Toksoplazmoz - Toxoplasmosis
| Toksoplazmoz | |
|---|---|
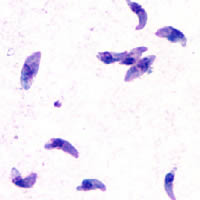 | |
| T. gondii taxizoidlar | |
| Mutaxassisligi | Yuqumli kasallik |
| Alomatlar | Ko'pincha, hech qachon homiladorlik (tug'ma nuqsonlar)[1][2] |
| Sabablari | Toxoplasma gondii[3] |
| Xavf omillari | Noto'g'ri pishirilgan ovqatni iste'mol qilish, yuqtirilgan mushuklarning najasiga ta'sir qilish[3] |
| Diagnostika usuli | Qon testi, amniotik suyuqlik sinov[4] |
| Davolash | Homiladorlik paytida spiramitsin yoki pirimetamin /sulfadiazin va folin kislotasi[5] |
| Chastotani | Odamlarning 50% gacha, yiliga 200 mingta tug'ma toksoplazmoz kasalligi[6][7] |
Toksoplazmoz a parazitar kasallik sabab bo'lgan Toxoplasma gondii.[3] Toksoplazmoz bilan yuqadigan infektsiyalar odatda kattalarda aniq alomatlarni keltirib chiqarmaydi.[2] Ba'zida odamlarda bir necha hafta yoki bir necha oy yumshoq bo'lishi mumkin, grippga o'xshash kasallik mushaklarning og'rig'i va yumshoqligi kabi limfa tugunlari.[1] Kam sonli odamlarda ko'z bilan bog'liq muammolar rivojlanishi mumkin.[1] A bo'lganlarda zaif immunitet tizimi kabi jiddiy alomatlar soqchilik va yomon koordinatsiya yuzaga kelishi mumkin.[1] Davomida yuqtirgan bo'lsa homiladorlik, tug'ma toksoplazmoz deb ataladigan holat bolaga ta'sir qilishi mumkin.[1]
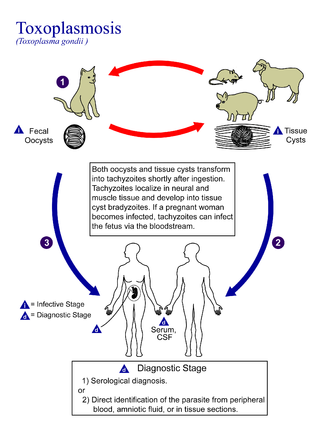
Toksoplazmoz odatda tarkibida kam pishgan ovqatni iste'mol qilish orqali tarqaladi kistalar, homiladorlik paytida mushukning yuqtirgan najasiga va yuqtirgan onadan chaqalog'iga ta'sir qilish.[3] Kamdan kam hollarda kasallik tarqalishi mumkin qon quyish.[3] Odamlar orasida boshqacha tarzda tarqalmaydi.[3] Parazit jinsiy yo'l bilan ko'payishni faqat mushuk oilasi.[8] Biroq, u ko'pchilik turlarini yuqtirishi mumkin issiq qonli hayvonlar odamlar, shu jumladan.[8] Tashxis odatda qonni tekshirish orqali amalga oshiriladi antikorlar yoki sinov orqali amniotik suyuqlik parazit uchun DNK.[4]
Oldini olish ovqatni to'g'ri tayyorlash va pishirish orqali amalga oshiriladi.[9] Shuningdek, homilador ayollarga mushuk axlat qutilarini tozalamaslik tavsiya etiladi, yoki keyinchalik qo'lqop kiyib, qo'llarini yuvish kerak bo'lsa.[9] Aks holda sog'lom odamlarni davolash odatda kerak emas.[5] Homiladorlik paytida, spiramitsin yoki pirimetamin /sulfadiazin va folin kislotasi davolash uchun ishlatilishi mumkin.[5]
Dunyo aholisining yarmigacha toksoplazmoz bilan kasallangan, ammo alomatlari yo'q.[7] Qo'shma Shtatlarda odamlarning taxminan 11% yuqtirgan bo'lsa, dunyoning ayrim mintaqalarida bu 60% dan oshadi.[3] Tug'ma toksoplazmozning yiliga taxminan 200 ming holati ro'y beradi.[6] Charlz Nikoll va Louis Manceaux birinchi marta organizmni 1908 yilda tasvirlab bergan.[10] 1941 yilda homiladorlik paytida onadan bolaga yuqishi tasdiqlandi.[10] Infektsiya odamlarning xatti-harakatlariga ta'sir qilishi mumkinligi to'g'risida taxminiy dalillar mavjud.[11]
Belgilari va alomatlari
Yuqtirish uch bosqichdan iborat:
O'tkir
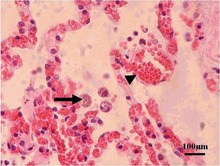
O'tkir toksoplazmoz ko'pincha sog'lom kattalarda asemptomatik bo'ladi.[12][13] Biroq, alomatlar namoyon bo'lishi mumkin va ko'pincha gripp o'xshash: shishgan limfa tugunlari, bosh og'rig'i, isitma va charchoq,[14] yoki mushak og'rig'i va bir oy yoki undan ko'proq davom etadigan og'riqlar. To'liq ishlaydigan odam uchun kamdan-kam uchraydi immunitet tizimi infektsiyadan keyin og'ir alomatlar paydo bo'lishi. Immun tizimi zaif odamlarda bosh og'rig'i, chalkashlik, koordinatsiya sustligi, tutilish, o'pkada sil kasalligiga o'xshash muammolar bo'lishi mumkin. Pneumocystis jiroveci pnevmoniya (OITS bilan kasallangan odamlarda uchraydigan keng tarqalgan opportunistik infeksiya) yoki retinaning qattiq yallig'lanishi (ko'z toksoplazmozi) natijasida paydo bo'ladigan ko'rish.[14] Yosh bolalar va immunitet tanqisligi odamlar, masalan, OIV / OITS bilan kasallanganlar, ayrim turlarini qabul qilganlar kimyoviy terapiya, yoki yaqinda an olganlar organ transplantatsiyasi, og'ir toksoplazmoz rivojlanishi mumkin. Bu miyaga zarar etkazishi mumkin (ensefalit ) yoki ko'zlar (nekrotizan retinoxoroidit ).[15] Orqali yuqtirgan chaqaloqlar platsenta uzatish ushbu muammolarning birortasi bilan yoki nazal nuqsonlar bilan tug'ilishi mumkin, ammo yangi tug'ilgan chaqaloqlarda bu asoratlar kam uchraydi. Toksoplazmik trofozoitlar o'tkir toksoplazmozni keltirib chiqaradigan deb nomlanadi taxizoidlar, va odatda tana suyuqliklarida uchraydi.
Shishgan limfa tugunlari odatda bo'yin yoki iyak ostida, so'ngra qo'ltiq osti va chanoqda uchraydi. Shishish dastlabki infektsiyadan keyin turli vaqtlarda paydo bo'lishi mumkin, parazitga qarshi davolanishdan mustaqil ravishda har xil vaqt davomida davom etishi va takrorlanishi mumkin.[16] Odatda kattalardagi bitta saytlarda uchraydi, ammo bolalarda bir nechta sayt tez-tez uchraydi. Kattalashgan limfa tugunlari 60% hollarda 1-2 oy ichida tugaydi. Shu bilan birga, ta'sirlanganlarning to'rtdan biri normal holatga qaytish uchun 2-4 oy davom etadi va 8% 4-6 oyni oladi. Katta miqdordagi (6%) odatdagidan ancha keyin qaytmaydi.[17]
Yashirin
Aniq simptomlar yo'qligi sababli,[12][13] xostlar osonlikcha yuqtiriladi T. gondii va toksoplazmozni bilmasdan rivojlantiradi. Yengil bo'lsa-da, grippga o'xshash alomatlar vaqti-vaqti bilan ta'sirlanishdan keyingi bir necha hafta ichida, infektsiyaga uchraydi T. gondii sog'lom odamlarda kuzatilishi mumkin bo'lgan alomatlarni keltirib chiqarmaydi.[7][18] Ko'pchilikda immunokompetent odamlar, infektsiya yashirin bosqichga kiradi, bu davrda faqat bradizoidlar (to'qima kistalarida ) mavjud;[19] bu to'qima kistalari va hatto zararlanishlari ham paydo bo'lishi mumkin retinalar, alveolyar o'pkaning shilliq qavati (bu erda o'tkir infektsiya a ni taqlid qilishi mumkin Pneumocystis jirovecii infektsiya), yurak, skelet mushaklari va markaziy asab tizimi (CNS), shu jumladan miya.[20] Kistlar CNSda hosil bo'ladi (miya to'qimasi ) yuqtirilganda T. gondii va mezbonning umri davomida davom eting.[21] Bachadonda bo'lganida yuqtirgan chaqaloqlarning aksariyati tug'ilish paytida hech qanday alomatlarga ega emas, ammo keyinchalik alomatlar paydo bo'lishi mumkin.[22]
Sharhlar serologik tadqiqotlar shuni ko'rsatdiki, global aholining 30-50% yashirin toksoplazmoz bilan kasallangan va xronik ravishda yuqtirilgan bo'lishi mumkin, ammo har bir mamlakatda infektsiya darajasi sezilarli darajada farq qiladi.[7][23][24] Infektsiyaning ushbu yashirin holati so'nggi paytlarda ko'pchilik bilan bog'liq kasallik yuklari,[7] asabiy o'zgarishlar,[21][23] va immunitetga ega bo'lmagan odamlarda jinsga bog'liq bo'lgan xatti-harakatlarning nozik o'zgarishlari,[25][26] shuningdek, avtotransport vositalarining to'qnashuvi xavfi ortadi.[27]
Teri
Kamdan kam hollarda, kasallikning erishilgan shaklida, shu jumladan teri lezyonlari paydo bo'lishi mumkin rozeola va eritema ko'p qirrali otilishlar, prurigo o'xshash tugunlar, ürtiker va makulopapulyar shikastlanishlar. Yangi tug'ilgan chaqaloqlarda bo'lishi mumkin punktat makulalar, ekximozlar, yoki "mersinli muffin" lezyonlari.Teri toksoplazmozining diagnostikasi taxyzoit shakliga asoslangan T. gondii topilgan epidermis.[28] U epidermisning barcha darajalarida uchraydi, taxminan 6 dan 2 mm gacha va kamon shaklida, yadrosi uning uchdan bir qismiga teng. Uni elektron mikroskop yordamida aniqlash mumkin Giemsa binoni sitoplazma ko'k, yadro qizil rangni ko'rsatadigan to'qima.[29]
Sababi
Parazitologiya
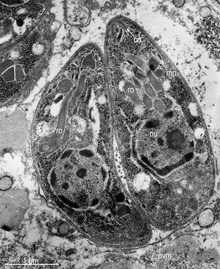
Uning hayot aylanish jarayonida, T. gondii bir nechta shakllarni qabul qiladi.[30] Tachyzoites o'tkir infektsiya uchun javobgardir; ular tez bo'linib, tana to'qimalari orqali tarqaladi. Taxyzoites "taxyzoic merozoites" deb ham tanilgan, bu bosqichning parazitologik xususiyatini aniqroq ifodalaydigan tavsiflovchi atama.[31] Ko'paygandan keyin taxyzoitlar aylanadi bradizoidlar yashirin hujayra ichidagi to'qima ichida joylashgan kistalar asosan mushak va miyada hosil bo'ladi. Kistlarning shakllanishi qisman mezbon immunitet tizimining bosimi bilan qo'zg'atiladi.[32] Bradizoidlar ("bradizoid merozoitlar" deb ham yuritiladi) antibiotiklarga ta'sir ko'rsatmaydi. Bradizoidlar hosil bo'lganidan so'ng, mezbonning umri davomida to'qimalarda qolishi mumkin. Sog'lom xostda ba'zi bradizoidlar yana faol taxizoidlarga aylansa, immunitet tizimi ularni tezda yo'q qiladi. Ammo immunitet tanqisligi bo'lgan odamlarda yoki rivojlangan immunitet tizimiga ega bo'lmagan xomilalarda taxyzoitlar keng tarqalib, sezilarli darajada asab kasalliklariga olib kelishi mumkin.[30]
Parazitning tirik qolishi xo’jayinning omon qolishi va parazitlarning tarqalishi o’rtasidagi muvozanatga bog’liq.[32] T. gondii bu muvozanatni xo’jayinning immunitet reaksiyasini boshqarish, xo’jayinning immunitetini kamaytirish va parazitning reproduktiv ustunligini oshirish orqali amalga oshiradi.[32] Oddiy xujayra xujayrasini yuqtirgandan so'ng, u xujayraning immunitet tizimining zararlanishiga qarshi turadi va xujayraning immunitet jarayonlarini o'zgartiradi.
