalda keltirilgan.
| Rivojlanish mintaqalari | 2006 | 2011 | 2016 | |||
|---|---|---|---|---|---|---|
| Respondentlarning soni yo'q | Tarqalishi% | Respondentlarning soni yo'q | Tarqalishi% | Respondentlarning soni yo'q | Tarqalishi% | |
| Sharqiy | 1217 | 11.83 | 1148 | 11.66 | 902 | 6.33 |
| Markaziy | 1342 | 12.30 | 1066 | 15.02 | 1264 | 9.67 |
| G'arbiy | 1281 | 12.87 | 1159 | 15.63 | 923 | 5.39 |
| O'rta-g'arbiy | 778 | 9.32 | 914 | 14.37 | 1078 | 8.49 |
| Uzoq-g'arbiy | 798 | 12.07 | 741 | 10.94 | 660 | 6.22 |
| Jami | 5416 | 11.99 | 5028 | 13.92 | 4827 | 7.67 |
Onalik va yangi tug'ilgan chaqaloqlarning sog'lig'i
Onalik va neonatal sog'liqni saqlash (MNH) - Sog'liqni saqlash va Nepal aholisi vazirligi (Sog'liqni saqlash vazirligi) ning ustuvor vazifalaridan biri. Biroq, mamlakat hali ham yuqori darajaga ega Onalar o'limi darajasi Hindiston (174), Butan (148), Bangladesh (176), Myanma (178), Pokiston (178) va Shri-Lanka (30) kabi qo'shni Janubiy Osiyo davlatlariga nisbatan (MMR) (100000 tirik tug'ilishga 258). ).[60] So'nggi o'n yil ichida bu ko'rsatkich turg'un bo'lganiga qaramay, 2016 yilda yangi tug'ilgan chaqaloqlarning o'lim darajasi (1000 tirik tug'ilganga 21) 2011 yilda 1000 tirik tug'ilganga 33 taga nisbatan biroz pasayish kuzatildi,[61] mamlakatda. Nepal shuningdek Barqaror rivojlanish maqsadlariga imzo chekmoqda, ular mamlakat uchun 100,000 tirik tug'ilgan chaqaloqqa MMRni 70 ga va yangi tug'ilgan chaqaloqlarning o'limini 1000 tirik tug'ilishga 12 tagacha kamaytirish va 90% qamrab olishga erishish uchun katta maqsadlarni qo'ygan. 2030 yilga qadar to'rtta ANC tashrifi, institutsional etkazib berish, SBA etkazib berish va uchta PNC tekshiruvi.[62]
Nepal 1997 yildan buyon profilaktika va targ'ibot tadbirlari hamda homiladorlik, tug'ruq va tug'ruqdan keyingi davrda o'limga olib keladigan omillarni bartaraf etish orqali onalar va yangi tug'ilgan chaqaloqlarning kasalligi va o'limini kamaytirish, onalar va neonatallarning sog'lig'ini yaxshilashga qaratilgan.[63] Ushbu dasturlarning asosiy strategiyalari tug'ilishga tayyorlik, tug'ruqdan oldin parvarish qilish (ANC) tekshiruvlari, institutsional etkazib berish yoki tug'ruq bo'yicha malakali xizmatchilar (SBA) tomonidan sog'liqni saqlash muassasalarida ham, uyda ham etkazib berishdir. Nepalda AamaSuraksha dasturi (Onalikni rag'batlantirish sxemasi) joriy etildi, bu mamlakatda onalar va neonatal sog'liqni saqlashni rivojlantirishda muhim bosqich bo'lib, u institutsional tug'ilishga intilayotgan ayollar uchun iqtisodiy to'siqlarni kamaytirishga qaratilgan. Ushbu sxema bo'yicha, sog'liqni saqlash muassasasida etkazib beradigan nepal ayollari nepal rupisi (NR) 3000 (tog 'tumanlari), 2000 NRS (tepalik tumanlari) va 1000 NR (Teray tumanlari) naqd rag'batlantiradilar, ularga 800 NRs qo'shiladi. milliy protokol bo'yicha to'rtta ANC tashrifini yakunlagan ayollar. Ushbu dastur pulni rag'batlantirishdan tashqari, bepul institutsional etkazib berish, yangi tug'ilgan chaqaloqlarga muhim yordam va yangi tug'ilgan chaqaloqlarni parvarish qilishni ham ta'minlaydi. MoHP shuningdek, tug'ruqdan keyingi uchta tekshiruvni (PNC) tavsiya qiladi va qishloq joylarida PNC uyiga tashrif buyuradi. Shunga o'xshab, tug'ruq paytida tug'ruq xavfi ostida bo'lgan homilador ayollarni erta aniqlash uchun, MHP shuningdek, 14 ta chekka tumanda qishloq ultratovush tekshiruvini olib boradi va shoshilinch akusherlik va neonatal yordam markazlariga (CEONC) murojaat qiladi.[63]
MHPning Nepalda onalar va neonatal sog'lig'ini yaxshilash bo'yicha yuqorida aytib o'tilgan barcha sa'y-harakatlariga qaramay, bu borada rivojlanish sust bo'lib, 2030 yilga mo'ljallangan maqsadga erishish uchun hali yaxshilanadigan narsalar ko'p. Iqtisodiy, geografik va ijtimoiy-madaniy nomutanosibliklar mamlakatda onalar sog'lig'ini saqlash xizmatlarini takomillashtirishdagi ba'zi to'siqlardir.[64] Qashshoqlikda, chekka hududlarda yashaydigan va kam ma'lumotli ayollar onalikni muhofaza qilish xizmatlaridan kamroq foydalanishadi. Shuning uchun hukumat kam ta'minlangan va marginal ayollarga qaratilgan ko'proq aralashuv va dasturlarni ishlab chiqishi va amalga oshirishi kerak [65]
Jadval: Onalik va neonatal sog'liqni saqlash ko'rsatkichlari tendentsiyalari [61]
| 2011 | 2016 | |
| Neonatal o'lim darajasi / 1000 tirik tug'ilish | 33 | 21 |
| 4 ta ANC tashrifining ulushi (%) | 50 | 69 |
| Institutsional etkazib berish (%) | 35 | 57 |
| SBA etkazib berish | 36 | 58 |
| PNC tashrifi | 45 | 57 |
Og'iz sog'lig'i

Og'zaki sog'liq - bu sog'lom hayot uchun muhim shart. Nepal kabi rivojlanayotgan mamlakatlarda og'iz sog'lig'ini saqlashga urinish juda qiyin vazifadir. Sog'liqni saqlash xizmati departamentining yillik hisobotiga ko'ra (2009/10),[66] 392 831 ta tish kariesi / tish og'rig'i, 73309 kishi periodontal kasalliklar, 62 747 va 113 819 ta og'iz yarasi, shilliq qavat va boshqa tegishli kasalliklar. Ma'lumotlar mamlakat aholisida og'iz sog'lig'i muammolarining yuqori darajada tarqalishini ko'rsatadi. Aholida ushbu kasalliklarning aksariyati qashshoqlik va og'iz sog'lig'i to'g'risida xabardorlikning yo'qligi bilan bog'liq. Ga ko'ra Nepal stomatologiya assotsiatsiyasi jurnali Og'iz orqali sog'liqni saqlash bo'yicha "Pathfinder" so'rovi 2004 yil[67] Maktabda o'qiyotgan o'spirinlarda tish parchalanishining tarqalishi pastroq, bu 12 yoshdan 16 yoshgacha 25,6% ni tashkil qiladi. Bu ftorli tish pastasidan foydalanish va kattalar maktabida o'qish bilan bog'liq bo'lishi mumkin. Biroq, periodontal / tish go'shti kasalliklari o'spirinlarda yuqori bo'lib, 12 yoshdan 13 yoshgacha 62,8%, 15 yoshdan 16 yoshgacha 61% ni tashkil qiladi. Va og'iz orqali saraton kasalligi ko'plab mamlakatlarda 1 000 000 aholiga 1 dan 10 gacha bo'lgan holatlarni tashkil qiladi[68]
