Ketogenik parhez - Ketogenic diet
The ketogenik parhez yuqoriyog ', etarlioqsil, kam uglevodli diet tibbiyotda asosan nazorat qilish qiyin bo'lgan (refrakter) davolash uchun ishlatiladi epilepsiya bolalarda. Xun tanani emas, balki yog'larni yoqishga majbur qiladi uglevodlar.
Odatda oziq-ovqat tarkibidagi uglevodlarga aylanadi glyukoza, keyinchalik tanada ko'chiriladi va muhim ahamiyatga ega miya ishini kuchaytirish. Ammo dietada ozgina uglevod qolsa, the jigar konvertatsiya qiladi yog ' ichiga yog 'kislotalari va keton tanasi, ikkinchisi miya va glyukozani energiya manbai sifatida almashtirish. Qonda keton tanasining ko'tarilgan darajasi (holat deyiladi) ketoz ) nihoyat chastotasini pasaytiradi epileptik tutilishlar.[1] Ushbu parhezning biron bir turini tatib ko'rgan epilepsiya bilan kasallangan bolalar va yoshlarning qariyb yarmi tutilishlar sonining kamida yarmiga kamayganini ko'rishdi va parhez bekor qilingandan keyin ham ta'sir davom etmoqda.[2] Ba'zi dalillar shuni ko'rsatadiki, epilepsiya bilan kasallangan kattalar dietadan foyda ko'rishlari mumkin va kamroq qat'iy rejim, masalan o'zgartirilgan Atkins dietasi, xuddi shunday samarali.[1] Yon ta'siri o'z ichiga olishi mumkin ich qotishi, yuqori xolesterin, o'sish sekinlashadi, atsidoz va buyrak toshlari.[3]
Uchun original terapevtik parhez pediatrik epilepsiya tana o'sishi va tiklanishi uchun etarli miqdorda oqsilni va etarli miqdorda beradi kaloriya[Izoh 1] yoshi va bo'yi uchun to'g'ri vaznni saqlash. Klassik terapevtik ketogenik parhez o'tgan asrning 20-yillarida pediatrik epilepsiya kasalligini davolash uchun ishlab chiqilgan va keyingi o'n yillikda keng qo'llanilgan, ammo samarali qo'llanilishi bilan mashhurligi pasaygan. antikonvulsant dorilar. Ushbu klassik ketogenik parhez tarkibida yog'ning og'irligi bo'yicha qo'shilgan oqsil va uglevodga nisbati 4: 1 nisbat mavjud. Bunga kraxmalli meva va sabzavotlar, non, makaron mahsulotlari, don va shakar kabi yuqori uglevodli oziq-ovqat mahsulotlarini chiqarib tashlash, shu bilan birga yong'oq, qaymoq va sariyog 'kabi yog'larga boy oziq-ovqat mahsulotlarini iste'mol qilishni ko'paytirish orqali erishiladi.[1] Parhez yog'ining ko'p qismi uzun zanjirli triglitseridlar (LKT) deb ataladigan molekulalardan iborat. Biroq, o'rta zanjirli triglitseridlar (MCTs) - qisqa muddatli yog 'kislotalaridan tayyorlangan uglerod zanjirlari LCTlardan ko'ra ko'proq ketogenikdir. MCT ketogenik parhez deb nomlanuvchi klassik parhezning bir varianti kokos moyi, MCT-larga boy, taxminan kaloriyalarning yarmini ta'minlash uchun. Ratsionning ushbu variantida umumiy yog 'miqdori kamroq bo'lishiga qarab, uglevodlar va oqsillarning katta qismini iste'mol qilish mumkin, bu esa turli xil ovqatlarni tanlashga imkon beradi.[4][5]
1994 yilda Gollivud prodyuseri Jim Abrahams, kimning o'g'lining og'ir epilepsiya parhez tomonidan samarali nazorat qilingan, dietoterapiya yanada targ'ib qilish uchun Ketogenic Therapies uchun Charlie Foundation yaratdi. Reklama NBC telekanalida ko'rinishni o'z ichiga olgan Ma'lumotlar jadvali dasturi va ... Avval zarari yo'q (1997), a televizor uchun yaratilgan film yulduzcha Meril Strip. Jamg'arma tadqiqot ishiga homiylik qildi, uning natijalari - 1996 yilda e'lon qilingan - dietaga bo'lgan yangi ilmiy qiziqishning boshlanishi.[1]
Ketogenik parhez uchun mumkin bo'lgan terapevtik usullar ko'plab qo'shimcha nevrologik kasalliklar uchun o'rganilgan, ularning ba'zilari quyidagilardan iborat: Altsgeymer kasalligi, amiotrofik lateral skleroz, bosh og'rig'i, neyrotravma, og'riq, Parkinson kasalligi va uyqu buzilishi.[6]
Epilepsiya
Epilepsiya eng keng tarqalganlardan biridir nevrologik keyin buzilishlar O'chokli va qon tomir,[7] butun dunyo bo'ylab taxminan 50 million kishiga ta'sir qiladi.[8] Bu takrorlanadigan, sababsiz odamda aniqlanadi soqchilik. Bu qachon sodir bo'ladi kortikal neyronlar haddan tashqari yong'in, hipersinxron tarzda yoki ikkalasi ham miyaning normal ishlashini vaqtincha buzilishiga olib keladi. Bu, masalan, mushaklar, hislar, ong yoki kombinatsiyaga ta'sir qilishi mumkin. Tutqanoq bo'lishi mumkin markazlashtirilgan (miyaning ma'lum bir qismida cheklangan) yoki umumlashtirilgan (butun miyaga keng tarqalib, ongni yo'qotishiga olib keladi). Epilepsiya turli sabablarga ko'ra yuzaga kelishi mumkin; ba'zi shakllari epileptik deb tasniflangan sindromlar, ularning aksariyati bolalikdan boshlanadi. Ikki yoki uchta bo'lsa, epilepsiya refrakter hisoblanadi (davolanishga olib kelmaydi) antikonvulsant dorilar uni nazorat qila olmadi. Bemorlarning qariyb 60 foizi epilepsiya nazoratini birinchi foydalangan dori vositasida qo'llaydilar, 30 foizga yaqini esa dori vositalari bilan boshqarilmaydi. Giyohvand moddalar ishlamay qolganda, boshqa variantlar ham kiradi epilepsiya jarrohligi, vagus asab stimulyatsiyasi va ketogenik parhez.[7]
Tarix
Ketogenik parhez a asosiy oqim Muvaffaqiyatni ko'paytirish va oddiy bo'lmagan foydalanish cheklovlarini olib tashlash uchun ishlab chiqilgan parhez terapiyasi ro'za epilepsiya kasalligini davolash.[Izoh 2] 1920 va 30-yillarda mashhur bo'lishiga qaramay, u yangi antikonvülsan dori foydasiga tark etildi.[1] Epilepsiya bilan kasallangan odamlarning aksariyati o'zlarining tutilishlarini dori-darmon bilan muvaffaqiyatli nazorat qilishlari mumkin. Shu bilan birga, 25-30% turli xil dorilarni sinab ko'rganiga qaramay, bunday nazoratga erisha olmaydi.[9] Ushbu guruh uchun va ayniqsa bolalar uchun parhez yana bir bor epilepsiya kasalligini boshqarishda muhim rol o'ynadi.[1][10]
Ro'za

Shifokorlar qadimgi Yunoniston bemorlarning ovqatlanishini o'zgartirib, kasalliklarni davolash, shu jumladan epilepsiya. Erta traktat Gippokrat korpusi, Muqaddas kasallik to'g'risida, kasallikni qoplaydi; u kelib chiqadi v. Miloddan avvalgi 400 yil. Uning muallifi epilepsiya kelib chiqishi va davolanishi bo'yicha g'ayritabiiy bo'lgan degan keng tarqalgan fikrga qarshi chiqdi va dietoterapiya oqilona va jismoniy asosga ega edi.[3-eslatma] Xuddi shu to'plamda muallif Epidemiya epilepsiya paydo bo'lganidek tezda davolanadigan, oziq-ovqat va ichimliklardan butunlay voz kechish orqali davolanadigan odamning holatini tasvirlaydi.[4-eslatma] Qirol shifokori Erasistratus "Epilepsiyaga moyil bo'lgan odamni shafqatsiz ro'za tutish va qisqa vaqtga berish kerak" deb e'lon qildi.[5-eslatma] Galen "susaytiruvchi parhez" ga ishongan[6-eslatma] engil holatlarda davolanishga qodir va boshqalarda foydali bo'lishi mumkin.[11]
Epilepsiyani davolash sifatida ro'za tutish bo'yicha birinchi zamonaviy tadqiqot Frantsiyada 1911 yilda o'tkazilgan.[12] Har qanday yoshdagi epilepsiya bilan kasallangan yigirma kishi kaloriya miqdori past bo'lgan vegetarian parhezni iste'mol qilish bilan "zararsizlantirildi" va ochlik davri bilan birlashtirildi. Ikkisi juda katta foyda ko'rdi, ammo aksariyati belgilangan cheklovlarga rioya qilolmadi. Diyet bemorlarning aqliy qobiliyatini yaxshilaydi, ularning dori-darmonlaridan farqli o'laroq, kaliy bromidi, bu aqlni xiralashtirdi.[13]
Shu vaqt atrofida, Bernar Makfadden, amerikalik eksponent jismoniy madaniyat, sog'lig'ini tiklash uchun ro'za tutishni ommalashtirdi. Uning shogirdi osteopatik shifokor Doktor Xyu Uilyam Konklin Battle Creek, Michigan, epilepsiya bilan og'rigan bemorlarni ro'za tutishni tavsiya qilib davolashni boshladi. Konklin epileptik tutilishlar zaharli moddadan ajralib chiqqan toksin natijasida yuzaga kelgan deb taxmin qildi Peyerning yamoqlari ichaklarda, qon oqimiga chiqarildi. U ushbu toksin tarqalishiga imkon berish uchun 18 dan 25 kungacha davom etadigan ro'za tutishni tavsiya qildi. Konklin, ehtimol yuzlab epilepsiya kasallarini o'zining "suvli dietasi" bilan davolagan va bolalarda 90% davolanish darajasi bilan maqtalgan, kattalarda esa 50% gacha tushgan. Keyinchalik Konklin ishi yozuvlarini tahlil qilish shuni ko'rsatdiki, uning bemorlarining 20% xurujlardan xalos bo'lishgan va 50% biroz yaxshilangan.[10]
Konklinning ro'za tutish terapiyasi tomonidan qabul qilingan nevrologlar umumiy amaliyotda. 1916 yilda doktor MakMurrey yozgan Nyu-York tibbiy jurnali 1912 yildan beri epilepsiya bilan og'rigan bemorlarni tez, so'ngra kraxmalsiz va shakarsiz parhez bilan davolaganini da'vo qilmoqda. 1921 yilda endokrinolog Genri Roul Geylin o'z tajribalari haqida hisobot berdi Amerika tibbiyot assotsiatsiyasi anjuman. U Konklinning muvaffaqiyatini o'z qo'li bilan ko'rgan va natijalarni o'zining 36 nafar bemorida takrorlashga urinib ko'rgan. U bemorlarni qisqa vaqt ichida o'rganib chiqqaniga qaramay, shunga o'xshash natijalarga erishdi. 1920-yillarda olib borilgan keyingi tadqiqotlar shuni ko'rsatdiki, tutilishlar odatda ro'za tutgandan keyin qaytadi. Charlz P. Xovlend, Konklinning muvaffaqiyatli bemorlaridan birining ota-onasi va Nyu-Yorkdagi boy korporativ advokat, akasi Jon Elias Xovlendga "ochlik ketozi" ni o'rganish uchun 5000 dollar sovg'a qildi. Pediatriya professori sifatida Jons Xopkins kasalxonasi, Jon E. Xovlend pulni nevrolog tomonidan olib borilgan tadqiqotlarni moliyalashtirishga sarfladi Stenli Kobb va uning yordamchisi Uilyam G. Lennoks.[10]