U mezbon hujayraga kirib borishi bilan parazit a hosil qiladi parazitofor vakuol Mezbon hujayra membranasidan (PV) membrana.[2][33] PV parazitni o'z ichiga oladi va ikkalasi ham endolizozomal tizimning ta'siriga chidamli bo'lib, mezbonlarni boshqarishni o'z zimmasiga olishi mumkin. mitoxondriya va endoplazmatik to'r.[2][33]
Hujayrani birinchi marta ishg'ol qilishda parazit lampochkadan ROP oqsillarini chiqaradi roptriya organelle.[2] Ushbu oqsillar faollashishi mumkin bo'lgan PV membranasining yadrosi va yuzasiga o'tadi STAT ning ifodasini modulyatsiya qilish yo'llari sitokinlar transkripsiya darajasida, PV membranasini yo'q qilishni bog'lab qo'ying va inaktiv qiling IRG mumkin bo'lgan boshqa ta'sirlar qatorida oqsillar.[2][33][34] Bundan tashqari, T.ning ayrim shtammlari. gondii GRA15 deb nomlanuvchi oqsilni chiqarib, faollashtirishi mumkin NF-DB yallig'lanishni kuchaytiradigan yo'l sitokin Il-12 immunitetning dastlabki reaktsiyasida, ehtimol parazitning yashirin fazasiga olib keladi.[2] Parazitning ushbu oqsillarni ajratish qobiliyati uning genotipiga bog'liq va uning virulentligiga ta'sir qiladi.[2][34]
Parazit shuningdek, antopoptotik mexanizmga ta'sir qiladi, bu yuqtirilgan xujayra hujayralarining davom etishiga va ko'payishiga imkon beradi. Bitta usul apoptoz qarshilik, masalan, pro-apoptoz effektori oqsillarini buzishdir BAX va BAK.[35] Ushbu oqsillarni buzish uchun, T. gondii oqsillarning konformatsion o'zgarishlarini keltirib chiqaradi, bu esa oqsillarni apoptoz hodisalarini boshlaydigan turli xil uyali bo'linmalarga etkazilishiga yo'l qo'ymaydi. T. gondii ammo apoptoz effektori oqsillarining regulyatsiyasini keltirib chiqarmaydi.[35]
T. gondii shuningdek, boshlash qobiliyatiga ega avtofagiya mezbon hujayralarining.[36] Bu sog'lom, yuqtirilmagan hujayralarning pasayishiga olib keladi va natijada yuqtirgan hujayralarga hujum qilish uchun xost hujayralari kamroq bo'ladi. Vang tomonidan olib borilgan tadqiqotlar va boshq yuqtirilgan hujayralar normal va yuqtirilgan hujayralarda avtofagosomalarning yuqori darajasiga olib borishini aniqlaydi.[36] Ularning tadqiqotlari shuni ko'rsatadiki T. gondii kaltsiyga bog'liq bo'lgan yo'l yordamida mezbon hujayra autofagiyasini keltirib chiqaradi.[36] Boshqa bir tadqiqot shuni ko'rsatadiki, parazit hujayralarni signalizatsiya jarayonlari uchun muhim bo'lgan kaltsiy do'konlaridan chiqadigan kaltsiyga bevosita ta'sir qilishi mumkin.[35]
Yuqoridagi mexanizmlar imkon beradi T. gondii xostda turmoq. Toksoplazmaning ba'zi cheklovchi omillari shundaki, uning xujayra hujayralariga ta'siri kuchsiz immunitet tizimida kuchliroq va miqdorga bog'liq, shuning uchun ko'p sonli T. gondii har bir xujayra uchun yanada qattiq ta'sir qiladi.[37] Uy egasiga ta'siri, shuningdek, mezbon immunitet tizimining kuchiga bog'liq. Immunitetga ega bo'lmagan odamlar odatda og'ir alomatlarni yoki umuman namoyon bo'lmaydilar, o'lim yoki og'ir asoratlar immunitet tanqisligi bo'lgan odamlarni keltirib chiqarishi mumkin.[37]
Parazit uy egasining immunitetini o'zgartirishi mumkinligi sababli, u boshqa patogen tahdidlarga qarshi immunitetga ijobiy yoki salbiy ta'sir ko'rsatishi mumkin.[32] Bunga infektsiyalarga qarshi javoblar kiradi, lekin ular bilan chegaralanmaydi Helicobacter felis, Leyshmaniya mayor, yoki boshqa parazitlar, masalan Nippostrongylus brasiliensis.[32]
Yuqish
Toksoplazmoz odatda og'iz orqali yuqganda Toxoplasma gondii ookistalar yoki to'qima kistalari tasodifan iste'mol qilinadi.[38] Onadan homilaga tug'ma o'tkazuvchanlik ham paydo bo'lishi mumkin.[39] Transmissiya qattiq organ transplantatsiyasi jarayonida ham sodir bo'lishi mumkin[40] yoki gematogen ildiz hujayralari transplantatsiyasi.[41]
Og'iz orqali yuborish quyidagilar orqali sodir bo'lishi mumkin.
- Xom yoki qisman pishirilgan go'shtni, ayniqsa cho'chqa go'shti, qo'zichoq yoki kiyik go'shtini iste'mol qilish Toksoplazma kistalar: an'anaviy ravishda kam pishirilgan go'sht iste'mol qilinadigan mamlakatlarda infektsiyaning tarqalishi ushbu yuqish usuli bilan bog'liq. To'qimalarning kistalari, shuningdek, pishgan go'sht bilan ishlov berishdan keyin yoki pichoq, idish-tovoq yoki xom go'sht bilan ifloslangan taxta plitalarini ishlatishdan keyin og'ziga qo'l bilan tegish paytida yuqishi mumkin.[42]
- Yuqtirilgan mushuklarning najasini o'z ichiga olgan ifloslangan tuproq bilan aloqada bo'lgan yuvilmagan meva yoki sabzavotlarni iste'mol qilish.[43]
- Mushukni yutish najas tarkibida ookistlar mavjud: Bu bog'dorchilik, mushukni tozalashdan keyin og'zaki aloqa orqali sodir bo'lishi mumkin axlat qutisi, bolalar qumtepalari bilan aloqa qilish; parazit atrof muhitda bir necha oy yashashi mumkin.[44]
- To'g'ridan-to'g'ri iste'mol qilish yoki oziq-ovqat tayyorlash uchun suvdan foydalanish orqali tozalanmagan, filtrlanmagan suvni iste'mol qilish.[45]
- Pasterizatsiya qilinmagan sut va sut mahsulotlarini, xususan, echki sutini iste'mol qilish.
- Xom dengiz mahsulotlarini iste'mol qilish.
Mushuklar kasallik qo'zg'atgandan so'ng bir necha hafta davomida qo'zg'atuvchini najas bilan chiqaradi, umuman olganda sutemizuvchilar (kemiruvchilar kabi) yoki qushlarni o'z ichiga olishi mumkin bo'lgan yuqtirilgan oraliq xo'shni iste'mol qiladi. Ookistni to'kish odatda yuqtirilgan oraliq xostlarni qabul qilganidan keyingi uchinchi kundan boshlanadi va bir necha hafta davom etishi mumkin. Ookistalar tashqariga chiqarilganda yuqumli emas. Taxminan bir kundan so'ng, ookist sporulyatsiya deb ataladigan jarayonni boshdan kechiradi va potentsial patogen bo'lib qoladi.[46] Mushuklardan tashqari qushlar va sutemizuvchilar, shu jumladan odam ham parazitning oraliq xosti bo'lib, yuqish jarayonida ishtirok etadi. Ammo patogenligi infektsiya bilan bog'liq bo'lgan yosh va turlarga va yuqish uslubiga qarab farq qiladi T. gondii.[47]
Toksoplazmoz ham qattiq organ transplantatsiyasi orqali yuqishi mumkin. Yaqinda yuqtirilgan toksoplazma-seropozitiv donorlardan organlarni qabul qiladigan toksoplazma-seronegativ retseptorlari xavf ostida. Yashirin toksoplazmozga ega bo'lgan organ retsipientlari, qattiq organ transplantatsiyasi paytida yuzaga kelgan immunosupressiya tufayli kasallik o'z tizimida qayta faollashishi xavfi ostida.[40] Gematogen ildiz hujayralari transplantatsiyasini oluvchilar immunosupressiyaning uzoqroq muddatlari tufayli yuqtirish xavfi yuqori bo'lishi mumkin.[41]
Yurak va o'pka transplantatsiyasi yurakni tashkil etuvchi mushaklari tufayli toksoplazmoz infektsiyasining eng yuqori xavfini keltirib chiqaradi,[40] kistlarni o'z ichiga olishi mumkin, va boshqa organlar va to'qimalar uchun xavf turli xil.[48] Transplantatsiya jarayonidan oldin donorlar va retsipientlarni tekshirib, davolanishni ta'minlash orqali yuqish xavfi kamayishi mumkin.[48]
Homiladorlikning oldini olish choralari
Tug'ma toksoplazmoz - toksoplazmozning o'ziga xos shakli, bunda tug'ilmagan homila platsenta.[49] Tug'ma toksoplazmoz homilaning o'limi va tushishi bilan, chaqaloqlarda esa nevrologik etishmovchilik, neyrokognitiv nuqson va chorioretinit.[6] Ijobiy antikor titr oldingi ta'sirlanish va immunitetni ko'rsatadi va asosan homila xavfsizligini ta'minlaydi. Birinchi tug'ruqdan oldin shifokorga tashrif buyurganingizda oddiy qon olish ayolning avvalgi maruziyetga uchraganligini yoki yo'qligini va shuning uchun u xavf ostida yoki yo'qligini aniqlashi mumkin. Agar ayol o'zining birinchi ta'sirini qabul qilsa T. gondii homiladorlik paytida homila ayniqsa xavf ostida.[6]
Homiladorlikdan oldin tug'ma toksoplazmozning oldini olish bo'yicha ta'limning ta'siri haqida juda ko'p dalillar mavjud emas.[50] Biroq, bola tug'ilishidan oldin ota-onalarga ta'lim berish samarali bo'lishi tavsiya etilgan, chunki u oziq-ovqat, shaxsiy va uy hayvonlari gigienasini yaxshilashi mumkin.[50] Antenatal ta'lim tug'ma toksoplazmozni kamaytirishi mumkinligini aniqlash uchun ko'proq tadqiqotlar o'tkazish kerak.[50]
Antikorlarning salbiy titrlari bo'lgan homilador ayollar uchun, ilgari ta'sir qilmaganligini ko'rsatmoqda T. gondii, Serologni har oyda bo'lgani kabi tez-tez o'tkazib turadigan ayollar uchun homiladorlik paytida davolanish tavsiya etiladi T. gondii birinchi marta homila parazitini yuqtirish xavfini keskin kamaytiradi. Bolaning immuniteti hayotning birinchi yilida to'liq rivojlanmaganligi va butun tanada hosil bo'ladigan elastik kistalarni antiprotozoanlar bilan yo'q qilish juda qiyin bo'lgani uchun, yosh bolalarda infektsiya juda jiddiy bo'lishi mumkin.