Odamlarning aksariyati qashshoqlikda yashayotgan Nepal singari mamlakatlarda sog'liqni saqlash, ta'lim va xabardorlik dasturlaridan foydalanish og'iz sog'lig'ini yaxshilashda katta to'siqlar bo'lgan. Odamlarda chekilgan va tutunsiz tamakini yuqori darajada iste'mol qilish og'iz sog'lig'ining aksariyat muammolari bilan juda bog'liq. Tishlarni kuniga kamida bir marta tozalashning tarqalishi 94,9% ni tashkil etgan bo'lsa, kuniga kamida ikki marta tishlarni tozalash darajasi atigi 9,9% ni tashkil etdi. Ftorli tish pastasidan foydalanish 71,4% orasida kuzatilgan. Qishloq aholisi orasida tishlari ingichka bambuk tayoq bilan yuvilishi mahalliy tilda "Datiwan" deb ataladigan narsa juda keng tarqalgan. Va faqat 3,9% oxirgi 6 oy ichida stomatologik tashrif buyurgan.[69]
Jadval: Og'iz gigienasi bo'yicha amaliyotlarni turli yosh guruhlari o'rtasida taqsimlash
| Yosh guruhlari (yil) | Tishlarni kuniga kamida bir marta tozalash | Tishlarni kuniga kamida ikki marta tozalash | Ftorli tish pastasi | Tishlarga tashriflar (6 oy ichida) |
|---|---|---|---|---|
| 15-29 | 97.9% | 13.1% | 79.3% | 2.8% |
| 30-44 | 94.8% | 8.2% | 69.1% | 4.0% |
| 45-69 | 89.6% | 6.2% | 57.6% | 6.1% |
Nepal hukumati shunga o'xshash muassasalarni himoya qilmaydi JSSV yoki UNICEF og'iz sog'lig'iga ustuvor ahamiyat bermagani uchun boshqa tibbiy masalalar bo'yicha ko'rsatadigan yordamlarini ko'rsatish. Odamlar orasida bir nechta noto'g'ri tushunchalar juda dolzarb bo'lib, yoshi o'tgan sayin tishlarning bo'shashishi odatiy holdir va ba'zi tishlarning yo'qolishi odamlarni o'ldirmaydi. Odamlarning aksariyati davolanish uchun kasallik kuchayganida yoki chidab bo'lmas og'riq keltirganda murojaat qilishadi.
Bolalar salomatligi
Nepal, shuningdek, MRM 4 ga erishish yo'lida, 2015 yilda 1000 tirik tug'ilgan chaqaloqqa 5 yoshgacha bo'lgan bolalar o'limi 35,8 ni tashkil etdi,[70] 1991 yilda 162 dan kam[71] milliy ma'lumotlarga ko'ra. Dunyo miqyosidagi hisob-kitoblarga ko'ra, bu ko'rsatkich 1991 yildan 2013 yilgacha 65 foizga kamaygan, har 1000 tirik tug'ilgan chaqaloqqa 128 dan 48 gacha.[72] Nepal turli xil jamoatchilik va milliy kampaniya yondashuvlari orqali bolalar o'limining eng muhim sabablarini oldini olish yoki davolash bo'yicha samarali choralarni qamrab olishni muvaffaqiyatli takomillashtirdi. Bularga yarim yillik A vitamini qo'shimchasini yuqori darajada qamrab olish va degelmintizatsiya qilish kiradi; CB-IMCI; bolalarni to'liq emlashning yuqori ko'rsatkichlari; va 6 oygacha bo'lgan bolalarni faqat ko'krak suti bilan oziqlantirishni o'rtacha darajada qamrab olish. Biroq, so'nggi bir necha yil ichida YMR to'xtab qolmadi va 2015 yilda 1000 tirik tug'ilgan chaqaloqqa 22,2 o'lim ko'rsatkichi qayd etildi. Bu Hindistonda 27,7 (2015) va Pokistonda 45,5 (2015) bilan solishtirganda.[70]
NMR Nepalda jiddiy tashvish uyg'otmoqda, bu 2015 yilga kelib bolalar o'limi koeffitsientining (IMR) 76 foizini va 5 yoshgacha bo'lgan bolalar o'limining (U5MR) 58 foizini tashkil qiladi va bu uning oldidagi muammolardan biridir.[70] Odatda, mojaro tarixi sog'liqni saqlash ko'rsatkichlariga salbiy ta'sir qiladi. Biroq, Nepal o'n yillik qurolli to'qnashuvlarga qaramay, sog'liqni saqlash ko'rsatkichlarining aksariyati bo'yicha muvaffaqiyatga erishdi. Buni tushunishga urinishlar bir qator mumkin bo'lgan tushuntirishlarni taqdim etdi, shu jumladan aksariyat hollarda sobiq isyonchilar sog'liqni saqlash xizmatlarini ko'rsatishni maqsadli ravishda buzmaganligi; sog'liqni saqlash xodimlariga poliklinikalarda qatnashish va isyonchilar bazasida xizmat ko'rsatish uchun bosim o'tkazildi; ziddiyat asosiy aktyorlar o'rtasida muvofiqlashtirishni yaxshilash uchun muhit yaratdi; va Nepalning sog'liqni saqlash tizimi aholining kam ta'minlangan guruhlari va chekka hududlarga yo'naltirilgan yondashuvlarni, xususan, ayollarning sog'liqni saqlash ko'ngillilari (FCHV), ayollar guruhlari va sog'liqni saqlash muassasalarini operatsion boshqarish qo'mitalari (HFOMC) orqali jamoatchilikni qo'llab-quvvatlashning funktsional tizimi bilan asosiy xizmatlarni ko'rsatishga qaratilgan yondashuvlarni qabul qildi. .[73]
Bolalar salomatligi dasturlari
Sog'liqni saqlash va aholi vazirligining Nepal sog'liqni saqlash bo'limi (MOHP) Nepalda bolalarning sog'lig'ini yaxshilash uchun turli xil operatsion tashabbuslarni o'z ichiga olgan bir nechta bolalar hayotini saqlab qolish tadbirlarini boshladi. Bularga Immunizatsiya bo'yicha Kengaytirilgan Dastur (EPI), Bolalik kasalliklarini jamoatchilik asosida kompleks boshqarish (CB-IMCI) dasturi, Jamiyatga asoslangan yangi tug'ilgan chaqaloqlarni parvarish qilish dasturi (CB-NCP), Chaqaloq va yosh bolalarni oziqlantirish dasturi, mikro - ozuqaviy moddalarni qo'shish dasturi, A vitamini va degelmintizatsiya kampaniyasi va O'tkir ovqatlanishni jamoatchilik asosida boshqarish dasturi.[66]:29
Immunizatsiya