Parhez
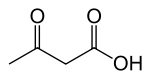
1921 yilda Rollin Tyorner Vudiatt diet va diabet. U uchta suvda eruvchan birikmalar, b-gidroksibutirat, asetoatsetat va aseton (umumiy sifatida tanilgan keton tanasi ), ochlik paytida yoki juda kam uglevodli, yog'li parhezni iste'mol qilganda, sog'lom odamlarda jigar tomonidan ishlab chiqarilgan.[10] Doktor Rassel Morz Uaylder, da Mayo klinikasi, ushbu tadqiqot asosida qurilgan va "ketogenik parhez" atamasi bilan qonda yuqori darajada keton tanalari hosil bo'lgan dietani tavsiflash uchun ishlatilgan (ketonemiya ) ortiqcha yog 'va uglevod etishmovchiligi orqali. Uaylder parhez terapiyasida ro'za tutishning foydasini abadiy saqlab qolish mumkinligiga umid qildi. Uning 1921 yilda bir nechta epilepsiya kasallari ustidan o'tkazgan sinovi ketogenik parhezni epilepsiya davolash usuli sifatida birinchi marta ishlatgan.[10]
Uaylderning hamkasbi, pediatr Myni Gustav Peterman keyinchalik klassik parhezni tuzdi, bolalarda tana vazniga kilogramm vazniga bir gramm protein, kuniga 10-15 g uglevod va yog'dan qolgan kaloriya. 20-asrning 20-yillarida Petermanning ishi dietani induktsiya qilish va saqlash texnikasini yaratdi. Peterman ijobiy ta'sirlarni (ehtiyotkorlik, xulq-atvor va uyquni yaxshilash) va salbiy ta'sirlarni (ortiqcha ketoz tufayli ko'ngil aynish va gijjalar) hujjatlashtirdi. Parhez bolalarda juda muvaffaqiyatli bo'lgan: Peterman 1925 yilda 37 yosh bemorning 95% dietada tutilish nazorati yaxshilanganligi va 60% tutilishsiz bo'lib qolganligi haqida xabar bergan. 1930 yilga kelib, parhez shuningdek 100 o'smir va kattalarda o'rganilgan. Mayo klinikasidan Klifford Jozef Barborka, shuningdek, keksa yoshdagi bemorlarning 56 foizi parhezni yaxshilaganligini va 12 foizi tutqanoqsiz bo'lishini aytdi. Voyaga etganlarning natijalari bolalarning zamonaviy tadqiqotlariga o'xshash bo'lsa-da, ular zamonaviy tadqiqotlar bilan taqqoslanmagan. Barborka kattalar dietadan eng kam foyda olishlari mumkin degan xulosaga kelishdi va kattalarda ketogenik parhezdan foydalanish 1999 yilgacha yana o'rganilmagan.[10][14]
Antikonvülzanlar va pasayish
1920-1930 yillarda, faqat antitonvulsant dorilar sedativ bo'lganida bromidlar (kashf etilgan 1857) va fenobarbital (1912), ketogenik parhez keng qo'llanilgan va o'rganilgan. Bu 1938 yilda o'zgargan X. Xyuston Merritt, kichik va Treysi Putnam topilgan fenitoin (Dilantin) va tadqiqotning yo'nalishi yangi dori-darmonlarni kashf etishga qaratildi. Kirish bilan natriy valproat 1970-yillarda nevrologlar uchun epileptik sindromlar va tutqanoq turlari bo'yicha samarali bo'lgan dorilar mavjud edi. Ketogenik parhezdan foydalanish, bu vaqtga kelib, kabi qiyin holatlarda cheklangan Lennoks-Gastaut sindromi, yana rad etdi.[10]
MCT dietasi

1960-yillarda, o'rta zanjirli triglitseridlar (MCTs) energiya birligiga normal parhez yog'laridan (asosan uzun zanjirli triglitseridlardan) ko'proq keton tanasini ishlab chiqarishi aniqlandi.[15] MKTlar samaraliroq so'riladi va ular orqali tezda jigarga ko'chiriladi jigar portal tizimi o'rniga limfa tizimi.[16] Klassik ketogenik parhezning qattiq uglevod cheklovlari ota-onalarga farzandlari toqat qiladigan mazali taomlarni ishlab chiqarishni qiyinlashtirdi. 1971 yilda, Piter Xuttenloxer ketogenik parhezni ishlab chiqdi, bu erda kaloriyalarning taxminan 60% MCT yog'idan olinadi va bu ko'proq ketogenik parhezga qaraganda ko'proq oqsil va uglevodga uch baravar ko'p bo'lishiga imkon beradi. Yog 'sutining kamida ikki baravaridan ko'pi bilan aralashtirilgan, sovutilgan va ovqat paytida ho'llangan yoki ovqatga qo'shilgan. U buni 12 ta bolalar va o'spirinlarda tutilishi qiyin bo'lgan tutqanoqlarda sinab ko'rdi. Aksariyat bolalar tutishni nazorat qilish va hushyorlikni yaxshilashdi, natijalar klassik ketogenik parhezga o'xshash edi. Oshqozon-ichak traktining buzilishi muammo bo'lib, bitta bemorni dietadan voz kechishga olib keldi, ammo ovqatni tayyorlash osonroq edi va bolalar ularni yaxshi qabul qilishdi.[15] MCT dietasi ko'plab shifoxonalarda klassik ketogenik parhez o'rnini egalladi, ammo ba'zilari ikkalasining kombinatsiyasi bo'lgan dietalarni ishlab chiqdilar.[10]
Uyg'onish
Ketogenik parhez AQShda ommaviy axborot vositalarining ta'siriga 1994 yil oktyabr oyida, NBC bo'lganida erishdi Ma'lumotlar jadvali televidenie dasturida Gollivud prodyuserining o'g'li Charli Abrahamsning ishi haqida xabar berildi Jim Abrahams. Ikki yoshli bola asosiy va muqobil davolash usullari nazoratsiz qolgan epilepsiya kasalligiga chalingan. Abrahams ota-onalar uchun epilepsiya qo'llanmasida ketogenik parhezga oid ma'lumotni topdi va Charliga olib keldi Jon M. Freeman da Jons Xopkins kasalxonasi terapiyani taklif qilishni davom ettirdi. Parhez ostida Charli epilepsiya tez nazoratga olindi va uning rivojlanishi qayta tiklandi. Bu Abrahamsni parhezni targ'ib qilish va tadqiqotlarni moliyalashtirish uchun Charli fondini yaratishga ilhomlantirdi.[10] Ko'p markazli istiqbolli tadqiqotlar 1994 yilda boshlangan, natijalar 1996 yilda Amerika Epilepsiya Jamiyatiga taqdim etilgan va nashr etilgan[17] 1998 yilda. Ratsionga ilmiy qiziqish portlashi kuzatildi. 1997 yilda Abrahams televizion film suratga oldi, ... Avval zarari yo'q, Meril Strip bosh rolni o'ynagan, unda ketogenik parhez yordamida yosh bolakayning epchil epilepsisi muvaffaqiyatli davolanadi.[1]
2007 yilga kelib ketogenik parhez 45 mamlakatda joylashgan 75 ta markazdan mavjud bo'lib, modifikatsiyalangan Atkins dietasi kabi kamroq cheklangan variantlar, ayniqsa katta yoshdagi bolalar va kattalar orasida qo'llanilgan. Ketogenik parhez, shuningdek, epilepsiya kasalligidan tashqari, turli xil kasalliklarni davolash uchun tekshiruvdan o'tkazildi.[1]
Samaradorlik
Ketogenik parhez soqchilik chastotasini uni sinab ko'rgan bemorlarning yarmida 50% dan ko'prog'iga va bemorlarning uchdan birida 90% dan ko'prog'iga kamaytiradi.[18] Bunga javob bergan bolalarning to'rtdan uch qismi buni ikki hafta ichida amalga oshiradilar, ammo mutaxassislar buni samarasiz deb taxmin qilishdan oldin kamida uch oy sinov o'tkazishni maslahat berishadi.[19] Olovga chidamli epilepsiya bilan og'rigan bolalar, boshqa antikonvülzan dori vositasidan ko'ra ketogenik parhezdan ko'proq foyda olishadi.[1] O'smirlar va kattalar parhezdan ham foydalanishlari mumkin, ammo og'iz orqali parhezga rioya qilish (naycha bilan oziqlanadigan) muammo bo'lib qolmoqda.[20]
Sinov dizayni
Dastlabki tadqiqotlar yuqori muvaffaqiyat darajasi haqida xabar bergan; 1925 yilda o'tkazilgan bir tadqiqotda bemorlarning 60% xurujdan xoli bo'lishdi va boshqa 35% bemorlarda soqchilik chastotasi 50% kamaygan. Ushbu tadqiqotlar odatda a kohort yaqinda shifokor tomonidan davolangan bemorlarning (a retrospektiv o'rganish ) va dietada cheklovlarni muvaffaqiyatli saqlab qolgan bemorlarni tanladilar. Biroq, ushbu tadqiqotlarni zamonaviy sinovlar bilan taqqoslash qiyin. Buning bir sababi shundaki, bu eski sinovlar azob chekdi tanlovning noto'g'ri tomoni, chunki ular dietani boshlay olmagan yoki ushlab tura olmagan va shu bilan yaxshi natijalarga erishadigan bemorlar orasidan tanlangan bemorlarni chiqarib tashlashdi. Ushbu noto'g'ri fikrni nazorat qilish uchun zamonaviy o'quv dizayni a ni afzal ko'radi istiqbolli kohort (tadqiqotdagi bemorlar terapiya boshlanishidan oldin tanlanadi), natijada davolanish boshlangan yoki tugaganligidan qat'iy nazar barcha bemorlar uchun natijalar beriladi ( davolash uchun mo'ljallangan tahlil ).[21]
Eski va yangi tadqiqotlar o'rtasidagi yana bir farq shundaki, ketogenik parhez bilan davolangan bemorlarning turi vaqt o'tishi bilan o'zgargan. Dastlab ishlab chiqilgan va ishlatilganida, ketogenik parhez so'nggi davolash usuli emas edi; Aksincha, zamonaviy tadqiqotlar olib borilayotgan bolalar bir qator antikonvulsant dorilarni sinab ko'rishgan va muvaffaqiyatsizlikka uchraganlar, shuning uchun davolash qiyinroq epilepsiya bor deb taxmin qilish mumkin. Dastlabki va zamonaviy tadqiqotlar ham farq qiladi, chunki davolanish protokol o'zgargan. Qadimgi protokollarda diet uzoq vaqt davomida boshlangan tez, 5-10% yo'qotish uchun mo'ljallangan tana vazni va kaloriya iste'molini qattiq cheklab qo'ydi. Bolalarning sog'lig'i va o'sishi bilan bog'liq tashvishlar dietadagi cheklovlarni yumshatishga olib keldi.[21] Suyuqlikni cheklash bir vaqtlar ovqatlanishning o'ziga xos xususiyati edi, ammo bu ich qotishi va buyrak toshlari xavfini oshirdi va endi foydali deb hisoblanmaydi.[18]
Natijalar