Ushbu xavf-xatarlarga qaramay, ko'pgina mamlakatlarda homilador ayollar toksoplazmozni muntazam ravishda tekshiruvdan o'tkazmaydilar, chunki bu iqtisodiy samaradorlik va ularning ko'pligi yolg'on ijobiy hosil bo'lgan; Portugaliya,[51] Frantsiya,[52] Avstriya,[52] Urugvay,[53] va Italiya[54] taniqli istisnolar va ayrim mintaqaviy skrining dasturlari ishlaydi Germaniya, Shveytsariya va Belgiya.[54] Invaziv sifatida tug'ruqdan oldin sinov ba'zi xavfga olib keladi homila (Toksoplazmoz bilan kasallanish uchun 18,5 homiladorlik yo'qolishi oldini oldi),[52] tug'ruqdan keyingi yoki yangi tug'ilgan chaqaloq skrining afzal. Istisno holatlar bu erda homila anormalliklar qayd etiladi va shu tariqa skrining maqsadga muvofiq bo'lishi mumkin.[52]
Homilador ayollar muomaladan qochishlari kerak xom go'sht, ichish xom sut (ayniqsa, echki suti) va turidan qat'i nazar, xom yoki pishmagan go'sht iste'mol qilmaslik tavsiya etiladi.[55] O'rtasidagi aniq munosabatlar tufayli Toksoplazma mushuklarga ko'pincha mushuklarning axlatiga tushmaslik va bog'dorchilikdan voz kechish (bog 'tuprog'ida mushuklarning najasi keng tarqalgan) yoki hech bo'lmaganda qo'lqop kiyish tavsiya etiladi.[55] Ko'pgina mushuklar faol ravishda to'kilmaydi ookistalar, chunki ular hayotlarining dastlabki olti oyida, ootsistlarni qisqa vaqt ichida (1-2 hafta) to'kishganda yuqtirishadi.[56] Ammo, bu ookistlar tuproqqa ko'milib, sporulyatsiya qilinadi va bir necha oydan bir yildan ko'proq vaqtgacha yuqumli bo'lib qoladi.[55] Ko'plab tadqiqotlar shuni ko'rsatdiki, uy sharoitida mushuk bilan yashash muhim xavf omili emas T. gondii infektsiya,[55][57][58] bir nechta mushukchalar bilan yashash ba'zi ahamiyatga ega.[59]
2006 yilda Chexiya tadqiqot guruhi[60] yuqori darajadagi toksoplazmoz antikorlari bo'lgan ayollarning o'g'il tug'ilishi qiz bolalarga qaraganda ancha yuqori bo'lgan. Ko'pgina populyatsiyalarda tug'ilish koeffitsienti o'g'il bolalarning 51 foizini tashkil qiladi, ammo yuqtirgan ayollar T. gondii o'g'il bolani topish ehtimoli 72% gacha bo'lgan.[61]
Tashxis
Odamlarda toksoplazmoz diagnostikasi biologik, serologik, gistologik yoki molekulyar usullar bilan yoki yuqorida aytilganlarning kombinatsiyasi bilan amalga oshiriladi.[56] Toksoplazmozni ajratish qiyin bo'lishi mumkin birlamchi markaziy asab tizimining limfomasi. U bir nechta boshqa yuqumli kasalliklarni taqlid qiladi, shuning uchun klinik belgilar o'ziga xos emas va aniq tashxis qo'yish uchun etarli darajada xarakterli emas. Natijada, tashxis terapiya sinovi orqali aniqlanadi (pirimetamin, sulfadiazin va folin kislotasi (USAN: leykovorin)), agar dorilar klinik ta'sir ko'rsatmasa va takroriy tasvirlashda yaxshilanish bo'lmasa.
T. gondii da aniqlanishi mumkin qon, amniotik suyuqlik, yoki miya omurilik suyuqligi yordamida polimeraza zanjiri reaktsiyasi.[62] T. gondii xostda, ehtimol aniqlashdan qochib ketadigan, harakatsiz kist sifatida mavjud bo'lishi mumkin.
Serologik sinov aniqlay oladi T. gondii usullarini qo'llagan holda qon zardobidagi antikorlar Sabin - Feldman bo'yoq sinovi (DT), bilvosita gemaglutinatsiyani tahlil qilish, bilvosita lyuminestsent antikorlarni tahlil qilish (IFA), to'g'ridan-to'g'ri aglutinatsiya testi, lateks aglutinatsiya testi (LAT), ferment bilan bog'liq immunosorbent tahlil (Elishay) va immunosorbentli aglutinatsiyani tahlil qilish testi (IAAT).[56]
O'lchash uchun eng ko'p ishlatiladigan testlar IgG antikor DT, Elishay, IFA va o'zgartirilgan to'g'ridan-to'g'ri aglutinatsiya testidir.[63] IgG antikorlari odatda infektsiyadan bir-ikki hafta ichida paydo bo'ladi, bir oydan ikki oygacha avjiga chiqadi, so'ngra har xil tezlikda pasayadi.[63] Toksoplazma IgG antikorlari odatda umr bo'yi saqlanib qoladi va shuning uchun qonda mavjud yoki oldingi infektsiya natijasida bo'lishi mumkin.[64]
Ba'zi darajada o'tkir toksoplazmoz infektsiyalari surunkali infektsiyalardan IgG yordamida farqlanishi mumkin avidlik sinov, bu Elishayning o'zgarishi. Infektsiyaga birinchi javobda toksoplazmadagi o'ziga xos IgG toksoplazma antigeniga nisbatan yaqinligi past; keyingi haftalarda va oyda IgG antigenga yaqinligi oshadi. IgG avidligi testiga asoslanib, agar yuqtirgan odamda IgG yuqori yaqinlikka ega bo'lsa, demak, infektsiya sinovdan uch-besh oy oldin boshlangan. Bu, ayniqsa, tug'ruq infektsiyasida foydalidir, bu erda homiladorlik holati va homiladorlik paytida homiladorlik davri davolanishni belgilaydi.[65]
IgG dan farqli o'laroq, IgM antikorlari o'tkir infektsiyani aniqlash uchun ishlatilishi mumkin, ammo umuman surunkali infektsiyani emas.[64] IgM antikorlari infektsiyadan keyin IgG antikorlariga qaraganda tezroq paydo bo'ladi va tiklanishdan keyin IgG antikorlariga qaraganda tezroq yo'qoladi.[56] Ko'p hollarda, T. gondii- o'ziga xos IgM antikorlari dastlab birlamchi infektsiyani olgandan keyin taxminan bir hafta o'tgach aniqlanishi va bir oydan olti oygacha kamayishi mumkin; Yuqtirilganlarning 25% salbiy hisoblanadi T. gondii- etti oy ichida maxsus IgM.[64] Shu bilan birga, IgM infektsiyadan bir necha oy yoki bir necha yil o'tgach, surunkali bosqichda aniqlanishi mumkin va o'tkir infektsiya uchun noto'g'ri ijobiy holatlar bo'lishi mumkin.[63] IgM antikorini o'lchash uchun eng ko'p ishlatiladigan testlar IgM-ELISA juft sendvichi, IFA testi va immunosorbentli aglutinatsiya tahlili (IgM-ISAGA). Tijorat test to'plamlari ko'pincha o'ziga xos xususiyatlarga ega va hisobot natijalari ko'pincha noto'g'ri talqin etiladi.[63]
Tug'ma
Tug'ma toksoplazmozni aniqlash bo'yicha tavsiyalar quyidagilarni o'z ichiga oladi: testlar asosida prenatal tashxis amniotik suyuqlik va ultratovush tekshiruvlari; platsentaning molekulyar tekshiruviga asoslangan yangi tug'ilgan diagnostika va ichak qoni va ona-bola qiyosiy serologik tekshiruvlari va tug'ilish paytida klinik tekshiruv; va asosida erta bolalikni tashxislash nevrologik va oftalmologik hayotning birinchi yilida tekshiruvlar va serologik tekshiruv.[49] Homiladorlik davrida serologik tekshiruvni uch hafta oralig'ida o'tkazish tavsiya etiladi.[66]
Toksoplazmoz tashxisi juda aniq anti-serologik aniqlashga bog'liq bo'lsa hamToksoplazma immunoglobulin, serologik tekshiruv cheklovlarga ega. Masalan, ning faol fazasini aniqlay olmasligi mumkin T. gondii yuqumli kasallik, chunkiToksoplazma IgG yoki IgM infektsiyadan bir necha hafta o'tgach ishlab chiqarilmasligi mumkin. Natijada, homilador ayol faol bosqichida salbiy tekshiruv o'tkazishi mumkin T. gondii aniqlanmagan va shuning uchun davolanmagan tug'ma toksoplazmozga olib keladigan infektsiya.[67] Shuningdek, test aniqlanmasligi mumkin T. gondii immunitet tanqisligi bo'lgan bemorlarning infektsiyalari, chunki o'ziga xos anti-titrlarToksoplazma Ushbu turdagi bemorlarda IgG yoki IgM ko'tarilmasligi mumkin.
Amniotik suyuqlikni o'z ichiga olgan klinik namunalar yordamida toksoplazmozni tashxislash uchun ko'plab PCR asosidagi metodlar ishlab chiqilgan, qon, miya omurilik suyuqligi va to'qima biopsiyasi. PCR asosidagi eng sezgir texnika ichki PCR keyin PCR mahsulotlarini duragaylash.[67] Ushbu texnikaning asosiy salbiy tomoni shundaki, ular ko'p vaqt talab etadi va miqdoriy ma'lumot bermaydi.[67]
Haqiqiy vaqtda PCR patogenni aniqlashda, genlarning ekspressioni va regulyatsiyasi va allelik kamsitilishida foydalidir. Ushbu PCR texnikasi 5 'nukleaza faolligidan foydalanadi Taq PCR kengayish bosqichida keraksiz, lyuminestsentsiya bilan belgilangan gibridlanish zondini ajratish uchun DNK-polimeraza.[67] Ikkinchi lyuminestsent bo'yoq, masalan, 6-karboksi-tetrametil-rodamin, buzilmagan probning lyuminestsentsiyasini o'chiradi.[67] PCR paytida duragaylash naychasining nukleazli bo'linishi, ketma-ketlikni aniqlash vositasi bilan kuzatilishi mumkin bo'lgan PCR mahsuloti miqdoriga mutanosib lyuminestsentsiyaning ko'payishiga olib keladigan söndürme ta'sirini chiqaradi.[67]
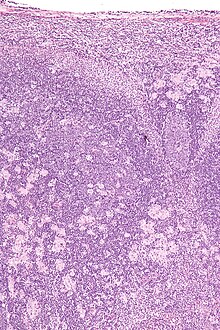
Toksoplazmozni aniqlab bo'lmaydi immunostaining. Ta'sir qilingan limfa tugunlari Toksoplazma xarakterli o'zgarishlarga ega, shu jumladan yomon chegaralangan reaktiv germinal markazlar, monotsitoid B hujayralari klasterlari va tarqoq epiteliyoid histiositlar.