Milliy immunizatsiya dasturi Nepalda birinchi (P1) dastur hisoblanadi. Dastur boshlanganidan beri u universal tarzda o'rnatildi va muvaffaqiyatli amalga oshirildi. Immunizatsiya xizmatlarini shifoxonalarda, boshqa sog'liqni saqlash markazlarida, ko'chma va ko'chma klinikalarda, nodavlat tashkilotlarda va xususiy klinikalarda EPI klinikalaridan bepul olish mumkin. Hukumat kasalxonalar, xususiy muassasalar va qariyalar uylariga barcha vaktsinalar va emlash bilan bog'liq logistika vositalarini harajatsiz ta'minladi. Nepal o'shandan beri dasturning muvaffaqiyati uchun e'tirofga sazovor bo'ldi, chunki uning boyligi, jinsi va yoshidan qat'i nazar, aholining 97 foizini teng ravishda qamrab olish. Biroq, Milliy Immunizatsiya Dasturining keng miqyosli muvaffaqiyatiga qaramay, tengsizliklar baribir mavjud. Shunga qaramay, so'nggi 15 yillik tendentsiyalar immunizatsiya bilan to'liq qamrab olish imkoniyatlarini ko'rsatadigan istiqbolli ijobiy o'zgarishlarni ko'rsatdi.[74] 2014 yildan 2015 yilgacha yana ikkita vaktsina - inaktivatsiyalangan poliomielitga qarshi emlash (IPV) va pnevmokokk konjugat vaktsinasi (PCV) joriy etildi. Nepalning oltita tumani 99,9% emlash bilan qamrab olingan deb e'lon qilindi. Nepal 2014 yil 27 martda poliomiyelitdan xoli bo'lgan maqomga erishdi. Neonatal va onaning qoqshol kasalligi 2005 yilda allaqachon yo'q qilingan va yapon ensefaliti nazorat ostida holatidadir. Nepal ham 2019 yilga qadar qizamiqni yo'q qilish bo'yicha maqsadga erishmoqda.[66]:i, 8 Nepaldagi bolalarning bir foizi hali vaktsinani qamrab olmagan.
Bolalik kasalliklarini jamoatchilik asosida kompleks boshqarish (CB-IMCI)
Bolalik kasalliklarini jamoatchilik asosida kompleks boshqarish (CB-IMCI) dasturi 2 oylikdan 5 yoshgacha bo'lgan bolalar o'rtasida pnevmoniya, diareya, bezgak va qizamiq kabi kasalliklarni hamda to'yib ovqatlanmaslik kabi kasalliklarni davolashga qaratilgan birlashtirilgan to'plamdir. Shuningdek, u infektsiyani davolash, sariqlik, gipertermiya va 2 oylikgacha bo'lgan yosh bolalar uchun emizish bo'yicha maslahatlarni o'z ichiga oladi. CB-IMCI dasturi Nepalning barcha tumanlarida jamoatchilik darajasiga qadar amalga oshirildi va u bolalar kasalliklarini boshqarish bo'yicha ijobiy natijalarni ko'rsatdi. So'nggi o'n yil ichida Nepal asosan CB-IMCI dasturini amalga oshirish hisobiga besh yoshgacha bo'lgan bolalar o'limini kamaytirishda muvaffaqiyat qozondi. Dastlab, diareya kasalliklarini nazorat qilish (CDD) dasturi 1982 yilda boshlangan; va O'tkir nafas yo'li infektsiyalarini nazorat qilish (ARI) dasturi 1987 yilda boshlangan. CDD va ARI dasturlari 1998 yilda CB-IMCI dasturiga birlashtirilgan.[75]
Jamiyatga asoslangan yangi tug'ilgan chaqaloqlarni parvarish qilish dasturi (CB-NCP)
Nepal oilaviy sog'liqni saqlash tadqiqotlari 1996 yil, Nepal demografik va sog'liqni saqlash tadqiqotlari va Jahon Sog'liqni saqlash tashkiloti vaqt o'tishi bilan o'tkazilgan hisob-kitoblar shuni ko'rsatdiki, Nepalda yangi tug'ilgan chaqaloqlarning o'limi bolalar va bolalar o'limiga qaraganda sekinroq pasaymoqda. Nepal Demografik va sog'liqni saqlash tadqiqotlari 2011 yilda 1000 tirik tug'ilgan chaqaloqqa 33 yangi tug'ilgan chaqaloqlarning o'limini ko'rsatdi, bu 5 yoshgacha bo'lganlarning 61 foizini tashkil qiladi. The major causes of neonatal death in Nepal are an infection, birth asphyxia, preterm birth, and hypothermia. Given Nepal's existing health service indicators, it becomes clear that strategies to address neonatal mortality in Nepal must consider the fact that 72% of births take place at home (NDHS 2011).[75]
Therefore, as an urgent step to reduce neonatal mortality, Ministry of Health and Population (MoHP) initiated a new program called 'Community-Based Newborn Care Package' (CB-NCP) based on the 2004 National Neonatal Health Strategy.[75]
National Nutritional Program
The National Nutrition Program under the Department of Health Services has set its ultimate goal as "all Nepali people living with adequate nutrition, food safety and food security for adequate physical, mental and social growth and equitable human capital development and survival" with the mission to improve the overall nutritional status of children, women of childbearing age, pregnant women, and all ages through the control of general malnutrition and the prevention and control of micronutrient deficiency disorders having a broader inter and intra sectoral collaboration and coordination, partnership among different stakeholders and high level of awareness and cooperation of population in general.[76]
Malnutrition remains a serious obstacle to child survival, growth, and development in Nepal. The most common form of malnutrition is protein-energy malnutrition (PEM). Other common forms of malnutrition are iodine, iron, and vitamin A deficiency. These deficiencies often appear together in many cases. Moderately acute and severely acutely malnourished children are more likely to die from common childhood illnesses than those adequately nourished. In addition, malnutrition constitutes a serious threat to young children and is associated with about one-third of child mortality. Major causes of PEM in Nepal is low birth weight of below 2.5 kg due to poor maternal nutrition, inadequate dietary intake, frequent infections, household food insecurity, poor feeding behaviour and poor care & practices leading to an intergenerational cycle of malnutrition.[77]