Davolash niyatida istiqbolli dizayni bilan olib borilgan tadqiqotlar 1998 yilda bir guruh tomonidan nashr etilgan Jons Xopkins kasalxonasi[22] va undan keyin 2001 yilda chop etilgan hisobot.[23] Ketogenik parhez bo'yicha ko'plab tadqiqotlar singari, yo'q nazorat guruhi (davolashni olmagan bemorlar) ishlatilgan. Tadqiqotda 150 nafar bola ro'yxatdan o'tgan. Uch oydan keyin ularning 83 foizi dietada bo'lishdi, 26 foizida tutilishning yaxshi pasayishi kuzatildi, 31 foizida juda yaxshi pasayish kuzatildi va 3 foizida tutilish yo'q.[7-eslatma] 12 oy ichida 55% dietada edi, 23% yaxshi javob berdi, 20% juda yaxshi javob berdi va 7% tutqanoqsiz. Ushbu bosqichga qadar parhezni bekor qilganlar buni samarasiz, o'ta cheklovchi yoki kasalligi sababli qildilar va qolganlarning aksariyati undan foydalandilar. Ikki, uch va to'rt yoshdagi dietada davom etayotganlarning ulushi mos ravishda 39%, 20% va 12% ni tashkil etdi. Ushbu davrda, parhezni to'xtatishning eng keng tarqalgan sababi, bolalar tutilishsiz yoki sezilarli darajada yaxshilanganligi edi. To'rt yil ichida 150 nafar dastlabki bolalarning 16 foizida tutilish chastotasi yaxshi pasaygan, 14 foizi juda yaxshi pasaygan va 13 foizi tutilishsiz edi, ammo bu raqamlarga dietada bo'lmagan ko'plab odamlar kiradi. Ushbu davomiylikdan keyin parhezda qolganlar odatda tutilishsiz emas, ammo juda yaxshi javob berishgan.[23][24]
Bir nechta kichik tadqiqotlar natijalarini har bir tadqiqotdan ko'ra kuchliroq dalillarni yaratish uchun birlashtirish mumkin - bu statistik usul meta-tahlil. 2006 yilda o'tkazilgan to'rtta shunday tahlillardan biri, jami 1084 bemorga nisbatan 19 ta tadqiqotni ko'rib chiqdi.[25] Xulosa qilishicha, uchdan biri soqchilik chastotasini mukammal pasayishiga va bemorlarning yarmi yaxshi pasayishga erishgan.[18]
A Kokran 2018 yilda o'tkazilgan tizimli tekshiruv epilepsiya bilan og'rigan odamlarda ketogenik parhezning o'n bitta randomizatsiyalangan nazorat ostida tekshiruvlarini topdi va tahlil qildi, ular uchun dorilar ularning tutilishlarini nazorat qila olmadi.[2] Sinovlarning oltitasi ketogenik parhezga tayinlangan guruhni boshqasiga tayinlanmagan guruh bilan taqqosladi. Boshqa sinovlarda parhez turlari yoki ularni yanada toqatli qilish uchun ularni kiritish usullari taqqoslangan.[2] Ketogenik parhezni dietadan tashqari nazorat bilan eng katta sinovida,[16] bolalar va yoshlarning qariyb 38 foizida parhez bilan tutilishning yarim yoki undan kam qismi kuzatilgan, dietaga tayinlanmagan guruh bilan solishtirganda 6 foiz. O'zgartirilgan Atkins Diet-ning dietadan tashqari nazoratga nisbatan ikkita katta sinovi shunga o'xshash natijalarga olib keldi, bolalarning 50% dan ortig'i parhez bilan yarim yoki undan kam tutilishlarga ega, nazorat guruhidagi 10% ga nisbatan.[2]
2018-dagi muntazam tekshiruv kattalardagi ketogenik parhez bo'yicha 16 ta tadqiqotni ko'rib chiqdi. Xulosa shuki, davolanish ushbu bemorlar guruhi uchun tobora ommalashib bormoqda, kattalardagi samaradorlik bolalarga o'xshaydi, yon ta'siri esa nisbatan yumshoq. Biroq, ko'plab bemorlar turli sabablarga ko'ra parhezdan voz kechishdi va dalillarning sifati bolalar bo'yicha olib borilgan tadqiqotlardan past edi. Sog'liqni saqlash muammolari yuqori darajalarni o'z ichiga oladi past zichlikdagi lipoprotein, jami yuqori xolesterin va Ozish.[26]
Ko'rsatkichlar va kontrendikatsiyalar
Ketogenik parhez bolalar va yosh bolalarda qo'shimcha (qo'shimcha) davolash sifatida ko'rsatilgan dorilarga chidamli epilepsiya.[28][29] U milliy tomonidan tasdiqlangan klinik ko'rsatmalar Shotlandiyada,[29] Angliya va Uels[28] va AQShning deyarli barcha sug'urta kompaniyalari tomonidan qoplanadi.[30] Fokusli bolalar jarohat (epilepsiya kasalligini keltirib chiqaradigan miya anormalligining yagona nuqtasi) jarrohlik ketogenik parhezga qaraganda jarrohlik yo'li bilan tutilishsiz bo'lish ehtimoli ko'proq.[19][31] Ketogenik parhezni taklif qiladigan epilepsiya markazlarining taxminan uchdan bir qismi kattalarga parhez terapiyasini taklif qiladi. Oziq-ovqat mahsulotlarining cheklangan ikkita varianti - past glisemik indeks davolash va o'zgartirilgan Atkins dietasi - o'spirinlar va kattalar uchun ko'proq mos keladi, asosan yaxshi rioya qilish tufayli.[19] Ketogenik parhezning suyuq shakli, ayniqsa, uni tayyorlash oson va sut aralashmasidagi chaqaloqlar va boshqalar tomonidan yaxshi muhosaba qilinadi. naycha bilan oziqlangan.[5][32][19]
Xun himoyachilari, ikkita dori muvaffaqiyatsiz tugagandan so'ng, uni jiddiy ko'rib chiqishni tavsiya etadilar, chunki boshqa dorilarning muvaffaqiyatga erishish ehtimoli atigi 10% ni tashkil qiladi.[19][33][34] Xun ba'zi bir epilepsiya va genetik sindromlar uchun ayniqsa foydaliroq bo'lgan joylarda tavsiya etiladi. Bunga quyidagilar kiradi Dravet sindromi, bolalar spazmlari, miyoklonik-astatik epilepsiya, tuberoz skleroz kompleksi va oziqlanadigan bolalar uchun gastrostomiya naychasi.[19][35]
2005 yilda AQShdagi 88 bolalar nevropatologlari o'rtasida o'tkazilgan so'rov natijalariga ko'ra, 36% uch yoki undan ko'p dori ishlamay qolgandan keyin parhezni muntazam ravishda buyurgan, 24% vaqti-vaqti bilan dietani oxirgi chora sifatida belgilagan, 24% esa kamdan-kam holatlarda dietani buyurgan. , va 16% hech qachon dietani buyurmagan. Ushbu bo'shliq uchun bir nechta mumkin bo'lgan tushuntirishlar mavjud dalil va klinik amaliyot.[36] Etarli darajada tayyorgarlikning etishmasligi asosiy omillardan biri bo'lishi mumkin dietologlar ketogenik parhez dasturini boshqarish uchun zarur bo'lganlar.[33]
Ketogenik parhez organizmdagi metabolizmni o'zgartirganligi sababli, bu a birinchi darajali terapiya aniq bo'lgan bolalarda tug'ma metabolik kasalliklar kabi piruvat dehidrogenaza (E1) etishmovchiligi va glyukoza tashuvchisi 1 etishmovchilik sindromi,[37] organizmning uglevodlarni yoqilg'i sifatida ishlatishiga to'sqinlik qiladigan, bu keton tanalariga bog'liqlikka olib keladi. Ketogenik parhez ushbu kasalliklarda tutilishlarni va boshqa alomatlarni davolashda foydalidir va bu mutlaq ko'rsatkichdir.[38] Biroq, bu mutlaqo kontrendikedir kabi boshqa kasalliklarni davolashda piruvat karboksilaza etishmovchiligi, porfiriya va boshqa noyob yog 'almashinuvining irsiy kasalliklari.[19] Yog 'kislotasi oksidlanishining buzilishi bo'lgan odamlar dietada asosiy energiya manbai bo'lgan uglevodlarni almashtiradigan yog' kislotalarini metabolizm qila olmaydi. Ketogenik parhezda ularning tanasi yonilg'i uchun o'zlarining oqsil do'konlarini iste'mol qilishadi, natijada ketoasidoz va oxir-oqibat koma va o'lim.[39]
O'zaro aloqalar
Ketogenik parhez odatda bemorning mavjud antikonvulsant rejimi bilan birgalikda boshlanadi, ammo parhez muvaffaqiyatli bo'lsa, bemorlar antikonvulsantlardan ajratilishi mumkin. Sinergetik foyda keltiradigan ba'zi bir dalillar, dieta bilan birlashganda ko'rinadi vagus asab stimulyatori yoki dori bilan zonisamid va dietani qabul qiladigan bolalarda unchalik muvaffaqiyatli bo'lmasligi mumkin fenobarbital.[18]
Yomon ta'sir
Ketogenik parhez a deb hisoblanmaydi benign, yaxlit yoki tabiiy davolash. Har qanday jiddiy tibbiy terapiyada bo'lgani kabi, bu asoratlarni keltirib chiqarishi mumkin, garchi ular antikonvülzan dori yoki jarrohlik amaliyotiga qaraganda kamroq og'irroq va kamroq bo'lsa.[30] Umumiy, ammo osonlikcha davolash mumkin bo'lgan qisqa muddatli yon ta'sirlarni o'z ichiga oladi ich qotishi, past navli atsidoz va gipoglikemiya agar dastlabki ro'za tutilsa. Qonda lipidlarning ko'tarilgan darajasi bolalarning 60 foizigacha ta'sir qiladi[40] va xolesterin darajasi oshishi mumkin 30% atrofida.[30] Bunga dietadagi yog 'tarkibidagi o'zgarishlar, masalan, to'yingan yog'lardan ko'p to'yinmagan yog'larga qarab va doimiy bo'lsa, ketogenik nisbatni pasaytirish orqali davolash mumkin.[40] Ko'pchilikning parhez etishmasligiga qarshi kurashish uchun qo'shimchalar zarur mikroelementlar.[18]
Bolalarda ketogenik parhezni uzoq vaqt davomida qo'llash o'sishning sekinlashishi yoki to'xtab qolishi, suyak sinishi va buyrak toshlari.[18] Ovqatlanish darajasi insulinga o'xshash o'sish omili 1, bu bolalik o'sishi uchun muhimdir. Ko'p antikonvulsant dorilar singari, ketogenik parhez suyak sog'lig'iga salbiy ta'sir ko'rsatadi. Asidoz va o'sishni to'xtatish gormoni kabi ko'plab omillar ishtirok etishi mumkin.[40] Ketogenik parhezda bo'lgan har 20 boladan bittasida buyrak toshlari rivojlanadi (umumiy aholi uchun bir necha mingdan biriga nisbatan). Deb nomlanuvchi antikonvulsantlar sinfi karbonat angidraz inhibitörleri (topiramat, zonisamid ) buyrakda tosh paydo bo'lish xavfini oshirishi ma'lum, ammo bu antikonvulsantlar va ketogenik parhezning kombinatsiyasi faqatgina dietadan yuqori xavf tug'dirmaydi.[41] Toshlar davolanadi va parhezni to'xtatish uchun asos bo'lmaydi.[41] Klinikalarning yarmiga yaqini og'iz orqali ishlaydi kaliy sitrat qo'shimchalar empirik tarzda barcha ketogenik parhezli bemorlarga, bu tosh shakllanishini kamaytiradigan ba'zi dalillar bilan. Biroq, bo'lajak nazorat ostida sinovdan o'tkazilmagan.[19] Buyrak toshining hosil bo'lishi (nefrolitiyaz) to'rt sababga ko'ra ovqatlanish bilan bog'liq:[41]