Tug'ma toksoplazmozning klassik uchligiga quyidagilar kiradi. chorioretinit, gidrosefali va intrakranial arterioskleroz.[68] Boshqa oqibatlarga sensorinevral karlik, tutqanoq va aqliy qobiliyatsizlik kiradi.[69]
Tug'ma toksoplazmoz ham bolaning eshitish qobiliyatiga ta'sir qilishi mumkin. Yangi tug'ilgan chaqaloqlarning 30 foizigacha eshitish qobiliyati ma'lum darajada sensorinevral tarzda yo'qoladi.[70] Bolaning muloqot qobiliyatlari ham ta'sir qilishi mumkin. 2010 yilda nashr etilgan tadqiqotda 106 bemor ko'rib chiqildi, ularning barchasi 2,5 oydan oldin toksoplazmoz bilan davolangan. Ushbu guruhdan 26,4% til buzilishi bilan murojaat qilgan.[71]
Davolash
Davolash ko'pincha jiddiy sog'liq muammolari bo'lgan odamlar uchun tavsiya etiladi, masalan OIV kimning CD4 hisoblagichlar 200 mm / mm dan past3, chunki kasallik odamning immuniteti zaif bo'lganida eng jiddiy hisoblanadi. Trimetoprim / sulfametoksazol bu toksoplazmozni oldini olish uchun tanlangan dori, ammo faol kasallikni davolash uchun emas. 2012 yildagi tadqiqot ushbu kasallikning faol va yashirin shaklini ikki usul yordamida davolashning istiqbolli yangi usulini ko'rsatadi. endoxinga o'xshash kinolonlar.[72]
O'tkir
O'tkir toksoplazmoz uchun buyurilgan dorilar quyidagilar:
- Pirimetamin - bir bezgakka qarshi dori
- Sulfadiazin - bir antibiotik toksoplazmozni davolash uchun pirimetamin bilan birgalikda ishlatiladi
- Kombinatsiyalangan terapiya odatda insidansni kamaytirish uchun foliy kislotasi qo'shimchalari bilan amalga oshiriladi trombotsitopeniya.
- Kombinatsiyalangan terapiya OIV kasalligida eng foydali hisoblanadi.
- Klindamitsin[73]
- Spiramitsin - homilador ayollar uchun ko'pincha bolalariga yuqtirishni oldini olish uchun ishlatiladigan antibiotik.
(boshqa antibiotiklar, masalan minosiklin, ba'zi bir foydalanishni a sifatida ko'rgan qutqarish terapiyasi ).
Agar homiladorlik paytida yuqtirilsa, piramitamin / sulfadiazin va birinchi trimestrda spiramitsin tavsiya etiladi. leykovorin ikkinchi va uchinchi trimestrlarning oxirida tavsiya etiladi.[74]
Yashirin
Yashirin toksoplazmoz bilan kasallangan odamlarda kistalar ushbu davolash usullariga qarshi immunitetga ega, chunki antibiotiklar bradizoidlar etarli konsentratsiyada.
Yashirin toksoplazmoz uchun buyurilgan dorilar:
- Atovakuone - o'ldirish uchun ishlatilgan antibiotik Toksoplazma ichidagi kistalar OITS bemorlar[75]
- Klindamitsin - bu bilan birga bo'lgan antibiotik atovaquone, sichqonlardagi kistalarni optimal tarzda yo'q qilganday tuyuldi[76]
Tug'ma
Homilador ayolga o'tkir toksoplazmoz tashxisi qo'yilganda, amniyosentez yordamida homila yuqtiriladimi yoki yo'qligini aniqlash mumkin. Homilador ayolda o'tkir toksoplazmoz paydo bo'lganda, taxizoidlar platsenta to'qimalariga kirish ehtimoli taxminan 30% ni tashkil qiladi va u erdan homilaga kirib, uni yuqtiradi. INFEKTSION paytida homiladorlik muddati oshgani sayin, homila yuqtirish ehtimoli ham oshadi.[30]
Agar parazit hali homilaga etib bormagan bo'lsa, spiramitsin platsenta yuqishini oldini olishga yordam beradi. Agar homila yuqtirgan bo'lsa, homilador ayolni davolash mumkin pirimetamin va sulfadiazin, bilan folin kislotasi, birinchi trimestrdan keyin. Ular birinchi trimestrdan keyin davolanadi, chunki pirimetamin antifolat ta'siriga ega va foliy kislotasining etishmasligi xalaqit berishi mumkin xomilalik miyaning shakllanishi va sabab trombotsitopeniya.[77] Homiladorlikning oldingi bosqichlarida yuqtirish homilaning va neonatalning yomon natijalari bilan, ayniqsa infektsiya davolanmagan bo'lsa, o'zaro bog'liqdir.[78]
Tug'ilgandan keyingi 12 oylik toksoplazmozga qarshi davolanishni o'tkazgan yangi tug'ilgan chaqaloqlarda sensorinevral eshitish qobiliyati past bo'ladi.[79] Ushbu guruh uchun tug'ma toksoplazmoz bilan kasallangan bolalarni davolash bosqichlari haqida ma'lumot yaratilgan.[80]
Epidemiologiya
T. gondii infektsiyalar butun dunyo bo'ylab ro'y beradi, ammo infektsiya darajasi mamlakatlar bo'yicha sezilarli darajada farq qiladi.[24] Bola tug'ish yoshidagi ayollar uchun 44 ta mamlakat bo'yicha o'tkazilgan 99 ta tadqiqotlar natijasida o'tkazilgan so'rov natijalariga ko'ra eng ko'p tarqalgan joylar mavjud lotin Amerikasi (taxminan 50-80%), qismlari Sharqiy va Markaziy Evropa (taxminan 20-60%), Yaqin Sharq (taxminan 30-50%), qismlari Janubi-sharqiy Osiyo (taxminan 20-60%) va uning qismlari Afrika (taxminan 20-55%).[24]
In Qo'shma Shtatlar, ma'lumotlar Milliy sog'liqni saqlash va ovqatlanishni o'rganish bo'yicha so'rov (NHANES) 1999 yildan 2004 yilgacha AQShda tug'ilgan 12-49 yoshdagi odamlarning 9,0% ni tashkil qildi seropozitiv uchun IgG antikorlar qarshi T. gondii, 1988-1994 yillarda NHANESda o'lchangan 14,1% dan past.[81] 1999-2004 yillarda o'tkazilgan so'rovda AQShda tug'ilganlarning 7,7% va 15-44 yoshdagi chet elda tug'ilgan ayollarning 28,1%. T. gondii seropozitiv.[81] Kamayish tendentsiyasi seroprevalans Qo'shma Shtatlar va ko'plab Evropa mamlakatlarida o'tkazilgan ko'plab tadqiqotlar tomonidan kuzatilgan.[24] Toksoplazma gondii ikkinchi sababdir oziq-ovqat - Qo'shma Shtatlarda o'lim va oziq-ovqat bilan bog'liq kasalxonaga yotqizishning to'rtinchi sababi.[82]
Toksoplazmoz uchun javobgar protist T. gondii. Butun dunyoda toksoplazmoz kasalliklari uchun javob beradigan uchta asosiy T. gondii turi mavjud. I, II va III turlari mavjud. Ushbu uch turdagi T. gondii genotiplarining xilma-xilligi tufayli ma'lum xostlarga, asosan sichqonlarga va odamlarga turlicha ta'sir ko'rsatadi.[83]
- I toifa: sichqonlar va odamlarda virusli OITS bilan kasallangan odamlar.
- II tip: sichqonlarda zararli emas, odamlarda (asosan Evropa va Shimoliy Amerika), OITS bilan kasallangan odamlarda uchraydi.
- III tur: sichqonlarda zararli emas, asosan hayvonlarda zararli, ammo odamlarda ham ozroq darajada kuzatiladi.
Joriy serotiplash texnikalar faqat II yoki II tipdagi parazitlarni ajratishi mumkin.[84]
Parazit homiladorlik paytida yuqtirilganda homila uchun alohida xavf tug'diradi,[85] global miqyosda epidemiologik bilan bog'liq ma'lumotlar T. gondii tug'ish yoshidagi ayollarda seropozitivlik testlaridan kelib chiqadi. Seropozitivlik testlari antitellarning mavjudligini tekshiradi T. gondii qonda, shuning uchun seropozitivlik parazitga duchor bo'lishini kafolatlasa-da, uning surunkali yuqishini kafolatlamaydi.[86]
Tarix
Toxoplasma gondii birinchi marta 1908 yilda Tunisda Nikol va Manceoux tomonidan, Braziliyada esa Splendore tomonidan mustaqil ravishda tasvirlangan.[10] Splendore xabar berdi protozoan quyonda, Nikol va Mansaux buni Shimoliy Afrikadagi kemiruvchida, gundi (Ctenodactylus gundi ).[38] 1909 yilda Nikol va Mansa protozoyani farqlashdi Leyshmaniya.[10] Keyin Nikoll va Manceuux ism berishdi Toxoplasma gondii uning yuqumli bosqichining egri shaklidan keyin (yunoncha ildiz 'toxon' = kamon).[10]
Birinchi tug'ma toksoplazmoz kasalligi 1923 yilda qayd etilgan, ammo u sabab bo'lganligi aniqlanmagan T. gondii.[38] Yanki (1923) kasalxonaga murojaat qilgan 11 oylik bolaning otopsi natijalarini batafsil bayon qildi gidrosefali. Bolada toksoplazmozning klassik belgilari bor edi, shu jumladan chorioretinit (koroid va ko'zning to'r pardasi yallig'lanishi).[38] Gistologiya bir qator "sporotsitlar" ni aniqladi, ammo Janko ularni aniqlamadi T. gondii.[38]
Faqat 1937 yilgacha birinchi batafsil ilmiy tahlil qilingan T. gondii viruslarni tahlil qilish uchun ilgari ishlab chiqilgan texnikalar yordamida amalga oshirildi.[10] 1937 yilda Sabin va Olitskiy tahlil qildilar T. gondii laboratoriya maymunlari va sichqonlarida. Sabin va Olitskiy buni ko'rsatdilar T. gondii majburiy hujayra ichidagi parazit bo'lib, sichqonlar ovqatlanardi T. gondii- yuqtirilgan to'qima ham infektsiyani yuqtirgan.[10] Shunday qilib Sabin va Olitskiy namoyish qildilar T. gondii kabi patogen hayvonlar orasida o'tkazuvchan.