An analysis of the causes of stunted growth in Nepal reveals that around half is rooted in poor maternal nutrition, and the other half in poor infant and young child nutrition. Around a quarter of babies are born with a low birth weight. As per the findings of Nepal Demographic and Health Survey (NDHS, 2011), 41 percent of children below 5 years of age are stunted. A survey by NDHS and NMICS also showed that 30% of the children are underweight and 11% of children below 5 years are wasted.[66]:241
In order to address under-nutrition problems in young children, the Government of Nepal (GoN) has implemented:
- a) Infant and Young Child Feeding (IYCF)
- b) Control of Protein Energy Malnutrition (PEM)
- c) Control of Iodine Deficiency Disorder (IDD)
- d) Control of Vitamin A Deficiency (VAD)
- e) Control of Iron Deficiency Anaemia (IDA)
- f) Deworming of children aged 1 to 5 years and vitamin A capsule distribution
- g) Community Management of Acute Malnutrition (CMAM)
- h) Hospital-based nutrition management and rehabilitation
The hospital-based nutrition management and rehabilitation program treats severe malnourished children at Out-patient Therapeutic Program (OTP) centres in Health Facilities. As per requirement, the package is linked with the other nutrition programs such as the Child Nutrition Grant, Micronutrient powder (MNP) distribution to young children (6 to 23 months)[66]:22,24 and food distribution in the food insecure areas[iqtibos kerak ].
Infant and Young Child Feeding program
UNICEF and WHO recommended that children be exclusively breastfed (no other liquid, solid food, or plain water) during the first six months of life (WHO/UNICEF, 2002). The nutrition program under the 2004 National Nutrition Policy and Strategy promotes exclusive breastfeeding through the age of 6 months and, thereafter, the introduction of semisolid or solid foods along with continued breast milk until the child is at least age 2. Introducing breast milk substitutes to infants before age 6 months can contribute to breastfeeding failure. Substitutes, such as formula, other kinds of milk and porridge are often watered down and provide too few calories. Furthermore, possible contamination of these substitutes exposes the infant to the risk of illness. Nepal's Breast Milk Substitute Act (2049) of 1992 promotes and protects breastfeeding and regulates the unauthorized or unsolicited sale and distribution of breast milk substitutes.[78]
After six months, a child requires adequate complementary foods for normal growth. Lack of appropriate complementary feeding may lead to malnutrition and frequent illnesses, which in turn may lead to death. However, even with complementary feeding, the child should continue to be breastfed for two years or more.[78]
Practice of exclusive breastfeeding after Normal delivery and C-section
Etarli oziqlanish during infancy is crucial for child survival, optimal growth and development throughout life. It has been postulated that 13% of the current under-five mortality rate could be averted by promoting proper breastfeeding practices, which is seemingly the single most cost effective intervention to reduce child mortality in resource-constrained settings such as in Nepal. Childhood malnutrition and growth faltering affects more than half of children under five in developing countries, and usually starts during infancy, possibly due to improper breastfeeding and mixed feeding practices.[79]
Ga binoan JSSV, exclusive breastfeeding is defined as no other food or drink, not even water, except ona suti (including milk expressed or from a wet nurse) for 6 months of life, but allows the infant to receive ORS, drops and syrups (vitaminlar, minerallar va dorilar ). Exclusive breastfeeding for the first 6 months of life is the recommended way of feeding infants, followed by continued breastfeeding with appropriate complementary foods for up to 2 years or beyond.[80]
As per the study carried out in Paropakar Maternity & Women's Hospital, Thapathali, 2017, the participants of normal delivery had an opportunity to breastfeed within an hour while almost all participants going through C bo'limi were not offered to do so.[80]
The reason for participants to not practice breastfeeding within an hour were mother's sickness, unable to hold the baby due to suture, baby taken away from mother, and less or no production of breast milk soon after surgery to feed the child. In addition, (as shown in table below) 84.7% of normal delivery participants did not feed anything other than breast milk to their babies while 78% of C-sectioned participants fed formula to their babies after they had started breastfeeding.
| Yetkazib berish usullari | Fed anything other than breast milk to baby | Foiz |
| Normal delivery | Ha | 15.33 |
| Yo'q | 84.66 | |
| Jami | 100 | |
| Kesariyalik tug'ruq | Ha | 56 |
| Yo'q | 44 | |
| Jami | 100 |
The participants assumed that formula-fed babies were more likely to gain weight more quickly than breastfed babies. These might be the major increasing drawbacks for the practice of exclusive breastfeeding in Nepal.
The perspective towards breastfeeding is found to be optimistic, believing to the benefits of breastfeeding were not only for a limited period; is always convenient, healthier and cheaper than formula. Exclusive breastfeeding has always been considered as an ideal food for the baby up to six months after birth.