- Siydikdagi ortiqcha kaltsiy (giperkalsiyuriya ) atsidoz bilan suyak demineralizatsiyasining kuchayishi tufayli yuzaga keladi. Suyaklar asosan tarkib topgan kaltsiy fosfat. Fosfat kislota bilan reaksiyaga kirishadi va kaltsiy buyraklar orqali chiqariladi.[41]
- Gipotsitraturiya: siydikda sitratning g'ayritabiiy past konsentratsiyasi bor, bu odatda erkin kaltsiyni eritib yuborishga yordam beradi.[41]
- Siydikning past pH qiymati bor, u to'xtaydi siydik kislotasi eriydigan, a rolini o'ynaydigan kristallarga olib keladigan nidus kaltsiy toshining hosil bo'lishi uchun.[41]
- Ko'pgina muassasalar an'anaviy ravishda dietada bemorlarning suv iste'molini odatdagi kundalik ehtiyojlarning 80% gacha cheklashdi;[41] bu amaliyot endi rag'batlantirilmaydi.[18]
O'smir va kattalarda tez-tez uchraydigan nojo'ya ta'sirlarga vazn yo'qotish, ich qotish, dislipidemiya va ayollarda, dismenoreya.[42]
Amalga oshirish
Ketogenik parhez a tibbiy ovqatlanish terapiyasi bu turli fanlarning ishtirokchilarini o'z ichiga oladi. Jamoa a'zolari ro'yxatdan o'tgan pediatrni o'z ichiga oladi parhezshunos parhez dasturini kim muvofiqlashtiradi; pediatrik nevrolog ketogenik parhezni taklif qilishda kim tajribali; va a ro'yxatdan o'tgan hamshira bolalik epilepsiya bilan tanish bo'lgan. Qo'shimcha yordam a dan kelishi mumkin tibbiy ijtimoiy xodim oila bilan ishlaydigan va a farmatsevt dori-darmonlarning uglevod miqdori bo'yicha kim maslahat berishi mumkin. Va nihoyat, parhezni xavfsiz amalga oshirish uchun ota-onalar va boshqa tarbiyachilar dietaning ko'p jihatlari bo'yicha ma'lumot olishlari kerak.[5]
Ovqatni o'lchash va rejalashtirish bilan bog'liq vaqt ajratilganligi sababli parhezni amalga oshirish parvarish qiluvchilar va bemor uchun qiyinchiliklar tug'dirishi mumkin. Rejadan tashqari har qanday ovqatlanish zarur bo'lgan ovqatlanish muvozanatini buzishi mumkinligi sababli, ba'zi odamlar dietani saqlash uchun zarur bo'lgan tartibni qiyin va yoqimsiz deb bilishadi. Ba'zi odamlar dietani bekor qiladilar yoki ozgina talabga javob beradigan parhezga o'tadilar, masalan, o'zgartirilgan Atkins dietasi yoki past glisemik indeksni davolash dietasi, chunki ular qiyinchiliklarni juda katta deb hisoblashadi.[43]
Boshlash
Klassik ketogenik parhezni boshlash uchun Jons Xopkins kasalxonasi protokoli keng qabul qilingan.[44] Bu bemor va ularning yordamchilari bilan maslahatlashishni va keyinroq kasalxonaga qisqa vaqt ichida yotishni o'z ichiga oladi.[21] Ketogenik parhezni boshlash paytida asoratlar xavfi tufayli, aksariyat markazlar parhezni kasalxonada tibbiyot nazorati ostida boshlaydilar.[19]
Dastlabki konsultatsiya vaqtida bemorlar ekranlangan mumkin bo'lgan shartlar uchun qarshi parhez. Ovqatlanish tarix olinadi va parhez parametrlari tanlanadi: yog'ning ketogenik nisbati, aralash protein va uglevodga nisbati, kaloriya talablari va suyuqlikni iste'mol qilish.[21]
Kasalxonaga yotqizilishidan bir kun oldin, dietada uglevodlarning ulushi kamayishi mumkin va bemor kechki ovqatdan keyin ro'za tutishni boshlaydi.[21] Qabulda faqat kaloriya va kofeinsiz suyuqlik[39] dan iborat kechki ovqatgacha ruxsat beriladi.tuxum tuxumi "[8-eslatma] ovqatlanish uchun odatdagi kaloriyalarning uchdan bir qismi bilan cheklangan. Keyingi nonushta va tushlik shunga o'xshashdir, ikkinchi kuni esa "tuxumli" kechki ovqat odatdagi ovqatning kaloriya miqdorining uchdan ikki qismiga ko'paytiriladi. Uchinchi kunga kelib, kechki ovqat to'liq kaloriya kvotasini o'z ichiga oladi va odatdagi ketogenik taom hisoblanadi ("tuxum" emas). To'rtinchi kuni ketogenik nonushta qilgandan so'ng, bemor bo'shatiladi. Iloji bo'lsa, bemorning hozirgi dori-darmonlari uglevodsiz formulalarga o'tkaziladi.[21]
Kasalxonada, glyukoza darajasi har kuni bir necha marta tekshiriladi va bemorga simptomatik belgilar kuzatiladi ketoz (uni oz miqdordagi apelsin sharbati bilan davolash mumkin). Energiya etishmovchiligi va sustlik tez-tez uchraydi, ammo ikki hafta ichida yo'qoladi.[17] Ota-onalar dastlabki uch kun ichida ovqatlanish, parhezni boshqarish, ovqat tayyorlash, shakarni iste'mol qilish va kasallik bilan shug'ullanish kabi darslarga qatnashadilar.[21] Ota-onalarning ta'lim darajasi va majburiyatlari dori-darmonlarga qaraganda yuqori.[45]
Jons Xopkins protokolining o'zgarishi keng tarqalgan. Boshlanish yordamida amalga oshirilishi mumkin ambulatoriya kasalxonada qolishni talab qilishdan ko'ra, klinikalar. Ko'pincha, dastlabki ro'za ishlatilmaydi (ro'za tutish xavfini oshiradi atsidoz, gipoglikemiya va vazn yo'qotish). Uch kunlik ovqatlanish paytida ovqatlanish hajmini oshirish o'rniga, ba'zi muassasalar ovqatlanish hajmini saqlab qolishadi, ammo ketogenik nisbatni 2: 1 dan 4: 1 gacha o'zgartiradilar.[19]
Bemorlarga foyda keltiradigan bemorlarning yarmi tutishni besh kun ichida kamaytirishga erishadilar (agar parhez dastlabki bir-ikki kunlik ro'za bilan boshlanadigan bo'lsa), to'rtdan uch qismi ikki hafta ichida kamayadi va 90% 23 kun ichida kamayadi. Agar parhez ro'za bilan boshlanmasa, bemorlarning yarmi yaxshilanishga erishish vaqti (ikki hafta) uzoqroq, ammo tutilishning uzoq muddatli pasayish darajasi ta'sir qilmaydi.[45] Ota-onalar samaradorligi to'g'risida yakuniy ko'rib chiqishdan oldin kamida uch oy davomida parhezni saqlashga da'vat etiladi.[19]
Texnik xizmat
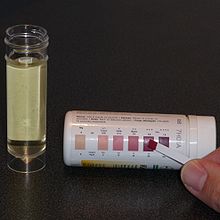
Boshlanishidan keyin bola parhezshunos va nevropatolog tomonidan ko'riladigan kasalxonadagi ambulatoriya-poliklinikaga muntazam ravishda tashrif buyuradi va turli xil tekshiruvlar va tekshiruvlar o'tkaziladi. Ular birinchi yilda har uch oyda, so'ngra olti oyda bir marta o'tkaziladi. Bir yoshgacha bo'lgan bolalar tez-tez uchraydi, dastlabki tashrif atigi ikki-to'rt hafta o'tgach amalga oshiriladi.[46] Ketozning doimiy saqlanib turishini ta'minlash va ovqatlanish rejalarini bemorga yaxshiroq moslashtirish uchun kichik tuzatishlar davri zarur. Ushbu nozik sozlash odatda kasalxona bilan telefon orqali amalga oshiriladi parhezshunos[21] va kaloriyalar sonini o'zgartirish, ketogenik nisbatni o'zgartirish yoki ba'zi bir MCT yoki kokos moylarini klassik parhezga qo'shishni o'z ichiga oladi.[18] Siydik keton darajasi ketozga erishilganligini aniqlash va bemorning parhezga rioya qilishini tasdiqlash uchun har kuni tekshiriladi, ammo ketonlar darajasi antikonvulsant ta'siriga bog'liq emas.[21] Bu tarkibida ketonli test chiziqlari yordamida amalga oshiriladi nitroprussid, bu atsetoasetat (uchta keton tanasidan biri) ishtirokida rangni pushti pushtidan maroonga o'zgartiradi.[47]
Qisqa muddatli soqchilik chastotasining ko'payishi kasallik paytida yoki paydo bo'lishi mumkin keton darajalari o'zgarib turadi. Agar soqchilik chastotasi yuqori bo'lib qolsa yoki bola ozib qolsa, parhez o'zgartirilishi mumkin.[21] Qabul qilishni nazorat qilishni yo'qotish kutilmagan manbalardan kelib chiqishi mumkin. Hatto "shakarsiz" ovqat tarkibida uglevodlar bo'lishi mumkin maltodekstrin, sorbitol, kraxmal va fruktoza. Quyosh nurlari uchun loson va boshqa terini parvarish qiluvchi vositalarning sorbitol tarkibi etarlicha yuqori bo'lishi mumkin, ba'zilari teriga singib ketishi va shu bilan ketozni inkor qilishi mumkin.[33]
To'xtatish
Ketogenik parhez bilan shug'ullanadigan bolalarning taxminan 20% xurujlardan xalos bo'lishadi va ko'pchilik antikonvülzan dori foydalanishni kamaytirishga yoki ularni butunlay yo'q qilishga qodir.[18] Odatda, dietada taxminan ikki yil davomida yoki olti oy tutilmasdan, dieta ikki yoki uch oy davomida asta-sekin bekor qilinishi mumkin. Bu siydik ketozi aniqlanmaguncha ketogenik nisbatni pasaytirib, so'ngra barcha kaloriya cheklovlarini bekor qilish orqali amalga oshiriladi.[48] Ushbu muddat va to'xtatish usuli bolada tutilishsiz bo'lib qolgan bolalarda antikonvulsant dori terapiyasini taqlid qiladi. Ba'zi metabolik kasalliklarni davolash uchun parhez zarur bo'lganda, davomiyligi uzoqroq bo'ladi. Ovqatlanishning umumiy davomiyligi davolovchi ketogenik parhez guruhi va ota-onalarga to'g'ri keladi; 12 yilgacha bo'lgan muddatlar o'rganilib, foydali deb topildi.[46]
Tutqanoq erkinligini qo'lga kiritgandan so'ng parhezni to'xtatgan bolalarda tutilishning qaytish xavfi taxminan 20% ni tashkil qiladi. Takrorlanishgacha bo'lgan vaqt juda o'zgaruvchan, ammo o'rtacha ikki yil. Bunday takrorlanish xavfi rezektsion jarrohlik uchun 10% (miyaning bir qismi olib tashlangan joyda) va antikonvulsant terapiya uchun 30-50% bilan taqqoslanadi. Qayta takrorlanadiganlarning yarmidan ko'prog'i konvulsiyadan yoki ketogenik parhezga qaytib, soqchilikdan xalos bo'lishlari mumkin. Qayta tiklanish ehtimoli, agar soqchilik erkinligiga qaramay, an elektroansefalogramma miyadagi epileptik faollikni ko'rsatadigan, ammo tutqanoqni keltirib chiqaradigan darajadan past bo'lgan epileptiform boshoqlarni ko'rsatadi. Qaytalanish, ehtimol, agar MRI tekshiruvi fokal anormalliklarni ko'rsatadi (masalan, bolalarda bo'lgani kabi tuberoz skleroz ). Bunday bolalar dietada o'rtacha ko'rsatkichdan uzoqroq turishi mumkin va tutilish erkinligiga erishgan tuberoz sklerozli bolalar cheksiz ketogenik parhezda qolishlari mumkin.[48]