T. gondii birinchi marta 1939 yilda inson patogenasi sifatida tasvirlangan Chaqaloqlar kasalxonasi yilda Nyu-York shahri.[10][87] Bo'ri, Koven va Peyj aniqlandi T. gondii tug'ruqdan oldin tug'ilgan chaqaloqdagi infektsiya Kesariya Bo'lim.[38] Kichkintoyda tutilishlar rivojlanib, uch kun davomida ikkala ko'zida ham chorioretinit bor edi. Keyin chaqaloq ensefalomiyelitni rivojlantirdi va bir oyligida vafot etdi. Bo'ri, Koven va Peyj izolyatsiya qilingan T. gondii miya to'qimalarining shikastlanishlaridan. Sichqonlarga, quyonlarga va kalamushlarga miya va orqa miya namunalarini intrakranial ravishda yuborish hayvonlarda ensefalitni keltirib chiqardi.[10] Wolf, Cowen and Page qo'shimcha ishlarni ko'rib chiqdilar va shunday xulosaga kelishdi T. gondii taniqli alomatlar paydo bo'ldi va onadan bolaga yuqishi mumkin edi.[38]
Birinchi kattalarda toksoplazmoz kasalligi 1940 yilda qayd etilgan bo'lib, unda nevrologik belgilar mavjud emas. Pinkerton va Vaynman borligi haqida xabar berishdi Toksoplazma keyingi bakterial infeksiya va isitmadan vafot etgan Perudan kelgan 22 yoshli yigitda.[38]
1948 yilda Sabin va Feldman tomonidan bemorning antikorlari binoni o'zgartirish qobiliyati asosida serologik bo'yoq testi yaratildi. Toksoplazma.[10][88] Sabin Feldman Bo'yoq sinovi endi identifikatsiyalash uchun oltin standart hisoblanadi Toksoplazma infektsiya.[10]
Uzatish Toksoplazma xom yoki pishmagan go'shtni iste'mol qilish orqali Desmonts va boshq. 1965 yilda Parij.[10] Desmonts a-da xom mol yoki ot go'shtining terapevtik iste'mol qilinishini kuzatdi sil kasalligi kasalxona yiliga 50% o'sishi bilan bog'liq edi Toksoplazma antikorlar.[10] Bu shuni anglatadiki, ko'proq T. gondii xom go'sht orqali yuqtirilayotgandi.
1974 yilda Desmonts va Couvreur dastlabki ikki trimestrda infektsiya homila uchun eng katta zarar etkazishini, yuqtirish onalarning homiladorlik paytida yuqtirganiga bog'liqligini, homiladorlikdan oldin antikorlari bo'lgan onalar homilaga yuqtirmaganligini va spiramitsin homilaga uzatishni pasaytirdi.[38]
Toksoplazma 1970-yillarda organlar yoki suyak iligi transplantatsiyasidan so'ng immunitetni bostiruvchi davo kuchayishi va OITS 1980-yillarning epidemiyasi.[10] Immunitet tizimi pasaygan bemorlar kasallikka juda moyil.
Jamiyat va madaniyat
"Telba mushuk-xonim"
"Aqlsiz mushuk-xonim sindromi" - bu parazitni bog'laydigan ilmiy natijalarni tavsiflovchi yangiliklar tashkilotlari tomonidan kiritilgan atama Toxoplasma gondii bir nechtasiga ruhiy kasalliklar va yurish-turish muammolari.[89][90] Bolalikda mushukka egalik qilish va keyinchalik rivojlanishi o'rtasidagi shubhali korrelyatsiya shizofreniya bolalar uchun xavf omilini aniqlash uchun qo'shimcha tadqiqotlar o'tkazish zarurligini ta'kidladi;[91] ammo, keyingi tadqiqotlar shuni ko'rsatdiki T. gondii keyingi psixozlarda sababchi omil bo'lmagan.[92] Tadqiqotchilar mushuk egaligi a xavfini keskin oshirmasligini ham aniqladilar T. gondii homilador ayollarda infektsiya.[55][93]
Atama aqldan ozgan mushuk-ayol sindromi stereotip va mashhur madaniy ma'lumotlarga asoslanadi. Bu xalq orasida yuqorida aytib o'tilgan azob-uqubatlar qayd etilgani sababli paydo bo'ldi. A mushuk ayol ayolning madaniy stereotipidir, ko'pincha a spinster, majburiy ravishda kim xazinalar va mushuklarga nuqta. Biolog Jaroslav Flegr toksoplazmoz inson xatti-harakatlariga ta'sir qiladi degan nazariyaning tarafdoridir.[94][95]
E'tiborga loyiq holatlar
- Tennischi Artur Ashe toksoplazmozdan kelib chiqqan nevrologik muammolar (va keyinchalik aniqlandi) OIV -ijobiy).[96]
- Aktyor Merritt Butrik OIV bilan kasallangan va immun tizimining zaiflashishi natijasida toksoplazmozdan vafot etgan.[97]
- Pedro Zamora, haqiqatan ham televizion shaxs va OIV / OITS faoliga immunitet tizimining OIV bilan zaiflashishi natijasida toksoplazmoz tashxisi qo'yilgan.[98][99]
- Klermont grafligi shahzodasi Fransua, da'vogar uchun Frantsiya taxti tug'ma toksoplazmoz bilan og'rigan; uning nogironligi uni merosxo'rlik qatorida e'tibordan chetda qoldirishiga olib keldi.
- Aktrisa Lesli Ash homiladorlikning ikkinchi oyida toksoplazmoz bilan kasallangan.[100]
- O'rta masofaga ingliz yuguruvchisi Sebastian Koe 1983 yilda toksoplazmoz bilan kasallangan bo'lib, uni Italiyada o'qiyotgan paytida mushuk yuqtirgan.[101][102]
- Tennischi Martina Navratilova davomida toksoplazmoz bilan kasallangan 1982 yil US Open.[103]
Boshqa hayvonlar
Garchi T. gondii deyarli barcha issiq qonli hayvonlarni yuqtirish qobiliyatiga ega, yuqtirishga moyilligi va darajasi turli xil darajada farq qiladi avlodlar va turlari.[106][107] Xuddi shu turdagi populyatsiyalarda yuqtirish darajasi, joylashishi, ovqatlanish tartibi va boshqa omillarning farqi tufayli ham keng farq qilishi mumkin.
Garchi infektsiya T. gondii Osiyo primatlarining seroprevalentligi bir nechta turlarida qayd etilgan T. gondii birinchi marta tokat makakalarida antitellar topildi (Macaca sinica ) Shri-Lanka oroliga xosdir.[108]
Avstraliyalik marsupials ayniqsa toksoplazmozga sezgir.[109] Wallabies, koalalar, Wombats, akademiklar va kichik dasyuridlar tomonidan o'ldirilishi mumkin, bilan sharqiy taqiqlangan bandiklar odatda infektsiyadan taxminan 3 hafta ichida vafot etadi.[110]
Dunyo bo'ylab yovvoyi cho'chqalarning 23% seropozitiv hisoblanadi T. gondii.[111] Seroprevalans butun dunyoda o'zgarib turadi, eng yuqori seroprevalans Shimoliy Amerika (32%) va Evropada (26%), eng pasti Osiyoda (13%) va Janubiy Amerikada (5%).[111] Yuqori kengliklarda joylashgan va issiq, nam iqlimga ega bo'lgan geografik mintaqalar seroprevalentlikning oshishi bilan bog'liq. T. gondii yovvoyi cho'chqa orasida.[111] Yovvoyi cho'chqa yuqtirgan T. gondii go'shtini iste'mol qiladigan odamlar uchun salomatlikka xavf tug'dirishi mumkin.[111]
Chorvachilik
Ular orasida chorva mollari, cho'chqalar, qo'ylar[112] and goats have the highest rates of chronic T. gondii infektsiya.[113] Ning tarqalishi T. gondii in meat-producing animals varies widely both within and among countries,[113] and rates of infection have been shown to be dramatically influenced by varying farming and management practices.[13] For instance, animals kept outdoors or in bepul environments are more at risk of infection than animals raised indoors or in commercial confinement operations.[13][43]
In the United States, the percentage of pigs harboring viable parasites has been measured (via bioassay in mice or cats) to be as high as 92.7% and as low as 0%, depending on the farm or herd.[43] Surveys of seroprevalence (T. gondii antibodies in blood) are more common, and such measurements are indicative of the high relative seroprevalence in pigs across the world.[114] Along with pigs, sheep and goats are among the most commonly infected livestock of epidemiological significance for human infection.[113] Prevalence of viable T. gondii in sheep tissue has been measured (via bioassay) to be as high as 78% in the United States,[115] and a 2011 survey of goats intended for consumption in the United States found a seroprevalence of 53.4%.[116]
Due to a lack of exposure to the outdoors, chickens raised in large-scale indoor confinement operations are not commonly infected with T. gondii.[13] Free-ranging or backyard-raised chickens are much more commonly infected.[13] A survey of free-ranging chickens in the United States found its prevalence to be 17–100%, depending on the farm.[117] Because chicken meat is generally cooked thoroughly before consumption, poultry is not generally considered to be a significant risk factor for human T. gondii infektsiya.[118]
Although cattle and buffalo can be infected with T. gondii, the parasite is generally eliminated or reduced to undetectable levels within a few weeks following exposure.[13] Tissue cysts are rarely present in buffalo meat or beef, and meat from these animals is considered to be low-risk for harboring viable parasites.[113][43]
Horses are considered resistant to chronic T. gondii infektsiya.[13] However, viable cells have been isolated from US horses slaughtered for export, and severe human toxoplasmosis in France has been epidemiologically linked to the consumption of Qazi.[43][119]
Uy mushuklari
In 1942, the first case of feline toxoplasmosis was diagnosed and reported in a domestic cat in Middletown, NY.[120] The investigators isolated oocysts from feline feces and found that the oocysts could be infectious for up to 12 months in the environment.[121]
The seroprevalence of T. gondii yilda uy mushuklari, worldwide has been estimated to be around 30–40%[122] and exhibits significant geographical variation. In the United States, no official national estimate has been made, but local surveys have shown levels varying between 16% and 80%.[122] A 2012 survey of 445 zotli pet cats and 45 shelter cats in Finlyandiya found an overall seroprevalence of 48.4%,[123] while a 2010 survey of feral cats from Giza, Misr found a seroprevalence rate of 97.4%.[124] Another survey from Colombia recorded seroprevalence of 89.3%, whereas a Chinese study found just a 2.1% prevalence.[106]
T. gondii infection rates in domestic cats vary widely depending on the cats' diets and lifestyles.[125] Yirtqich mushuklar that hunt for their food are more likely to be infected than domestic cats, and naturally also depends on the prevalence of T. gondii-infected prey such as birds and small sutemizuvchilar.[126]
Most infected cats will shed oocysts only once in their lifetimes, for a period of about one to two weeks.[122] This shedding can release millions of oocysts, each capable of spreading and surviving for months.[122] An estimated 1% of cats at any given time are actively shedding oocysts.[13]
It is difficult to control the cat population with the infected oocysts due to lack of an effective vaccine. This remains a challenge in most cases and the programs that are readily available are questionable in efficacy.[127]
Kemiruvchilar
Yuqtirish T. gondii ga ko'rsatildi alter the behavior of mice and rats in ways thought to increase the rodents' chances of being preyed upon by cats.[128][129][130] Infected rodents show a reduction in their innate aversion to cat odors; while uninfected mice and rats will generally avoid areas marked with cat siydik or with cat body odor, this avoidance is reduced or eliminated in infected animals.[128][130][131] Moreover, some evidence suggests this loss of aversion may be specific to feline odors: when given a choice between two yirtqich odors (cat or norka ), infected rodents show a significantly stronger preference to cat odors than do uninfected boshqaruv elementlari.[132][133]
In rodents, T. gondii–induced behavioral changes occur through epigenetic remodeling in neurons associated with observed behaviors;[134][135] for example, it modifies epigenetik metilatsiya to induce hypomethylation of argininli vazopressin -related genes in the medial amygdala to greatly decrease predator aversion.[134][135] Similar epigenetically-induced behavioral changes have also been observed in mouse models of addiction, where changes in the expression of histone-modifying enzymes orqali genlarni nokaut qilish yoki fermentlarni inhibatsiyasi in specific neurons produced alterations in drug-related behaviors.[136][137][138] Keng tarqalgan histone–lysine acetylation in cortical astrotsitlar appears to be another epigenetic mechanism employed by T. gondii.[139][140]
T. gondii-infected rodents show a number of behavioral changes beyond altered responses to cat odors. Rats infected with the parasite show increased levels of activity and decreased neophobic xulq-atvor.[141] Similarly, infected mice show alterations in patterns of harakatlanish and exploratory behavior during experimental tests. These patterns include traveling greater distances, moving at higher speeds, accelerating for longer periods of time, and showing a decreased pause-time when placed in new arenas.[142] Infected rodents have also been shown to have lower tashvish, using traditional models such as elevated plus mazes, open field arenas, and social interaction tests.[142][143]
Dengiz sutemizuvchilar
A Kaliforniya universiteti, Devis study of dead dengiz samurlari collected from 1998 to 2004 found toxoplasmosis was the cause of death for 13% of the animals.[144] Proximity to freshwater outflows into the ocean was a major risk factor. Yutish ookistalar from cat feces is considered to be the most likely ultimate source.[145] Yuzaki suv oqimi containing wild cat feces and litter from domestic cats flushed down toilets are possible sources of oocysts.[146][147] These same sources may have also introduced the toxoplasmosis infection to the endangered Gavayi rohibining muhri.[148] Infection with the parasite has contributed to the death of at least four Hawaiian monk seals.[148] A Hawaiian monk seal's infection with T. gondii was first noted in 2004.[149] The parasite's spread threatens the recovery of this highly endangered pinniped. The parasites have been found in dolphins and whales.[150][151] Researchers Black and Massie believe anchovies, which travel from estuaries into the open ocean, may be helping to spread the disease.[152]
Gigant panda
Toxoplasma gondii has been reported as the cause of death of a ulkan panda kept in a zoo in China, who died in 2014 of acute gastroenterit va nafas olish kasalligi.[105] Aftidan latif, this report emphasizes that all warm-blooded species are likely to be infected by T. gondii, including endangered species such as the giant panda.