We can say that mode of delivery is significant with initiation of breastfeeding within an hour. This means the practice of exclusive breastfeeding is higher among normal deliveries than C-sections. From analysis of Nepal demographic and health survey, 2011; Two in every three mothers had initiated breastfeeding within one hour of childbirth.[80]
In some cultures including Nepal there is a preference for the introduction of prelacteal feeds. Iqtisodiy status and the mother's education status were significant factors associated with the introduction of prelacteal feeds. The lower socio-economic groups have less access to the expensive prelacteal feeds such as ghee or honey and therefore exclusive breastfeeding is the only option available. This might be a reason for the reported lower prelacteal feeding practice rates amongst the poorest wealth groups in Nepal.[81]
Geriatric health

There are no active and effective policies and programs to mainstream aging population in national, social and political discourse in Nepal. About 9% of the total population accounts for 60+ populations and the number is projected to be around 20% by 2050. The decline in fertility rate and increased life expectancy is the main cause for the increased number of old age people in Nepal.[82] An increase in the number of aged people and availability of no healthcare services in a developing country like Nepal, aging could be a matter of challenge.
Geriatric services
Out of 2.1million elderly people (2011 census), only 3 geriatric specialists are registered to take care of them. Nepal not only lacks geriatric specialists, but geriatric nurses and caregivers are also lacking.[83] There is only one shelter for elderly people run by the government (Pashupatinath Bridrashram) which was established in 1976 as the first residential facility for elders and has the capacity for only 230 elderly people. Official data of Social Welfare Council shows that the total number of old age homes (OAHs) registered as of 2005 was 153. However, most of these homes either do not exist today or operate in very poor condition. Only about twenty homes are currently functional throughout the country.[84] These organizations vary in their organizational status (government, private, NGO, personal charity), capacity, facilities, and the services they provide. Most of them are charity organizations. About 1,500 elders are living in these old-age homes at present.[85]
Government has initiated to provide geriatric care services by formulating certain plans and policies but these could not be effective due to lack of resources. Madrid Plan of Action on Aging (2002), Senior Citizen Policy (2002), National Plan of Action on Aging (2005), Senior Citizen Act (2006) and The senior Citizens regulations (2008) are the initiatives taken by Nepal government. The Sog'liqni saqlash va aholi vazirligi started social service units in 8 hospitals and geriatric wards in 3 hospitals. About 70 registered old age homes are available in the country out of which 11 get government grants.
In March 2012, a residential health care home for elderly people named Health Home Care Nepal with 15 beds was established by private investment. It aims to provide comprehensive holistic package services for needy elderly people. It was the first model care home managed by medical professionals.[86] Old age homes which are giving services for free in Nepal are listed below:
– Sri Sathya Sai Seva organisation
– Siddhi Memorial Foundation Nepal
Geriatric diseases
There is little baseline information on the prevalence of geriatric diseases among the elderly which is an obstacle for health care planning and management. Prevalence of chronic diseases in old age is a common phenomenon. Most of the common geriatric diseases in Nepal o'z ichiga oladi gastrit, artrit, gipertoniya, KOAH, infektsiyalar, eye problems, orqa og'riq, dementia, bosh og'rig'i, diabet, falaj va yurak muammolari.[84]Specific and exact data related to geriatric population is lacking behind as this section is not more concerned as that of child and women health. More research should be conducted from the public level to get the specific data which can give a focussed idea to develop effective health policies for the old people.
The table below shows the status of diseased state of elderly people in a certain number of aged people in Katmandu.
| Major Chronic Health Problem | % (N= 509) |
|---|---|
| High Blood Pressure | 39.7 |
| Qandli diabet | 22.3 |
| Nafas olish kasalliklari | 21.7 |
| Artrit | 16 |
| Back Pain | 14.3 |
| Yurak kasalliklari | 8.3 |
| Liver and Gull Bladder Diseases | 4.7 |
| Bone Fracture | 4.7 |
| Qon tomir | 4.3 |
| Saraton | 0.7 |
source: Socio-Demographic and Health Status of Nepalese Elderly [87]
These are the only data from a specific place in a specific number of people. More research and studies are to be conducted at the national level to know the exact health status of elderly people in Nepal. The government of Nepal should focus its concern in this field so that elderly from Nepal can get some heath benefits. More research should be conducted from the public level to get the specific data which can give a focussed idea to develop effective health policies for the old people.
Yo'l-transport hodisalari
Road traffic injuries are one of the global health burdens, an eighth leading cause of death worldwide. Globally, approximately 1.25 million lives are cut short every year because of a road traffic injuries. Ranging from 20 to 50 million people become victims of non-fatal injuries, with many acquiring a disability for the rest of the life as a result of their injury.[88] In Nepal, a road traffic accident rank eighth among killer causes of disability-adjusted life years and also eighth among premature cause of death after Non-Communicable Diseases and Communicable Diseases.[89]
A substantial problem of road traffic accident with fatalities occurs mainly on highways caused by bus crashes in Nepal. Due to the country's geography, bus accidents mostly happen in the hilly region and along the long-distance route causing 31 percent of fatalities and serious injuries every year.[90] Accidents involving motorcycles, micro-buses, cars etc. highly prevail in the capital city, Kathmandu compared to other cities and lowland areas. The number of Road Traffic Accidents in the capital city was (53.5±14.1) of the number for the entire country.[91] People between 15 and 40 ages are the most affected group followed by those above 50 years and majorities were male making 73 percent of disability-adjusted life years. The number of registered vehicles in Bagmati zonasi was 129,557, a 29.6 percent of the whole nation in fiscal year 2017/2018.[92][91]
The table below shows the trend of fatality per 10000 vehicles between 2005 and 2013.
| Yil | Baxtsiz hodisalar | Halok bo'lganlar | Total Vehicles | Fatality per 10000 transport vositalari |
|---|---|---|---|---|
| 2005-6 | 3894 | 825 | 536443 | 15.38 |
| 2006-7 | 4546 | 953 | 625179 | 15.24 |
| 2007-8 | 6821 | 1131 | 710917 | 15.91 |
| 2008-9 | 8353 | 1356 | 813487 | 16.67 |
| 2009-10 | 11747 | 1734 | 1015271 | 17.08 |
| 2010-11 | 140131 | 1689 | 1175824 | 14.36 |
| 2011-12 | 14291 | 1837 | 1342927 | 13.68 |
| 2012-13 | 13582 | 1816 | 1545988 | 11.75 |
source: Traffic Accidents Record, Traffic Directorate, Nepal Police, 2013.[92]
Ruhiy salomatlik
In terms of the network of mental health facilities, there are 18 outpatient mental health facilities, 3-day treatment facilities, and 17 community-based psychiatric inpatient units available in the country. The majority of the mental health service users are treated in outpatient facilities. Thirty-seven percent of patients are female. The patients admitted to mental hospitals belong primarily to the following two diagnostic groups: Schizophrenia, schizotypal and delusional disorders (34%) and Mood [affective] disorders (21%). On average, patients spend 18.85 days in mental hospitals. All of the patients spent less than one year in the mental hospital during the year of assessment.