Variantlar
Klassik

Ketogenik parhez a tomonidan hisoblanadi parhezshunos har bir bola uchun. Yoshi, vazni, faollik darajasi, madaniyati va ovqatlanish afzalliklari ovqatlanish rejasiga ta'sir qiladi. Birinchidan, energiya talablari bolaning yoshi uchun tavsiya etilgan kunlik miqdorning (RDA) 80-90% darajasida o'rnatiladi (yuqori yog'li diet oddiy uglevodli dietaga qaraganda ishlov berish uchun kam energiya talab qiladi). Juda faol bolalar yoki mushaklari bo'lganlar spastiklik bundan ko'proq oziq-ovqat energiyasini talab qilish; harakatsiz bolalar kamroq talab qiladi. Ratsionning ketogenik nisbati yog'ning og'irligini uglevod va oqsilning umumiy og'irligi bilan taqqoslaydi. Bu odatda 4: 1 ni tashkil qiladi, ammo 18 oydan kichik, 12 yoshdan katta yoki semirib ketgan bolalar 3: 1 nisbatda boshlanishi mumkin. Yog 'energiyaga boy, uglevod yoki oqsil uchun 4 kkal / g (17 kJ / g) bilan solishtirganda 9 kkal / g (38 kJ / g), shuning uchun ketogenik parhezning miqdori odatdagidan kichikdir. The quantity of fat in the diet can be calculated from the overall energy requirements and the chosen ketogenic ratio. Next, the protein levels are set to allow for growth and body maintenance, and are around 1 g protein for each kg of body weight. Lastly, the amount of carbohydrate is set according to what allowance is left while maintaining the chosen ratio. Any carbohydrate in medications or qo'shimchalar must be subtracted from this allowance. The total daily amount of fat, protein, and carbohydrate is then evenly divided across the meals.[39]
A computer program such as KetoCalculator may be used to help generate recipes.[49] The meals often have four components: heavy whipping cream, a protein-rich food (typically meat), a fruit or vegetable and a fat such as butter, vegetable oil, or mayonnaise. Only low-carbohydrate fruits and vegetables are allowed, which excludes bananas, potatoes, peas, and corn. Suitable fruits are divided into two groups based on the amount of carbohydrate they contain, and vegetables are similarly divided into two groups. Foods within each of these four groups may be freely substituted to allow for variation without needing to recalculate portion sizes. For example, cooked broccoli, Brussels sprouts, cauliflower, and green beans are all equivalent. Fresh, canned, or frozen foods are equivalent, but raw and cooked vegetables differ, and processed foods are an additional complication. Parents are required to be precise when measuring food quantities on an electronic o'lchov accurate to 1 g. The child must eat the whole meal and cannot have extra portions; any snacks must be incorporated into the meal plan. A small amount of MCT oil may be used to help with constipation or to increase ketosis.[39]
The classic ketogenic diet is not a muvozanatli ovqatlanish and only contains tiny portions of fresh fruit and vegetables, mustahkamlangan cereals, and calcium-rich foods. Xususan, B vitaminlari, kaltsiy va D vitamini must be artificially supplemented. This is achieved by taking two sugar-free supplements designed for the patient's age: a multivitamin bilan minerallar va kaltsiy D vitamini bilan.[18] A typical day of food for a child on a 4:1 ratio, 1,500 kcal (6,300 kJ) ketogenic diet comprises three small meals and three small snacks:[30]
| Ovqat | Menu idea | Tarkibi |
|---|---|---|
| Nonushta | Egg with bacon |
|
| Morning snack | Peanut butter ball (serving size: 0.5 ounce) |
|
| Tushlik | Tuna salatasi |
|
| Afternoon snack | Keto yogurt (serving size: 1.3 ounces) |
|
| Kechki ovqat | Cheeseburger (no bun) |
|
| Evening snack | Keto custard (serving size: 1.2 ounces) |
|
MCT oil
Normal dietary fat contains mostly long-chain triglycerides (LCTs). Medium-chain triglycerides (MCTs) are more ketogenic than LCTs because they generate more ketones per unit of energy when metabolised. Their use allows for a diet with a lower proportion of fat and a greater proportion of protein and carbohydrate,[18] leading to more food choices and larger portion sizes.[4] The original MCT diet developed by Peter Huttenlocher in the 1970s derived 60% of its calories from MCT oil.[15] Consuming that quantity of MCT oil caused abdominal cramps, diarrhea, and vomiting in some children. A figure of 45% is regarded as a balance between achieving good ketosis and minimising gastrointestinal complaints. The classical and modified MCT ketogenic diets are equally effective and differences in tolerability are not statistically significant.[46] The MCT diet is less popular in the United States; MCT oil is more expensive than other dietary fats and is not covered by sug'urta kompaniyalari.[18]
Modified Atkins
First reported in 2003, the idea of using a form of the Atkins diet to treat epilepsy came about after parents and patients discovered that the induction phase of the Atkins diet controlled seizures. The ketogenic diet team at Johns Hopkins Hospital modified the Atkins diet by removing the aim of achieving weight loss, extending the induction phase indefinitely, and specifically encouraging fat consumption. Compared with the ketogenic diet, the modified Atkins diet (MAD) places no limit on calories or protein, and the lower overall ketogenic ratio (about 1:1) does not need to be consistently maintained by all meals of the day. The MAD does not begin with a fast or with a stay in hospital and requires less dietitian support than the ketogenic diet. Carbohydrates are initially limited to 10 g per day in children or 20 g per day in adults, and are increased to 20–30 g per day after a month or so, depending on the effect on seizure control or tolerance of the restrictions. Like the ketogenic diet, the MAD requires vitamin and mineral supplements and children are carefully and periodically monitored at outpatient clinics.[50]
The modified Atkins diet reduces seizure frequency by more than 50% in 43% of patients who try it and by more than 90% in 27% of patients.[18] Few adverse effects have been reported, though cholesterol is increased and the diet has not been studied long term.[50] Although based on a smaller data set (126 adults and children from 11 studies over five centres), these results from 2009 compare favorably with the traditional ketogenic diet.[18]
Low glycemic index treatment
The low glycemic index treatment (LGIT)[51] is an attempt to achieve the stable qon glyukoza levels seen in children on the classic ketogenic diet while using a much less restrictive regimen. The hypothesis is that stable blood glucose may be one of the mechanisms of action involved in the ketogenic diet,[46] which occurs because the absorption of the limited carbohydrates is slowed by the high fat content.[5] Although it is also a high-fat diet (with approximately 60% calories from fat),[5] the LGIT allows more carbohydrate than either the classic ketogenic diet or the modified Atkins diet, approximately 40–60 g per day.[18] However, the types of carbohydrates consumed are restricted to those that have a glycaemic index lower than 50. Like the modified Atkins diet, the LGIT is initiated and maintained at outpatient clinics and does not require precise weighing of food or intensive dietitian support. Both are offered at most centres that run ketogenic diet programmes, and in some centres they are often the primary dietary therapy for adolescents.[46]
Short-term results for the LGIT indicate that at one month approximately half of the patients experience a greater than 50% reduction in seizure frequency, with overall figures approaching that of the ketogenic diet. The data (coming from one centre's experience with 76 children up to the year 2009) also indicate fewer side effects than the ketogenic diet and that it is better tolerated, with more palatable meals.[18][52]
Prescribed formulations

Infants and patients fed via a gastrostomiya naychasi can also be given a ketogenic diet. Parents make up a belgilangan powdered formula, such as KetoCal, into a liquid feed.[21] Gastrostomy feeding avoids any issues with palatability, and bottle-fed infants readily accept the ketogenic formula.[33] Some studies have found this liquid feed to be more efficacious and associated with lower total xolesterin than a solid ketogenic diet.[18] KetoCal is a nutritionally complete food containing milk protein and is supplemented with amino acids, fat, carbohydrate, vitamins, minerals and trace elements. It is used to administer the 4:1 ratio classic ketogenic diet in children over one year. The formula is available in both 3:1 and 4:1 ratios, either unflavoured or in an artificially sweetened vanilla flavour and is suitable for tube or oral feeding.[53] Other formula products include KetoVolve[54] and Ketonia.[55] Alternatively, a liquid ketogenic diet may be produced by combining Ross Carbohydrate Free soy formula with Microlipid and Polycose.[55]