Tadqiqot
Surunkali infektsiya T. gondii has traditionally been considered asemptomatik in people with normal immune function.[153] Some evidence suggests latent infection may subtly influence a range of human behaviors and tendencies, and infection may alter the susceptibility to or intensity of a number of psixiatrik or neurological disorders.[154][153]
In most of the current studies where positive correlations have been found between T. gondii antibody titers and certain behavioral traits or neurological disorders, T. gondii seropositivity tests are conducted after the onset of the examined disease or behavioral trait; that is, it is often unclear whether infection with the parasite increases the chances of having a certain trait or disorder, or if having a certain trait or disorder increases the chances of becoming infected with the parasite.[155] Groups of individuals with certain behavioral traits or neurological disorders may share certain behavioral tendencies that increase the likelihood of exposure to and infection with T. gondii; as a result, it is difficult to confirm causal relationships between T. gondii infections and associated neurological disorders or behavioral traits.[155]
Ruhiy salomatlik
Some evidence links T. gondii ga shizofreniya.[153] Two 2012 meta-analyses found that the rates of antikorlar ga T. gondii in people with schizophrenia were 2.7 times higher than in controls.[156][157] T. gondii antibody positivity was therefore considered an intermediate risk factor in relation to other known risk factors.[156] Cautions noted include that the antibody tests do not detect toxoplasmosis directly, most people with schizophrenia do not have antibodies for toxoplasmosis, and nashr tarafkashligi mavjud bo'lishi mumkin.[157] While the majority of these studies tested people already diagnosed with schizophrenia for T. gondii antibodies, associations between T. gondii and schizophrenia have been found prior to the onset of schizophrenia symptoms.[128] Sex differences in schizophrenia onset may be explained by a second peak of T. gondii infection incidence during ages 25–30 in females only.[158] Although a mechanism supporting the association between schizophrenia and T. gondii infection is unclear, studies have investigated a molecular basis of this correlation.[158] Antipsikotik dorilar used in schizophrenia appear to inhibit the replication of T. gondii tachyzoites in cell culture.[128] Supposing a causal link exists between T. gondii and schizophrenia, studies have yet to determine why only some individuals with latent toxoplasmosis develop shizofreniya; some plausible explanations include differing genetic susceptibility, parasite strain differences, and differences in the route of the acquired T. gondii infektsiya.[159]
Correlations have also been found between antibody titrlar ga T. gondii va OKB, o'z joniga qasd qilish in people with mood disorders including bipolyar buzilish.[154][160] Positive antibody titers to T. gondii appear to be uncorrelated with katta depressiya yoki distimiya.[161] Although there is a correlation between T. gondii and many psychological disorders, the underlying mechanism is unclear. A 2016 study of 236 persons with high levels of Toxoplasmosis antibodies found that "there was little evidence that T. gondii was related to increased risk of psychiatric disorder, poor impulse control, personality aberrations or neurocognitive impairment".[162]
Asab kasalliklari
Latent infection has been linked to Parkinson kasalligi va Altsgeymer kasalligi.[154]
There is a negative association between an infection with the parasite T. gondii va skleroz; researchers have concluded that toxoplasmosis infection may be a protective factor.[163]
Traffic accidents
Yashirin T. gondii infection in humans has been associated with a higher risk of avtohalokatlar, potentially due to impaired psixomotor performance or enhanced risk-taking personality profiles.[154]
Iqlim o'zgarishi
Climate change has been reported to affect the occurrence, survival, distribution and transmission of T. gondii.[164] T. gondii has been identified in the Canadian arctic, a location that was once too cold for its survival.[165] Higher temperatures increase the survival time of T. gondii.[164] More snowmelt and precipitation can increase the amount of T. gondii oocysts that are transported via river flow.[164] Shifts in bird, rodent, and insect populations and migration patterns can impact the distribution of T. gondii due to their role as reservoir and vector.[164] Urbanization and natural environmental degradation are also suggested to affect T. gondii transmission and increase risk of infection.[164]
Shuningdek qarang
Adabiyotlar
- ^ a b v d e "Parasites – Toxoplasmosis (Toxoplasma infection) Disease". 2014 yil 10-iyul. Arxivlandi asl nusxasidan 2015 yil 22 avgustda. Olingan 22 avgust 2015.
- ^ a b v d e f g h Hunter, CA; Sibley, LD (November 2012). "Modulation of innate immunity by Toxoplasma gondii virulence effectors". Tabiat sharhlari Mikrobiologiya. 10 (11): 766–78. doi:10.1038/nrmicro2858. PMC 3689224. PMID 23070557.
- ^ a b v d e f g "Parasites – Toxoplasmosis (Toxoplasma infection) Epidemiology & Risk Factors". 2015 yil 26 mart. Arxivlandi asl nusxasidan 2015 yil 23 avgustda. Olingan 22 avgust 2015.
- ^ a b "Parasites – Toxoplasmosis (Toxoplasma infection) Diagnosis". 2013 yil 10-yanvar. Arxivlandi asl nusxasidan 2015 yil 22 avgustda. Olingan 22 avgust 2015.
- ^ a b v "Parasites – Toxoplasmosis (Toxoplasma infection) Resources for Health Professionals". 2014 yil 14 aprel. Arxivlandi asl nusxasidan 2015 yil 13 sentyabrda. Olingan 22 avgust 2015.
- ^ a b v d Torgerson, Paul R; Mastroiacovo, Pierpaolo (2013). "The global burden of congenital toxoplasmosis: a systematic review". Jahon sog'liqni saqlash tashkilotining Axborotnomasi. 91 (7): 501–508. doi:10.2471/BLT.12.111732. ISSN 0042-9686. PMC 3699792. PMID 23825877.
- ^ a b v d e Flegr J, Prandota J, Sovicková M, Israili ZH (mart 2014). "Toksoplazmoz - global tahdid. 88 mamlakatlar qatorida yashirin toksoplazmozning o'ziga xos kasallik yuki bilan o'zaro bog'liqligi". PLOS ONE. 9 (3): e90203. Bibcode:2014PLoSO...990203F. doi:10.1371 / journal.pone.0090203. PMC 3963851. PMID 24662942.
Toxoplasmosis is becoming a global health hazard as it infects 30–50% of the world human population.
- ^ a b "Parasites – Toxoplasmosis (Toxoplasma infection) Biology". 2015 yil 17 mart. Arxivlandi asl nusxasidan 2015 yil 28 avgustda. Olingan 22 avgust 2015.
- ^ a b "Parasites – Toxoplasmosis (Toxoplasma infection) Prevention & Control". 2013 yil 10-yanvar. Arxivlandi asl nusxasidan 2015 yil 22 avgustda. Olingan 22 avgust 2015.
- ^ a b v d e f g h men j k l m n Ferguson DJ (2009). "Toxoplasma gondii: 1908–2008, homage to Nicolle, Manceaux and Splendore". Memórias do Instituto Oswaldo Cruz. 104 (2): 133–48. doi:10.1590/S0074-02762009000200003. PMID 19430635.
- ^ Tyebji, S; Seizova, S; Hannan, AJ; Tonkin, CJ (January 2019). "Toxoplasmosis: A pathway to neuropsychiatric disorders". Neyrologiya va biobehavioral sharhlar. 96: 72–92. doi:10.1016/j.neubiorev.2018.11.012. PMID 30476506. S2CID 53726244.
- ^ a b Dupont CD, Christian DA, Hunter CA (2012). "Immune response and immunopathology during toxoplasmosis". Immunopatologiya bo'yicha seminarlar. 34 (6): 793–813. doi:10.1007/s00281-012-0339-3. PMC 3498595. PMID 22955326.
- ^ a b v d e f g h men Dubey JP, Jones JL (September 2008). "Toxoplasma gondii infection in humans and animals in the United States". Xalqaro parazitologiya jurnali. 38 (11): 1257–78. doi:10.1016/j.ijpara.2008.03.007. PMID 18508057.
- ^ a b "toxoplasmosis". Arxivlandi from the original on 2015-09-08.
- ^ Jones JL, Kruszon-Moran D, Wilson M, McQuillan G, Navin T, McAuley JB (2001). "Toxoplasma gondii infection in the United States: seroprevalence and risk factors". Amerika Epidemiologiya jurnali. 154 (4): 357–65. doi:10.1093/aje/154.4.357. PMID 11495859.
- ^ Paul M (1 July 1999). "Immunoglobulin G Avidity in Diagnosis of Toxoplasmic Lymphadenopathy and Ocular Toxoplasmosis". Klinika. Tashxis. Laboratoriya laboratoriyasi. Immunol. 6 (4): 514–8. doi:10.1128/CDLI.6.4.514-518.1999. PMC 95718. PMID 10391853.
- ^ "Lymphadenopathy" (PDF). UK Neqas Micro. Arxivlandi (PDF) from the original on 2016-04-24. Olingan 2016-04-12.
- ^ "CDC Parasites – Toxoplasmosis (Toxoplasma infection) – Disease". Arxivlandi asl nusxasidan 2013 yil 7 martda. Olingan 12 mart 2013.
- ^ Dubey JP, Hodgin EC, Hamir AN (2006). "Acute fatal toxoplasmosis in squirrels (Sciurus carolensis) with bradyzoites in visceral tissues". Parazitologiya jurnali. 92 (3): 658–9. doi:10.1645/GE-749R.1. PMID 16884019. S2CID 20384171.