Two percent of the training for medical doctors is devoted to mental health, and the same percentage is provided for nurses. One Non Government Organization is running a community mental health service in 7 of the 75 districts in the country. In other districts, community mental health services are not available, as mental health services are not yet integrated into the general health service system.
Even though Nepal's mental health policy was formulated in 1996, there is no mental health legislation as yet. In terms of financing, less than one percent (0.17%) of health care expenditures by the government are directed towards mental health. There is no human right review body to inspect mental health facilities and impose sanctions on those facilities that persistently violate patients' rights.[93]
Mental health is one of the least focused healthcare segment in Nepal. Less focused in terms of awareness and treatment. Now also most of the people choose to visit traditional healers, if it doesn't work psychiatrist will be the second choice. Very less number of psychiatrists and more number of psychiatric cases makes hospital crowded place, providing quality service is challenging.
Only few number of trained psychologists are working either in private clinic or very few in government hospitals. Most of the psychologists are working within Kathmandu Valley only.
There are around 25 private centers providing psychotherapy in Kathmandu. Few of them are listed here.
Shuningdek qarang
Adabiyotlar
- ^ "REBUILDING NEPAL'S HEALTHCARE SYSTEM". Mumkin bo'lgan sog'liq.
- ^ a b v "Health System in Nepal: Challenges and Strategic Options" (PDF). Jahon Sog'liqni saqlash tashkiloti. 2007 yil noyabr.
- ^ Nepali Times Issue #561 (8 July 2011 – 14 July 2011)
- ^ "gapminder world". gapminder.org. Olingan 6 sentyabr 2016.[doimiy o'lik havola ]
- ^ a b Nepal country profile. Kongress kutubxonasi Federal tadqiqot bo'limi (2005 yil noyabr). Ushbu maqola ushbu manbadagi matnni o'z ichiga oladi jamoat mulki.
- ^ HDI 2010 index from article Let's Talk Human Development - Data challenges in estimating the HDI: The cases of Cuba, Palau and the Occupied Palestinian Territory
- ^ "gap minder world". gapminder.org. Arxivlandi asl nusxasi 2009 yil 6 fevralda. Olingan 6 sentyabr 2016.
- ^ "gapminder world". Olingan 6 sentyabr 2016.
- ^ "gapminder world". gapminder.org. Arxivlandi asl nusxasi 2012 yil 25 oktyabrda. Olingan 6 sentyabr 2016.
- ^ "Annual_Report_FY_2071_72" (PDF). dohs.gov.np. Arxivlandi asl nusxasi (PDF) 2018 yil 7 sentyabrda. Olingan 7 sentyabr 2016.
- ^ a b "Nepal: WHO Statistical Profile". kim. Olingan 12 sentyabr 2016.
- ^ "Gapminder Tools". Olingan 9 sentyabr 2018.
- ^ "world bank". gapminder.org. Olingan 7 sentyabr 2016.[doimiy o'lik havola ]
- ^ "Nepal: Country Profile". kim. Olingan 11 sentyabr 2016.
- ^ "gapminder world". gapminder.org. Arxivlandi asl nusxasi 2009 yil 6 fevralda. Olingan 7 sentyabr 2016.
- ^ "gapminder world". gapminder.org. Arxivlandi asl nusxasi 2012 yil 25 oktyabrda. Olingan 7 sentyabr 2016.
- ^ a b "JSSV". Olingan 7 sentyabr 2016.
- ^ a b Nepal Health Profile World Health Organisation data (2010)
- ^ "Health for all". Mening respublikam. Arxivlandi asl nusxasi 2012 yil 9-noyabrda. Olingan 14 noyabr 2012.
- ^ "Nepal". Jahon Sog'liqni saqlash tashkiloti. Olingan 18 mart 2018.
- ^ "HEALTH CARE SERVICES IN NEPAL OFFERING COMPREHENSIVE HEALTH CARE AND EDUCATION TO UNDER-SERVED COMMUNITIES". Karuna-Shechen Humanitarian Projects in the Himalayan Region.
- ^ Beine, David. 2001. "Saano Dumre Revisited: Changing Models of Illness in a Village of Central Nepal
- ^ a b Nepal human development report 2009-State transformation and human development by United Nations Development Programme
- ^ Contributions to Nepalese Studies 28(2): 155-185.
- ^ Beine, David. 2003 yil. Ensnared by AIDS: Cultural Contexts of HIV/AIDS in Nepal. Kathmandu, Nepal: Mandala Book Point.
- ^ Karki, Yagya B.; Agrawal, Gajanand (May 2008). "Effects of Communication Campaigns on the Health Behavior of Women of Reproductive Age in Nepal, Further Analysis of the 2006 Nepal Demographic and Health Survey" (PDF). Macro International Inc. Olingan 14 noyabr 2012.
- ^ a b "Nepal: Nutrition Profile" (PDF). usaid.gov. Olingan 10 sentyabr 2016.
- ^ Nepal Demographic and Health Survey. Nepal: Ministry of Health and Population. 2011 yil.
- ^ a b Nepal Demographic and Health Survey. Nepal: Ministry of Health and Population. 2016 yil.
- ^ International Fund for Agricultural Development (IFAD) retrieved 20 September 2011
- ^ "United Methodist Committee on relief; retrieved on 20 September 2011". Arxivlandi asl nusxasi 2012 yil 24 martda. Olingan 22 sentyabr 2011.
- ^ "Shiba Kumar Rai, Kazuko Hirai, Ayako Abe, Yoshimi Ohno 2002 "Infectious Diseases and Malnutrition Status in Nepal: an Overview"" (PDF). Arxivlandi asl nusxasi (PDF) 2012 yil 2 aprelda. Olingan 22 sentyabr 2011.
- ^ Raj Panta, Krishna PhD. "Decentralization of Corruption and Local Public Service Delivery in Nepal" (PDF). Nepal Rastra banki.
- ^ "Neonatology Conferences 2019 | Perinatology Conferences | Fetal Medicine conferences | Pediatrics conferences 2019 | Neonatal Conferences | Kyoto | Japan". neonatologycongress.pediatricsconferences.com. Olingan 17 sentyabr 2019.
- ^ "Road traffic injuries". www.who.int. Olingan 17 sentyabr 2019.
- ^ "Nepal: Country Profile". vizhub.healthdata.org. Olingan 16 sentyabr 2016.