Butun dunyo bo'ylab
In theory, there are no restrictions on where the ketogenic diet might be used, and it can cost less than modern anticonvulsants. However, fasting and dietary changes are affected by religious and cultural issues. A culture where food is often prepared by grandparents or hired help means more people must be educated about the diet. When families dine together, sharing the same meal, it can be difficult to separate the child's meal. In many countries, food labelling is not mandatory, so calculating macronutrients such as fat, protein and carbohydrates can be difficult. In some countries, it may be hard to find sugar-free forms of medicines and supplements, to purchase an accurate electronic scale, or to afford MCT oils.[56]
In Asia, the traditional diet includes rice and noodles as the main source of energy, making their elimination difficult. Therefore, the MCT-oil form of the diet, which allows more carbohydrate, has proved useful. In India, religious beliefs commonly affect the diet: for instance, Hindus consider cows sacred animals not to be killed and eaten, Islam forbids consumption of pork va strict vegetarians of the Jain faith do not eat root vegetables. The Indian ketogenic diet is started without a fast due to cultural opposition towards fasting in children. The low-fat, high-carbohydrate nature of the normal Indian and Asian diet means that their ketogenic diets typically have a lower ketogenic ratio (1:1) than in America and Europe. However, they appear to be just as effective.[56]
In many developing countries, the ketogenic diet is expensive because dairy fats and meat are more expensive than grain, fruit, and vegetables. The modified Atkins diet has been proposed as a lower-cost alternative for those countries; the slightly more expensive food bill can be offset by a reduction in pharmaceutical costs if the diet is successful. The modified Atkins diet is less complex to explain and prepare and requires less support from a dietitian.[57]
Ta'sir mexanizmi
Seizure pathology
The brain is composed of a network of neurons that transmit signals by propagating asab impulslari. The propagation of this impulse from one neuron to another is typically controlled by neyrotransmitterlar, though there are also electrical pathways between some neurons. Neurotransmitters can inhibit impulse firing (primarily done by b-aminobutirik kislota, or GABA) or they can excite the neuron into firing (primarily done by glutamat ). A neuron that releases inhibitory neurotransmitters from its terminals is called an inhibitory neuron, while one that releases excitatory neurotransmitters is an excitatory neuron. When the normal balance between inhibition and excitation is significantly disrupted in all or part of the brain, a seizure can occur. The GABA system is an important target for anticonvulsant drugs, since seizures may be discouraged by increasing GABA synthesis, decreasing its breakdown, or enhancing its effect on neurons.[7]
The nerve impulse is characterised by a great influx of sodium ions through kanallar in the neuron's hujayra membranasi followed by an efflux of potassium ions through other channels. The neuron is unable to fire again for a short time (known as the refrakter davr ), which is mediated by another kaliy kanali. The flow through these ion kanallari is governed by a "gate" which is opened by either a voltage change or a chemical messenger sifatida tanilgan ligand (such as a neurotransmitter). These channels are another target for anticonvulsant drugs.[7]
There are many ways in which epilepsy occurs. Examples of pathological physiology include: unusual excitatory connections within the neuronal network of the brain; abnormal neuron structure leading to altered current flow; decreased inhibitory neurotransmitter synthesis; ineffective receptors for inhibitory neurotransmitters; insufficient breakdown of excitatory neurotransmitters leading to excess; immature synapse development; and impaired function of ionic channels.[7]
Seizure control
Although many hypotheses have been put forward to explain how the ketogenic diet works, it remains a mystery. Disproven hypotheses include systemic acidosis (high levels of acid in the blood), electrolyte changes va hypoglycaemia (past qon glyukoza ).[21] Although many biochemical changes are known to occur in the brain of a patient on the ketogenic diet, it is not known which of these has an anticonvulsant effect. The lack of understanding in this area is similar to the situation with many anticonvulsant drugs.[58]
On the ketogenic diet, carbohydrates are restricted and so cannot provide for all the metabolic needs of the body. Instead, fatty acids are used as the major source of fuel. These are used through fatty-acid oxidation in the cell's mitoxondriya (the energy-producing parts of the cell). Humans can convert some aminokislotalar into glucose by a process called glyukoneogenez, but cannot do this by using fatty acids.[59] Since amino acids are needed to make proteins, which are essential for growth and repair of body tissues, these cannot be used only to produce glucose. This could pose a problem for the brain, since it is normally fuelled solely by glucose, and most fatty acids do not cross the qon-miya to'sig'i. However, the liver can use long-chain fatty acids to synthesise the three keton tanasi β-hydroxybutyrate, asetoatsetat va aseton. These ketone bodies enter the brain and qisman o'rnini bosuvchi qon glyukoza energiya manbai sifatida.[58]
The ketone bodies are possibly anticonvulsant; yilda hayvon modellari, acetoacetate and acetone protect against seizures. The ketogenic diet results in adaptive changes to brain energy metabolism that increase the energy reserves; ketone bodies are a more efficient fuel than glucose, and the number of mitochondria is increased. This may help the neyronlar to remain stable in the face of increased energy demand during a seizure, and may confer a neyroprotektiv effekt.[58]
The ketogenic diet has been studied in at least 14 rodent animal models of seizures. It is protective in many of these models and has a different protection profile than any known anticonvulsant. Aksincha, fenofibrat, not used clinically as an antiepileptic, exhibits experimental antikonvulsant properties in adult rats comparable to the ketogenic diet.[60] This, together with studies showing its efficacy in patients who have failed to achieve seizure control on half a dozen drugs, suggests a unique mechanism of action.[58]
Anticonvulsants suppress epileptic seizures, but they neither cure nor prevent the development of seizure susceptibility. The development of epilepsy (epileptogenesis) is a process that is poorly understood. A few anticonvulsants (valproat, levetiratsetam va benzodiazepinlar ) have shown antiepileptogenic properties in animal models of epileptogenesis. However, no anticonvulsant has ever achieved this in a clinical trial in humans. The ketogenic diet has been found to have antiepileptogenic properties in rats.[58]
Boshqa dasturlar
The ketogenic diet has been studied for potential therapeutic use in various neurological disorders other than epilepsy: Altsgeymer kasalligi (AD), amiotrofik lateral skleroz (ALS), autizm, bosh og'rig'i, neyrotravma, og'riq, Parkinson kasalligi (PD) va uyqu buzilishi.[6]
Because some cancer cells are inefficient in processing ketone bodies for energy, the ketogenic diet has also been suggested as a treatment for cancer.[61][62] A 2018 review looked at the evidence from preclinical and clinical studies of ketogenic diets in cancer therapy. The clinical studies in humans are typically very small, with some providing weak evidence for an anti-tumour effect, particularly for glioblastoma, but in other cancers and studies, no anti-tumour effect was seen. Taken together, results from preclinical studies, albeit sometimes contradictory, tend to support an anti-tumor effect rather than a pro-tumor effect of the KD for most solid cancers.[63]
The evidence of benefit for these conditions has not reached the level where clinical recommendations can be made.[46]
Shuningdek qarang
- Atkins diet – brand of low-carbohydrate diet
- Ketoz – metabolic process that uses fats as an energy source
- Parhezlar ro'yxati
- Kam uglevodli diet – varieties of diets that focus on reducing carbohydrates
- O'rta zanjirli triglitserid – easily absorbed, naturally occurring type of fat
- Moda parhezi
Izohlar
- ^ Ushbu maqolada, kkal degan ma'noni anglatadi kaloriya as a unit of measure (4.1868 kJ), and kaloriya stands for "energy" from food.