- ^ Nawaz Khan, A (2015). "Imaging in CNS Toxoplasmosis". Medscape Web Site.
- ^ a b Blanchard N, Dunay IR, Schlüter D (2015). "Persistence of Toxoplasma gondii in the central nervous system: a fine-tuned balance between the parasite, the brain and the immune system". Parazit immunologiyasi. 37 (3): 150–158. doi:10.1111/pim.12173. PMID 25573476. S2CID 1711188.
The seroprevalence of T. gondii in humans varies between 10 and 70% worldwide, depending on the region and increases significantly with age. Upon infection, the parasites persist as intraneuronal cysts in the central nervous system (CNS) for the lifetime of the host (1, Figure 1). Until recently, parasite persistence in healthy individuals was regarded as clinically asymptomatic. However, in the last decade, several reports have indicated that chronic cerebral toxoplasmosis may impact on the behaviour of its host (2).
- ^ Randall Parker: Humans Get Personality Altering Infections From Cats Arxivlandi 2005-12-17 yillarda Orqaga qaytish mashinasi. 2003 yil 30 sentyabr
- ^ a b Parlog A, Schlüter D, Dunay IR (March 2015). "Toxoplasma gondii-induced neuronal alterations". Parazit immunologiyasi. 37 (3): 159–170. doi:10.1111/pim.12157. hdl:10033/346575. PMID 25376390. S2CID 17132378.
The zoonotic pathogen Toxoplasma gondii infects over 30% of the human population. The intracellular parasite can persist lifelong in the CNS within neurons modifying their function and structure, thus leading to specific behavioural changes of the host. ... Furthermore, investigations of the human population have correlated Toksoplazma seropositivity with changes in neurological functions; however, the complex underlying mechanisms of the subtle behavioural alteration are still not fully understood. The parasites are able to induce direct modifications in the infected cells, for example by altering dopamine metabolism, by functionally silencing neurons as well as by hindering apoptosis.
- ^ a b v d Pappas G, Roussos N, Falagas ME (October 2009). "Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis". Xalqaro parazitologiya jurnali. 39 (12): 1385–94. doi:10.1016 / j.ijpara.2009.04.003. PMID 19433092.
- ^ Cook TB, Brenner LA, Cloninger CR, et al. (2015). ""Latent" infection with Toxoplasma gondii: association with trait aggression and impulsivity in healthy adults". Psixiatriya tadqiqotlari jurnali. 60: 87–94. doi:10.1016/j.jpsychires.2014.09.019. PMID 25306262.
- ^ Hurley RA, Taber KH (2012). "Latent Toxoplasmosis gondii: emerging evidence for influences on neuropsychiatric disorders". Nöropsikiyatriya va klinik nevrologiya jurnali. 24 (4): 376–83. doi:10.1176/appi.neuropsych.12100234. PMID 23224444.
Nine of eleven studies using the Cattell's 16-Personality Factor self-report questionnaire found significant and consistent results for both genders. Seropositive men overall had lower regard for rules and higher vigilance (suspicious, jealous, rigid/inflexible) than seronegative men. In contrast, seropositive women had greater regard for rules and higher warmth than seronegative women. Both seropositive genders were more anxious than matched healthy-comparison subjects. ... Behavioral observations and interviews were completed to ascertain whether the gender differences found in self-report measures were replicated by objective measures. Seropositive men scored significantly lower than seronegative men on Self-Control, Clothes Tidiness, and Relationships. The differences were less impressive for the seropositive women, with only trends toward higher scores on Self-Control and Clothes Tidiness as compared with seronegative women. The authors view the study results as objective confirmation that T. gondii presence can change a human host's behaviors.
- ^ Gohardehi, S; Sharif, M; Sarvi, S; Moosazadeh, M; Alizadeh-Navaei, R; Hosseini, SA; Amouei, A; Pagheh, A; Sadeghi, M; Daryani, A (August 2018). "The potential risk of toxoplasmosis for traffic accidents: A systematic review and meta-analysis". Eksperimental parazitologiya. 191: 19–24. doi:10.1016/j.exppara.2018.06.003. PMID 29906469.
- ^ Zimmermann, Stefan; Hadaschik, Eva; Dalpke, Alexander; Hassel, Jessica C.; Ajzenberg, Daniel; Tenner-Racz, Klara; Lehners, Nicola; Kapaun, Annette; Schnitzler, Paul (2013-04-01). "Varicella-Like Cutaneous Toxoplasmosis in a Patient with Aplastic Anemia". Klinik mikrobiologiya jurnali. 51 (4): 1341–1344. doi:10.1128/JCM.02851-12. ISSN 0095-1137. PMC 3666818. PMID 23390283.
- ^ Klaus, Sidney N.; Shoshana Frankenburg, and A. Damian Dhar (2003). "Chapter 235: Leishmaniasis and Other Protozoan Infections". In Freedberg; va boshq. (tahr.). Fitspatrikning umumiy tibbiyotdagi dermatologiyasi (6-nashr). McGraw-Hill. ISBN 0-07-138067-1.
- ^ a b v Robert-Gangneux, F.; Darde, M.-L. (2012). "Epidemiology of and Diagnostic Strategies for Toxoplasmosis". Klinik mikrobiologiya sharhlari. 25 (2): 264–296. doi:10.1128/CMR.05013-11. ISSN 0893-8512. PMC 3346298. PMID 22491772.
- ^ Markus, MB (1987). "Terms for coccidian merozoites". Tropik tibbiyot va parazitologiya yilnomalari. 81 (4): 463. doi:10.1080/00034983.1987.11812147. PMID 3446034.
- ^ a b v d e Miller CM; Boulter NR; Ikin RJ; Smith NC (January 2009). "The immunobiology of the innate response to Toxoplasma gondii". Xalqaro parazitologiya jurnali. 39 (1): 23–39. doi:10.1016/j.ijpara.2008.08.002. PMID 18775432.
- ^ a b v Martens S; Parvanova I; Zerrahn J; Griffiths G; Schell G; Reichmann G; Howard JC (November 2005). "Disruption of Toxoplasma gondii parasitophorous vacuoles by the mouse p47-resistance GTPases". PLOS patogenlari. 1 (3): e24. doi:10.1371/journal.ppat.0010024. PMC 1287907. PMID 16304607.
- ^ a b Denkers, EY; Schneider, AG; Cohen, AB; Butcher, BA (2012). "Phagocyte responses to protozoan infection and how Toxoplasma gondii meets the challenge". PLOS patogenlari. 8 (8): e1002794. doi:10.1371/journal.ppat.1002794. PMC 3410898. PMID 22876173.
- ^ a b v Hippe D, Weber A, Zhou L, Chang DC, Häcker G, Lüder CG (2009). "Toxoplasma gondii infection confers resistance against BimS-induced apoptosis by preventing the activation and mitochondrial targeting of pro-apoptotic Bax". Hujayra fanlari jurnali. 122 (Pt 19): 3511–21. doi:10.1242/jcs.050963. PMID 19737817.
- ^ a b v Wang Y, Weiss LM, Orlofsky A (2009). "Host cell autophagy is induced by Toxoplasma gondii and contributes to parasite growth". Biologik kimyo jurnali. 284 (3): 1694–701. doi:10.1074/jbc.M807890200. PMC 2615531. PMID 19028680.
- ^ a b Laliberté J, Carruthers VB (2008). "Host cell manipulation by the human pathogen Toxoplasma gondii". Uyali va molekulyar hayot haqidagi fanlar. 65 (12): 1900–15. doi:10.1007/s00018-008-7556-x. PMC 2662853. PMID 18327664.
- ^ a b v d e f g h men Weiss LM, Dubey JP (2009). "Toxoplasmosis: A history of clinical observations". Xalqaro parazitologiya jurnali. 39 (8): 895–901. doi:10.1016/j.ijpara.2009.02.004. PMC 2704023. PMID 19217908.
- ^ Toxoplasma gondii: the model apicomplexan: perspectives and methods. Elsevier / Academic Press. 2007 yil. ISBN 9780123695420.
- ^ a b v Derouin, F; Pelloux, H; ESCMID Study Group on Clinical, Parasitology. (2008 yil dekabr). "Prevention of toxoplasmosis in transplant patients". Klinik mikrobiologiya va infektsiya. 14 (12): 1089–101. doi:10.1111/j.1469-0691.2008.02091.x. PMID 19018809.
- ^ a b Khurana, Sumeeta; Batra, Nitya (2016). "Toxoplasmosis in organ transplant recipients: Evaluation, implication, and prevention". Tropik parazitologiya. 6 (2): 123–128. doi:10.4103/2229-5070.190814. PMC 5048698. PMID 27722100.
- ^ "Toksoplazmoz". Kasalliklarni nazorat qilish va oldini olish markazlari. 2004-11-22. Arxivlandi from the original on 2006-10-06.
- ^ a b v d e Jones JL, Dubey JP (September 2012). "Foodborne toxoplasmosis". Klinik yuqumli kasalliklar. 55 (6): 845–51. doi:10.1093/cid/cis508. PMID 22618566.
- ^ Dubey, J.P. "Swine Toxoplasmosis". Veterinary Division – Animal Health Programs. Arxivlandi asl nusxasidan 2017-03-22.
- ^ Signori Pereira, Karen; Franco, Regina; Leal, Diego (2010). "Transmission of Toxoplasmosis (Toxoplasma gondii) by Foods". Advances in Food Nutrition and Research. Oziq-ovqat va ovqatlanish bo'yicha tadqiqotlarning yutuqlari. 60: 1–19. doi:10.1016/S1043-4526(10)60001-0. ISBN 9780123809445. PMID 20691951.
- ^ "Parasites – Toxoplasmosis (Toxoplasma infection)". Kasalliklarni nazorat qilish va oldini olish markazlari. 2011-04-05. Arxivlandi from the original on 2015-08-28.
- ^ Assadi-Rad, A.M.; New, John C.; Patton, Sharon (April 1995). "Risk factors associated with transmission of Toxoplasma gondii to sows kept in different management systems in Tennessee". Veterinariya parazitologiyasi. 57 (4): 289–297. doi:10.1016/0304-4017(94)00677-5. PMID 7660566.
- ^ a b Coster, LO (June 2013). "Parasitic infections in solid organ transplant recipients". Shimoliy Amerikaning yuqumli kasalliklar klinikalari. 27 (2): 395–427. doi:10.1016/j.idc.2013.02.008. PMID 23714347.
- ^ a b Sterkers Y, Ribot J, Albaba S, Issert E, Bastien P, Pratlong F (2011). "Diagnosis of congenital toxoplasmosis by polymerase chain reaction on neonatal peripheral blood". Diagnostik mikrobiologiya va yuqumli kasallik. 71 (2): 174–6. doi:10.1016/j.diagmicrobio.2011.06.006. PMID 21856107.
- ^ a b v Di Mario, S; Basevi, V; Gagliotti, C; Spettoli, D; Gori, G; D'Amico, R; Magrini, N (23 October 2015). "Prenatal education for congenital toxoplasmosis" (PDF). Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 10 (10): CD006171. doi:10.1002/14651858.CD006171.pub4. PMID 26493047.
- ^ "Circular Normativa sobre Cuidados Pré-Concepcionais – Direcção-Geral de Saúde" (PDF). Arxivlandi asl nusxasi (PDF) 2011-07-16.
- ^ a b v d Sukthana Y (March 2006). "Toxoplasmosis: beyond animals to humans". Parazitologiya tendentsiyalari. 22 (3): 137–42. doi:10.1016/j.pt.2006.01.007. PMID 16446116.