- ^ "NEPAL BURDEN OF DISEASE 2017" (PDF).
- ^ a b "GBD Compare | IHME Viz Hub". vizhub.healthdata.org. Olingan 19 sentyabr 2019.
- ^ "Current cenario of Heart Diseases in Nepal: At a glance".
- ^ Kochi, Arata (March 1991). "The global tuberculosis situation and the new control strategy of the World Health Organization". Naycha. 72 (1): 1–6. doi:10.1016/0041-3879(91)90017-m. ISSN 0041-3879.
- ^ Cheesbrough, Monica, "Part 2", District Laboratory Practice in Tropical Countries, Kembrij: Kembrij universiteti matbuoti, ISBN 978-0-511-54347-0
- ^ Verma, Sharat Chandra (19 October 2016). "Health Sector Response to HIV in the SAARC Region". SAARC Journal of Tuberculosis, Lung Diseases and HIV/AIDS. 12 (1). doi:10.3126/saarctb.v12i1.15934. ISSN 2091-0959.
- ^ Piot, A. (2008). Implementing the WHO Stop TB Strategy : a Handbook for National Tuberculosis Control Programmes (2-nashr). Jeneva: Jahon sog'liqni saqlash tashkiloti. ISBN 978-92-4-068385-3. OCLC 781292812.
- ^ "Tuberculosis Control Programme". mohp.gov.np. Olingan 27 sentyabr 2020.
- ^ National Tuberculosis Centre (2003). "Annual report (2007/2008)". National Tuberculosis Control Programme Nepal. National Tuberculosis Centre.
- ^ National TB control Centre (29 January 2020). "TB Burden in Nepal". Nepal National TB Prevalence Survey Brief. Nepal hukumati.
- ^ Sah, S K; Verma, S C; Bhattarai, R; Bhandari, K; Bhatta, G K (19 October 2016). "Surveillance of HIV Infection among Patients with Tuberculosis in Nepal". SAARC Journal of Tuberculosis, Lung Diseases and HIV/AIDS. 12 (1): 25–30. doi:10.3126/saarctb.v12i1.15939. ISSN 2091-0959.
- ^ a b v National Tuberculosis Center (2019). National Tuberculosis Program, Annual Report 2018. Nepal hukumati.
- ^ SAARC Tuberculosis and HIV/AIDS centre (2009). "Tuberculosis Control SAARC Region update-2009". Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ "annual health report" (PDF). dohs.gov.np. Arxivlandi asl nusxasi (PDF) 2018 yil 7 sentyabrda. Olingan 11 sentyabr 2016.
- ^ a b "Health Profile: Nepal" (PDF). AQSh Xalqaro taraqqiyot agentligi. Mart 2008. Arxivlangan asl nusxasi (PDF) 2008 yil 17-avgustda. Olingan 25 avgust 2008.
 Ushbu maqola ushbu manbadagi matnni o'z ichiga oladi jamoat mulki.
Ushbu maqola ushbu manbadagi matnni o'z ichiga oladi jamoat mulki. - ^ "Diarrhoeal disease". Jahon Sog'liqni saqlash tashkiloti. Olingan 30 sentyabr 2020.
- ^ "GBD Compare". Olingan 30 sentyabr 2020.
- ^ Ono K, Rai SK, Chikahira M, et al. Seasonal distribution of enteropathogens detected from diarrheal stool and water samples collected in Kathmandu. Nepal. Southeast Asian J Trop Med Public Health. 2001;32:520–526. [PubMed] [Google Scholar]
- ^ Kimura K, Rai SK, Rai G, et al. Study of Cyclospora cayetanensis associated with diarrheal disease in Nepal and Lao DPR. Southeast Asian J Trop Med Public Health. 2005;36:1371–1376. [PubMed]
- ^ A large-scale study of bacterial contamination of drinking water and its public health impact in Nepal.Rai SK, Ono K, Yanagida JI, Ishiyama-Imura S, Kurokawa M, Rai CKNepal Med Coll J. 2012 Sep; 14(3):234-40.[PubMed]
- ^ Pach A, Bhattachan A (2014) Understanding cholera in Nepal (Blog Post, Stop Cholera). https://www.stopcholera.org/blog/understanding-cholera-nepal.
- ^ Detection of diarrheagenic viruses from diarrheal fecal samples collected from children in Kathmandu, Nepal.Kurokawa M, Ono K, Nukina M, Itoh M, Thapa U, Rai SKNepal Med Coll J. 2004 Jun; 6(1):17-23.[PubMed] [Ref list]
- ^ Diarrhea in under Five Year-Old Children in Nepal: A Spatiotemporal Analysis Based on Demographic and Health Survey Data - Scientific Figure on ResearchGate. Mavjud: https://www.researchgate.net/figure/Observed-diarrhea-prevalence-among-children-under-5-years-old-in-development-regions-of_tbl2_340143393 [accessed 1 Oct, 2020]
- ^ Trends in maternal mortality : 1990 to 2015 : estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization,, UNICEF,, United Nations. Iqtisodiy va ijtimoiy masalalar bo'limi. Population Division,, World Bank,. Jeneva, Shveytsariya. ISBN 9789241565141. OCLC 951230114.CS1 maint: qo'shimcha tinish belgilari (havola) CS1 maint: boshqalar (havola)
- ^ a b Népal. Ministry of health and population. Population division. New ERA. Xalqaro ICF. (2017). Nepal demographic and health survey 2016. Sog'liqni saqlash vazirligi. OCLC 1021410146.
- ^ "Barqaror rivojlanish maqsadlari". sdg.npc.gov.np. Olingan 30 sentyabr 2020.
- ^ a b Yillik hisobot. Kathmandu, Nepal: Department of Health Service, Ministry of Health and Population. 2018. p. 86.
- ^ Mehata, Suresh; Paudel, Yuba Raj; Dariang, Maureen; Aryal, Krishna Kumar; Lal, Bibek Kumar; Khanal, Mukti Nath; Thomas, Deborah (20 July 2017). "Trends and Inequalities in Use of Maternal Health Care Services in Nepal: Strategy in the Search for Improvements". BioMed Research International. doi:10.1155/2017/5079234. PMC 5541802. PMID 28808658. Olingan 30 sentyabr 2020.
- ^ Aryal, Krishna Kumar (2019). Maternal Health Care in Nepal: Trends and Determinants. Kathmandu,Nepal: DFID Nepal. xiii bet.