- ^ Unless otherwise stated, the term ro'za in this article refers to going without food while maintaining calorie-free fluid intake.
- ^ Hippocrates, Muqaddas kasallik to'g'risida, ch. 18; jild 6.
- ^ Hippocrates, Epidemiya, VII, 46; jild 5.
- ^ Galen, De venae sect. adv. Erasistrateos Romae degentes, v. 8; jild 11.
- ^ Galen, De victu attenuante, v. 1.
- ^ A yaxshi reduction is defined here to mean a 50–90% decrease in seizure frequency. An zo'r reduction is a 90–99% decrease.
- ^ Ketogenic "eggnog" is used during induction and is a drink with the required ketogenic ratio. For example, a 4:1 ratio eggnog would contain 60 g of 36% heavy whipping cream, 25 g pasteurised raw egg, saxarin and vanilla flavour. This contains 245 kcal (1,025 kJ), 4 g protein, 2 g carbohydrate and 24 g fat (24:6 = 4:1).[17] The eggnog may also be cooked to make a custard, or frozen to make ice cream.[39]
Adabiyotlar
- ^ a b v d e f g h men Freeman JM, Kossoff EH, Hartman AL. The ketogenic diet: one decade later. Pediatriya. 2007 Mar;119(3):535–43. doi:10.1542 / peds.2006-2447. PMID 17332207
- ^ a b v d Martin-McGill KJ, Jackson CF, Bresnahan R, Levy RG, Cooper PN. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. 2018 Nov 7;11:CD001903. doi:10.1002/14651858.CD001903.pub4. PMID 30403286
- ^ Kossoff EH, Wang HS. Dietary therapies for epilepsy. Biomed J. 2013 Jan-Feb;36(1):2-8. doi:10.4103/2319-4170.107152 PMID 23515147
- ^ a b Liu YM. Medium-chain triglyceride (MCT) ketogenic therapy. Epilepsiya. 2008 Nov;49 Suppl 8:33–6. doi:10.1111/j.1528-1167.2008.01830.x. PMID 19049583
- ^ a b v d e Zupec-Kania BA, Spellman E. An overview of the ketogenic diet for pediatric epilepsy. Nutr Clin Pract. 2008 Dec–2009 Jan;23(6):589–96. doi:10.1177/0884533608326138. PMID 19033218
- ^ a b Gano LB, Patel M, Rho JM. Ketogenic diets, mitochondria, and neurological diseases. J lipid rez. 2014 Nov;55(11):2211-28. doi:10.1194/jlr.R048975. PMID 24847102.
- ^ a b v d e Stafstrom CE. An introduction to seizures and epilepsy. In: Stafstrom CE, Rho JM, editors. Epilepsy and the ketogenic diet. Totowa: Humana Press; 2004 yil. ISBN 1-58829-295-9.
- ^ de Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsiya Behav. 2008 May;12(4):540–6. doi:10.1016/j.yebeh.2007.12.019. PMID 18280210
- ^ Cai QY, Zhou ZJ, Luo R, Gan J, Li SP, Mu DZ, Wan CM. Safety and tolerability of the ketogenic diet used for the treatment of refractory childhood epilepsy: a systematic review of published prospective studies. World J Pediatr. 2017 Dec;13(6):528-536. doi:10.1007/s12519-017-0053-2. PMID 28702868.
- ^ a b v d e f g h men Wheless JW. History and origin of the ketogenic diet (PDF). In: Stafstrom CE, Rho JM, editors. Epilepsy and the ketogenic diet. Totowa: Humana Press; 2004 yil. ISBN 1-58829-295-9.
- ^ Temkin O. The falling sickness: a history of epilepsy from the Greeks to the beginnings of modern neurology. 2-nashr. Baltimore: Johns Hopkins University Press; 1971. p. 33, 57, 66, 67, 71, 78. ISBN 0-8018-4849-0.
- ^ Guelpa, G; Marie, A (1911). "La lutte contre l'epilepsie par la desintoxication et par la reeducation alimentaire" [The fight against epilepsy by detoxification and by the reeducation about food]. Rev Ther Med-Chirurg. 78 (1): 8–13.CS1 maint: ref = harv (havola)As cited by Bailey (2005).
- ^ Bailey EE, Pfeifer HH, Thiele EA. The use of diet in the treatment of epilepsy. Epilepsiya Behav. 2005 Feb;6(1):4–8. doi:10.1016/j.yebeh.2004.10.006. PMID 15652725
- ^ Kossoff EH. Do ketogenic diets work for adults with epilepsy? Ha! epilepsy.com. 2007, March. Cited 24 October 2009.
- ^ a b v Huttenlocher PR, Wilbourn AJ, Signore JM. Medium-chain triglycerides as a therapy for intractable childhood epilepsy. Nevrologiya. 1971 Nov;21(11):1097–103. doi:10.1212/wnl.21.11.1097. PMID 5166216
- ^ a b Neal EG, Chaffe H, Schwartz RH, Lawson MS, Edwards N, Fitzsimmons G, va boshq. The ketogenic diet for the treatment of childhood epilepsy: a randomised controlled trial. Lanset neyroli. 2008 Jun;7(6):500–6. doi:10.1016/S1474-4422(08)70092-9. PMID 18456557
- ^ a b v Vining EP, Freeman JM, Ballaban-Gil K, Camfield CS, Camfield PR, Holmes GL, va boshq. A multicenter study of the efficacy of the ketogenic diet. Arch Neurol. 1998 Nov;55(11):1433–7. doi:10.1001/archneur.55.11.1433. PMID 9823827
- ^ a b v d e f g h men j k l m n o p q Kossoff EH, Zupec-Kania BA, Rho JM. Ketogenic diets: an update for child neurologists. J Child Neurol. 2009 Aug;24(8):979–88. doi:10.1177/0883073809337162. PMID 19535814
- ^ a b v d e f g h men j k l Kossoff EH, Zupec-Kania BA, Auvin S, Ballaban-Gil KR, Christina Bergqvist AG, Blackford R, Buchhalter JR, Caraballo RH, Cross JH, Dahlin MG, Donner EJ, Guzel O, Jehle RS, Klepper J, Kang HC, Lambrechts DA, Liu YMC, Nathan JK, Nordli DR Jr, Pfeifer HH, Rho JM, Scheffer IE, Sharma S, Stafstrom CE, Thiele EA, Turner Z, Vaccarezza MM, van der Louw EJTM, Veggiotti P, Wheless JW, Wirrell EC; Charlie Foundation; Matthew's Friends; Practice Committee of the Child Neurology Society. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open. 2018 May 21;3(2):175-192. doi:10.1002/epi4.12225. PMID 29881797.
- ^ Husari KS, Cervenka MC. The ketogenic diet all grown up-Ketogenic diet therapies for adults. Epilepsiya Res. 2020 May;162:106319. doi:10.1016/j.eplepsyres.2020.106319. PMID 32199222.
- ^ a b v d e f g h men j k l Hartman AL, Vining EP. Clinical aspects of the ketogenic diet. Epilepsiya. 2007 Jan;48(1):31–42. doi:10.1111/j.1528-1167.2007.00914.x PMID 17241206
- ^ Freeman JM, Vining EP, Pillas DJ, Pyzik PL, Casey JC, Kelly LM. The efficacy of the ketogenic diet—1998: a prospective evaluation of intervention in 150 children. Pediatriya. 1998 Dec;102(6):1358–63. doi:10.1542/peds.102.6.1358. PMID 9832569. https://web.archive.org/web/20040629224858/http://www.hopkinsmedicine.org/press/1998/DECEMBER/981207.HTM Lay summary]—JHMI Office of Communications and Public Affairs. Updated 7 December 1998. Cited 6 March 2008.
- ^ a b Hemingway C, Freeman JM, Pillas DJ, Pyzik PL. The ketogenic diet: a 3- to 6-year follow-up of 150 children enrolled prospectively. Pediatriya. 2001 Oct;108(4):898–905. doi:10.1542/peds.108.4.898. PMID 11581442
- ^ Kossoff EH, Rho JM. Ketogenic diets: evidence for short- and long-term efficacy. Neurotherapeutics. 2009 Apr;6(2):406–14. doi:10.1016/j.nurt.2009.01.005 PMID 19332337.
- ^ Henderson CB, Filloux FM, Alder SC, Lyon JL, Caplin DA. Efficacy of the ketogenic diet as a treatment option for epilepsy: meta-analysis. J Child Neurol. 2006 Mar;21(3):193–8. doi:10.2310/7010.2006.00044. PMID 16901419
- ^ Liu H, Yang Y, Wang Y, Tang H, Zhang F, Zhang Y, Zhao Y. Ketogenic diet for treatment of intractable epilepsy in adults: A meta-analysis of observational studies. Epilepsia Open. 2018 Feb 19;3(1):9–17. doi:10.1002/epi4.12098. PMID 29588983.