- ^ a b v d e "2013/2014 yillik hisobot" (PDF). Ministry of Health and Population of Nepal, Department of Health Services. 2015 yil yanvar. Olingan 24 yanvar 2017.
- ^ "JNDA : National Pathfinder Survey in Nepal". jnda. Olingan 17 sentyabr 2019.
- ^ "Oral health : oral health in Nepal". dentistryiq. Olingan 16 sentyabr 2019.
- ^ Thapa, P.; Aryal, K. K.; Mehata, S.; Vaidya, A.; Jha, B. K.; Dhimal, M.; Pradhan, S.; Dhakal, P.; Pandit, A.; Pandey, A. R.; Bista, B.; Pokhrel, A. U.; Karki, K. B. (2016). "NCBI : Oral hygiene practice in Nepal". BMC Og'iz sog'lig'i. 16: 105. doi:10.1186/s12903-016-0294-9. PMC 5041565. PMID 27686858.
- ^ a b v "World Development Indicators [online database]. Washington DC: The World Bank; 2015". World Development Indicators [online database]. Olingan 6 sentyabr 2016.
- ^ Nepal fertility, family planning and health survey: (NFHS, 1991). Kathmandu Nepal. 1993 yil.
- ^ "Gapminder Under five mortality from 1991 to 2011". Gapminder. Olingan 6 sentyabr 2015.
- ^ Devkota, Bhimsen (1 December 2010). "Understanding effects of armed conflict on health outcomes: the case of Nepal". Conflict and Health. 4: 20. doi:10.1186/1752-1505-4-20. PMC 3003631. PMID 21122098.
- ^ Kc, Ashish; Nelin, Viktoria; Raaijmakers, Hendrikus; Kim, Hyung Joon; Singh, Chahana; Målqvist, Mats (2017). "Increased immunization coverage addresses the equity gap in Nepal". Jahon sog'liqni saqlash tashkilotining Axborotnomasi. 95 (4): 261–269. doi:10.2471/BLT.16.178327. PMC 5407251. PMID 28479621. Olingan 9 sentyabr 2017.
- ^ a b v "Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population (MoHP), New ERA and ICF International, Calverton, Maryland; 2012" (PDF).
- ^ Multi-sector Nutrition Plan 2013-2017 (2023). http://scalingupnutrition.org/wp-content/uploads/2013/03/Nepal_MSNP_2013-2017.pdf: GOVERNMENT OF NEPAL / National Planning Commission. 2013 yil.CS1 tarmog'i: joylashuvi (havola)
- ^ "A case-control study on risk factors associated with malnutrition in Dolpa district of Nepal". Olingan 11 sentyabr 2016.
- ^ a b Policy - Mother's Milk Substitutes (Control of Sale and Distribution) Act, 2049 (1992). https://extranet.who.int/nutrition/gina/sites/default/files/NPL%201992%20Mother%27s%20Milk%20Substitues%20Control%20of%20sale%20and%20distribution%20Act%202049.pdf.CS1 tarmog'i: joylashuvi (havola)
- ^ Strand, Tor A.; Shrestha, Prakash S.; Mellander, Lotta; Chandyo, Ram K.; Ulak, Manjeswori (January 2012). "Infant feeding practices in Bhaktapur, Nepal: a cross-sectional, health facility-based survey". Xalqaro emizish jurnali. 7 (1): 1–8. doi:10.1186/1746-4358-7-1. ISSN 1746-4358. PMC 3285083. PMID 22230510.
- ^ a b v Sharma, Kashyap Kumar; Aryal, Rachana (25 November 2017). "Comparative Study between the Practices of Exclusive Breastfeeding After Normal Delivery and Cesarean Delivery in Paropakar Maternity and Women's Hospital, Thapathali, Kathmandu Nepal". Advanced Journal of Social Science. 1 (1): 40–52. doi:10.21467/ajss.1.1.40-52. ISSN 2581-3358.
- ^ Khanal, Vishnu; Adhikari, Mandira; Sauer, Kay; Zhao, Yun (8 August 2013). "Factors associated with the introduction of prelacteal feeds in Nepal: findings from the Nepal Demographic and Health Survey 2011". Xalqaro emizish jurnali. 8 (1): 9. doi:10.1186/1746-4358-8-9. ISSN 1746-4358. PMC 3750657. PMID 23924230.
 Ushbu manbadan nusxa ko'chirilgan, u ostida mavjud Attribution 2.0 Generic (CC by 2.0) License.
Ushbu manbadan nusxa ko'chirilgan, u ostida mavjud Attribution 2.0 Generic (CC by 2.0) License. - ^ "Monthly Discussion Forum on Ageing- Annual Report 2018". Olingan 28 avgust 2020.
- ^ "Without specialised care, older adults deprived of basic health care facilities". kathmandupost.com. Olingan 28 avgust 2020.
- ^ a b http://ageingnepal.org/wp-content/uploads/2015/05/OAH-Study-Final.pdf
- ^ USAID Country Health Statistical Report Nepal December 2009. Retrieved on 12 November 2010 form http://pdf.usaid.gov/pdf_docs/PNADR595.pdf
- ^ https://www.ifa-fiv.org/wp-content/uploads/2013/03/IFA-presentation-2014.pdf
- ^ Chalise, Hom Nath. "Socio-Demographic and Health Status of Nepalese Elderly". Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ "Road traffic injuries". Jahon Sog'liqni saqlash tashkiloti. Olingan 9 sentyabr 2018.
- ^ "Nepal | Institute for Health Metrics and Evaluation". www.healthdata.org. 9 sentyabr 2015 yil. Olingan 9 sentyabr 2018.
- ^ "opennepal/datasources" (PDF). GitHub. 6 mart 2018 yil. Olingan 9 sentyabr 2018.
- ^ a b Xuang, Ling; Poudyal, Amod K.; Wang, Nanping; Maharjan, Ramesh K.; Adhikary, Krishna P.; Onta, Sharad R. (1 October 2017). "Burden of road traffic accidents in Nepal by calculating disability-adjusted life years". Oilaviy tibbiyot va jamoat salomatligi. 5 (3): 179–187. doi:10.15212/fmch.2017.0111. ISSN 2305-6983.
- ^ a b "Annual Accidental Description". traffic.nepalpolice.gov.np. Olingan 9 sentyabr 2018.
- ^ "Organization of mental health services in developing countries: Sixteenth Report of the WHO Expert Committee on Mental Health". 1975 yil. doi:10.1037/e409862004-001. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering)
Tashqi havolalar
- Dunyo akusherlik holati - Nepal Country Profile
- Dunyo akusherlik holati - Nepal Country Profile