- ^ Bergqvist AGC. Indications and Contraindications of the Ketogenic diet. In: Stafstrom CE, Rho JM, editors. Epilepsy and the ketogenic diet. Totowa: Humana Press; 2004. p. 53–61. ISBN 1-58829-295-9.
- ^ a b Epilepsies: diagnosis and management. Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti (NICE). Published January 2012. Updated February 2016. Cited March 2018. ISBN 978-1-4731-1790-7.
- ^ a b Scottish Intercollegiate Guidelines Network. Guideline 81, Diagnosis and management of epilepsies in children and young people. A national clinical guideline (PDF). Edinburgh: Royal College of Physicians; 2005 yil. ISBN 1-899893-24-5.
- ^ a b v d Turner Z, Kossoff EH. The ketogenic and Atkins diets: recipes for seizure control (PDF). Pract Gastroenterol. 2006 Jun;29(6):53, 56, 58, 61–2, 64.
- ^ Stainman RS, Turner Z, Rubenstein JE, Kossoff EH. Decreased relative efficacy of the ketogenic diet for children with surgically approachable epilepsy. Seizure. 2007 Oct;16(7):615–9. doi:10.1016/j.seizure.2007.04.010. PMID 17544706
- ^ Kossoff EH, McGrogan JR, Freeman JM. Benefits of an all-liquid ketogenic diet. Epilepsiya. 2004 Sep;45(9):1163. doi:10.1111/j.0013-9580.2004.18504.x. PMID 15329084.
- ^ a b v d Kossoff EH, Freeman JM. The ketogenic diet—the physician's perspective. In: Stafstrom CE, Rho JM, editors. Epilepsy and the ketogenic diet. Totowa: Humana Press; 2004. p. 53–61. ISBN 1-58829-295-9.
- ^ Spendiff S. The diet that can treat epilepsy. Guardian. 2008 Aug 15;Sect. Health & wellbeing.
- ^ Wang S, Fallah A. Optimal management of seizures associated with tuberous sclerosis complex: current and emerging options. Neuropsychiatr Dis Treat. 2014 Oct 23;10:2021–30. doi:10.2147/NDT.S51789. PMID 25364257
- ^ Mastriani KS, Williams VC, Hulsey TC, Wheless JW, Maria BL. Evidence-based versus reported epilepsy management practices. J Child Neurol. 2008 Feb 15;23(5):507–14. doi:10.1177/0883073807309785. PMID 18281618
- ^ Wang D, Pascual JM, De Vivo D. Glyukoza tashuvchisi 1-toifa etishmovchilik sindromi. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A, muharrirlar. GeneReviews. Seattle (WA): University of Washington, Seattle; 1993–2018. 2002 Jul 30 [updated 2018 Mar 1]. PMID 20301603.
- ^ Huffman J, Kossoff EH. State of the ketogenic diet(s) in epilepsy (PDF). Curr Neurol Neurosci Rep. 2006 Jul;6(4):332–40. doi:10.1007/s11910-006-0027-6. PMID 16822355
- ^ a b v d e Zupec-Kania B, Werner RR, Zupanc ML. Clinical Use of the Ketogenic Diet—The Dietitian's Role. In: Stafstrom CE, Rho JM, editors. Epilepsy and the ketogenic diet. Totowa: Humana Press; 2004. p. 63-81. ISBN 1-58829-295-9.
- ^ a b v Bergqvist AG. Long-term monitoring of the ketogenic diet: Do's and Don'ts. Epilepsiya Res. 2011 Aug 18;100(3):261–6. doi:10.1016/j.eplepsyres.2011.05.020. PMID 21855296.
- ^ a b v d e f g Sampath A, Kossoff EH, Furth SL, Pyzik PL, Vining EP. Kidney stones and the ketogenic diet: risk factors and prevention (PDF). J Child Neurol. 2007 Apr;22(4):375–8. doi:10.1177/0883073807301926. PMID 17621514
- ^ Kossoff E. Is there a role for the ketogenic diet beyond childhood? In: Freeman J, Veggiotti P, Lanzi G, Tagliabue A, Perucca E. The ketogenic diet: from molecular mechanisms to clinical effects. Epilepsiya Res. 2006 Feb;68(2):145–80. doi:10.1016/j.eplepsyres.2005.10.003. PMID 16523530
- ^ Vogelstein F. Epilepsy's Big, Fat Miracle. Nyu-York Tayms. 2010 Nov 17.
- ^ Kim DY, Rho JM. The ketogenic diet and epilepsy. Curr Opin Clin Nutr Metab Care. 2008 Mar;11(2):113–20. doi:10.1097/MCO.0b013e3282f44c06. PMID 18301085
- ^ a b Kossoff EH, Laux LC, Blackford R, Morrison PF, Pyzik PL, Hamdy RM, va boshq. When do seizures usually improve with the ketogenic diet? (PDF). Epilepsiya. 2008 Feb;49(2):329–33. doi:10.1111/j.1528-1167.2007.01417.x. PMID 18028405
- ^ a b v d e f Kossoff EH, Zupec-Kania BA, Amark PE, Ballaban-Gil KR, Bergqvist AG, Blackford R, va boshq. Optimal clinical management of children receiving the ketogenic diet: recommendations of the International Ketogenic Diet Study Group. Epilepsiya. 2009 Feb;50(2):304–17. doi:10.1111/j.1528-1167.2008.01765.x. PMID 18823325
- ^ Musa-Veloso K, Cunnane SC. Measuring and interpreting ketosis and fatty acid profiles in patients on a high-fat ketogenic diet. In: Stafstrom CE, Rho JM, editors. Epilepsy and the ketogenic diet. Totowa: Humana Press; 2004. p. 129–41. ISBN 1-58829-295-9.
- ^ a b Martinez CC, Pyzik PL, Kossoff EH. Discontinuing the ketogenic diet in seizure-free children: recurrence and risk factors. Epilepsiya. 2007 Jan;48(1):187–90. doi:10.1111/j.1528-1167.2006.00911.x. PMID 17241227
- ^ Zupec-Kania B. KetoCalculator: a web-based calculator for the ketogenic diet. Epilepsiya. 2008 Nov;49 Suppl 8:14–6. doi:10.1111/j.1528-1167.2008.01824.x. PMID 19049577
- ^ a b Kossoff EH, Dorward JL. The modified Atkins diet. Epilepsiya. 2008 Nov;49 Suppl 8:37–41. doi:10.1111/j.1528-1167.2008.01831.x. PMID 19049584
- ^ Pfeifer, Heidi H. Low glycemic index treatment. Epilepsiya fondi. 22 August 2013. Cited 31 March 2018.
- ^ Muzykewicz DA, Lyczkowski DA, Memon N, Conant KD, Pfeifer HH, Thiele EA. Efficacy, safety, and tolerability of the low glycemic index treatment in pediatric epilepsy. Epilepsiya. 2009 May;50(5):1118–26. doi:10.1111/j.1528-1167.2008.01959.x. PMID 19220406
- ^ KetoCal Product Information. Nutricia North America. Cited 8 June 2018.
- ^ KetoVOLVE: 4:1 Ratio Powder. Solace Nutrition. Cited 17 June 2013.
- ^ a b Kossoff EH. The Ketogenic Diet ... in a bottle?. Keto News. Epilepsy.com. Updated July 2009. Cited 29 November 2009.
- ^ a b Kossoff EH, McGrogan JR. Worldwide use of the ketogenic diet. Epilepsiya. 2005 Feb;46(2):280–9. doi:10.1111/j.0013-9580.2005.42704.x. PMID 15679509.
- ^ Kossoff EH, Dorward JL, Molinero MR, Holden KR. The modified Atkins diet: a potential treatment for developing countries. Epilepsiya. 2008 Sep;49(9):1646–7. doi:10.1111/j.1528-1167.2008.01580_6.x PMID 18782218
- ^ a b v d e Hartman AL, Gasior M, Vining EP, Rogawski MA. The neuropharmacology of the ketogenic diet. Pediatr Neurol. 2007 May;36(5):281–292. doi:10.1016/j.pediatrneurol.2007.02.008. PMID 17509459
- ^ Kerndt PR, Naughton JL, Driscoll CE, Loxterkamp DA. Fasting: the history, pathophysiology and complications. West J Med. 1982 Nov;137(5):379–99. PMID 6758355
- ^ Porta N, Vallée L, Lecointe C, Bouchaert E, Staels B, Bordet R, Auvin S. Fenofibrate, a peroxisome proliferator-activated receptor-alpha agonist, exerts anticonvulsive properties. Epilepsiya. 2009 Apr;50(4):943–8. doi:10.1111/j.1528-1167.2008.01901.x. PMID 19054409.
- ^ Barañano KW, Hartman AL. The ketogenic diet: uses in epilepsy and other neurologic illnesses. Curr Treat Options Neurol. 2008;10(6):410–9. doi:10.1007/s11940-008-0043-8. PMID 18990309
- ^ Allen BG, Bhatia SK, Anderson CM, et al. Ketogenic diets as an adjuvant cancer therapy: History and potential mechanism. Redox Biol. 2014 Aug 7;2C:963–70. doi:10.1016/j.redox.2014.08.002. PMID 25460731
- ^ Weber DD, Aminazdeh-Gohari S, Kofler B. Ketogenic diet in cancer therapy. Aging (Albany NY). 2018 Feb 11;10(2):164–165. doi:10.18632/aging.101382. PMID 29443693 PMC 5842847.
Qo'shimcha o'qish
- Freeman JM, Kossoff EH, Freeman JB, Kelly MT. The Ketogenic Diet: A Treatment for Children and Others with Epilepsy. 4-nashr. New York: Demos; 2007 yil. ISBN 1-932603-18-2.
Tashqi havolalar
- Diet Review: Ketogenic Diet for Weight Loss, from the Harvard University School of Public Health
- Ketogenik parhez da Curlie
- Matthew's Friends, a UK charity and information resource
- The Charlie Foundation, a US charity and information resource
- Epilepsy.com: Dietary Therapies & Ketogenic News, information and regular research news updates