- ^ [1] Arxivlandi 2011 yil 24 avgust, soat Orqaga qaytish mashinasi
- ^ a b De Paschale M, Agrappi C, Clerici P, Mirri P, Manco MT, Cavallari S, Viganò EF (2008). "Seroprevalence and incidence of Toxoplasma gondii infection in the Legnano area of Italy". Klinik mikrobiologiya va infektsiya. 14 (2): 186–9. doi:10.1111/j.1469-0691.2007.01883.x. PMID 18034857.
- ^ a b v d e Kapperud, Georg; Jenum, Pal A.; Stray-Pedersen, Babill; Melby, Kjetil K.; Eskild, Anne; Eng, Jan (1996). "Risk factors for Toxoplasma gondii infection in pregnancy. Results of a prospective case-control study in Norway". Amerika Epidemiologiya jurnali. 144 (4): 405–412. doi:10.1093/oxfordjournals.aje.a008942. PMID 8712198.
- ^ a b v d Hill D, Dubey JP (2002). "Toxoplasma gondii: transmission, diagnosis and prevention". Klinik mikrobiologiya va infektsiya. 8 (10): 634–40. doi:10.1046/j.1469-0691.2002.00485.x. PMID 12390281.
- ^ Cook AJ, Gilbert RE, Buffolano W, Zufferey J, Petersen E, Jenum PA, Foulon W, Semprini AE, Dunn DT (Jul 15, 2000). "Sources of toxoplasma infection in pregnant women: European multicentre case-control study. European Research Network on Congenital Toxoplasmosis". BMJ. 321 (7254): 142–7. doi:10.1136/bmj.321.7254.142. PMC 27431. PMID 10894691.
- ^ Bobić B, Jevremović I, Marinković J, Sibalić D, Djurković-Djaković O (September 1998). "Risk factors for Toksoplazma infection in a reproductive age female population in the area of Belgrade, Yugoslavia". Evropa epidemiologiya jurnali. 14 (6): 605–10. doi:10.1023/A:1007461225944. PMID 9794128. S2CID 9423818.
- ^ Jones JL, Dargelas V, Roberts J, Press C, Remington JS, Montoya JG (2009). "Risk Factors forToxoplasma gondiiInfection in the United States". Klinik yuqumli kasalliklar. 49 (6): 878–884. doi:10.1086/605433. PMID 19663709.
- ^ Kanková S, Sulc J, Nouzová K, Fajfrlík K, Frynta D, Flegr J (2007). "Women infected with parasite Toksoplazma have more sons". Naturwissenschaften vafot etdi. 94 (2): 122–7. Bibcode:2007NW.....94..122K. doi:10.1007/s00114-006-0166-2. PMID 17028886. S2CID 9610443.
- ^ Ian Sample, science correspondent (2006-10-12). "Pregnant women infected by cat parasite more likely to give birth to boys, say researchers | Science". The Guardian. London. Arxivlandi from the original on 2014-02-19. Olingan 2013-02-14.
- ^ Switaj K, Master A, Skrzypczak M, Zaborowski P (2005). "Recent trends in molecular diagnostics for Toxoplasma gondii infektsiyalar ". Klinik mikrobiologiya va infektsiya. 11 (3): 170–6. doi:10.1111/j.1469-0691.2004.01073.x. PMID 15715713.
- ^ a b v d Montoya JG (2002). "Laboratory diagnosis of Toxoplasma gondii infection and toxoplasmosis". Yuqumli kasalliklar jurnali. 185 (Suppl 1): S73–82. doi:10.1086/338827. PMID 11865443.
- ^ a b v Jones JL, Parise ME, Fiore AE (2014). "Neglected parasitic infections in the United States: toxoplasmosis". Amerika tropik tibbiyot va gigiena jurnali. 90 (5): 794–9. doi:10.4269/ajtmh.13-0722. PMC 4015566. PMID 24808246.
- ^ Remington, J. S.; Thulliez, P.; Montoya, J. G. (2004). "Recent Developments for Diagnosis of Toxoplasmosis". Klinik mikrobiologiya jurnali. 42 (3): 941–945. doi:10.1128/JCM.42.3.941-945.2004. ISSN 0095-1137. PMC 356902. PMID 15004036.
- ^ Sensini, A. (2006). "Toxoplasma gondii infection in pregnancy: opportunities and pitfalls of serological diagnosis". Klinik mikrobiologiya va infektsiya. 12 (6): 504–512. doi:10.1111/j.1469-0691.2006.01444.x. ISSN 1198-743X. PMID 16700697.
- ^ a b v d e f Lin MH, Chen TC, Kuo TT, Tseng CC, Tseng CP (2000). "Real-time PCR for quantitative detection of Toxoplasma gondii". Klinik mikrobiologiya jurnali. 38 (11): 4121–5. doi:10.1128/JCM.38.11.4121-4125.2000. PMC 87551. PMID 11060078.
- ^ Jons, J; Lopez, A; Wilson, M (15 May 2003). "Congenital toxoplasmosis". Amerika oilaviy shifokori. 67 (10): 2131–8. PMID 12776962.
- ^ "Congenital toxoplasmosis: MedlinePlus Medical Encyclopedia". medlineplus.gov. Olingan 2018-02-26.
- ^ Corrêa, Camila de Castro; Maximino, Luciana Paula; Weber, Silke Anna Theresa (July 2018). "Hearing Disorders in Congenital Toxoplasmosis: A Literature Review". International Archives of Otorhinolaryngology. 22 (3): 330–333. doi:10.1055/s-0037-1605377. ISSN 1809-9777. PMC 6033603. PMID 29983776.
- ^ Macedo de Resende, Luciana. "Congenital toxoplasmosis: Auditory and language outcomes in early diagnosed and treated children".
- ^ Doggett JS, Nilsen A, Forquer I, Wegmann KW, Jones-Brando L, Yolken RH, Bordón C, Charman SA, Katneni K, Schultz T, Burrows JN, Hinrichs DJ, Meunier B, Carruthers VB, Riscoe MK (2012). "Endochin-like quinolones are highly efficacious against acute and latent experimental toxoplasmosis". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 109 (39): 15936–41. Bibcode:2012PNAS..10915936D. doi:10.1073/pnas.1208069109. PMC 3465437. PMID 23019377.
- ^ Rolston KV, Hoy J (1987). "Role of clindamycin in the treatment of central nervous system toxoplasmosis". Amerika tibbiyot jurnali. 83 (3): 551–554. doi:10.1016/0002-9343(87)90769-8. PMID 3661590.
- ^ "CDC – Toxoplasmosis – Resources for Health Professionals". www.cdc.gov. Arxivlandi asl nusxasidan 2016 yil 26 noyabrda. Olingan 5 dekabr 2016.
- ^ "Toxoplasmosis – treatment key research". NAM & aidsmap. 2005-11-02. Arxivlandi asl nusxasi 2007-10-22 kunlari.
- ^ Djurković-Djaković O, Milenković V, Nikolić A, Bobić B, Grujić J (2002). "Efficacy of atovaquone combined with clindamycin against murine infection with a cystogenic (Me49) strain of Toxoplasma gondii" (PDF). Antimikrobiyal kimyoterapiya jurnali. 50 (6): 981–7. doi:10.1093/jac/dkf251. PMID 12461021. Arxivlandi (PDF) from the original on 2006-03-29.
- ^ Jones J, Lopez A, Wilson M (2003). "Congenital toxoplasmosis". Amerika oilaviy shifokori. 67 (10): 2131–8. PMID 12776962.
- ^ McLeod R, Kieffer F, Sautter M, Hosten T, Pelloux H (2009). "Why prevent, diagnose and treat congenital toxoplasmosis?". Memórias do Instituto Oswaldo Cruz. 104 (2): 320–44. doi:10.1590/s0074-02762009000200029. PMC 2735102. PMID 19430661.
- ^ McLeod R, Boyer K, Karrison T, Kasza K, Swisher C, Roizen N, Jalbrzikowski J, Remington J, Heydemann P, Noble AG, Mets M, Holfels E, Withers S, Latkany P, Meier P, et al. (Toxoplasmosis Study Group) (15 May 2006). "Outcome of Treatment for Congenital Toxoplasmosis, 1981–2004: The National Collaborative Chicago-Based, Congenital Toxoplasmosis Study". Klinik yuqumli kasalliklar. 42 (10): 1383–1394. doi:10.1086/501360. PMID 16619149.
- ^ "Congenital Toxoplasmosis". Baby's First Test. Olingan 2 aprel 2020.
- ^ a b Jones JL, Kruszon-Moran D, Sanders-Lewis K, Wilson M (September 2007). "Toxoplasma gondii infection in the United States, 1999 2004, decline from the prior decade". Amerika tropik tibbiyot va gigiena jurnali. 77 (3): 405–10. doi:10.4269/ajtmh.2007.77.405. PMID 17827351.
- ^ Scallan, Elaine; Hoekstra, Robert; Angulo, Frederick; Tauxe, Robert; Widdowson, Marc-Alain; Roy, Sharon; Jones, Jeffery; Griffin, Patricia (January 2011). "Foodborne Illness Acquired in the United States - Major Pathogens". Rivojlanayotgan yuqumli kasalliklar. 17 (1): 7–15. doi:10.3201/eid1701.P11101. PMC 3375761. PMID 21192848.
- ^ Dalimi A, Abdoli A (2011). "Latent Toxoplasmosis and Human". Eron parazitologiya jurnali. 7 (1): 1–17. PMC 3488815. PMID 23133466. Arxivlandi asl nusxasidan 2016-08-17.
- ^ Sibley LD; Khan A; Ajioka JW; Rosenthal BM (2009). "Genetic diversity of Toxoplasma gondii in animals and humans". Qirollik jamiyatining falsafiy operatsiyalari B: Biologiya fanlari. 364 (1530): 2749–2761. doi:10.1098/rstb.2009.0087. PMC 2865090. PMID 19687043.
- ^ "CDC: Parasites – Toxoplasmosis (Toxoplasma infection) – Pregnant Women". Arxivlandi asl nusxasidan 2013 yil 7 martda. Olingan 13 mart 2013.
- ^ Dubey JP, Frenkel JK (May 1998). "Toxoplasmosis of rats: a review, with considerations of their value as an animal model and their possible role in epidemiology". Veterinariya parazitologiyasi. 77 (1): 1–32. doi:10.1016/S0304-4017(97)00227-6. PMID 9652380.
- ^ Tucker, Abigail (2016). The Lion In the Living Room: How House Cats Tamed Us And Took Over the World. Simon va Shuster. p. 108. ISBN 978-1-4767-3823-9.
- ^ "Laboratory Tests For The Diagnosis Of Toxoplasmosis". Toxoplasma Serology Laboratory. Arxivlandi from the original on 2007-12-23.
- ^ "Sizning mushukingiz qanday qilib sizni aqldan ozdirmoqda - Ketlin Makoliff". Atlantika. 2012-02-06. Arxivlandi asl nusxasidan 2013-06-03. Olingan 2013-06-03.
- ^ "'Cat Lady' Conundrum – Rebecca Skloot". The New York Times. 2007-12-09. Arxivlandi asl nusxasidan 2017-01-18.
- ^ Torrey, E.; Simmons, Wendy; Yolken, Robert (June 2015). "Is childhood cat ownership a risk factor for schizophrenia later in life?". Shizofreniya tadqiqotlari. 165 (1): 1–2. doi:10.1016/j.schres.2015.03.036. PMID 25892720. S2CID 205073283.
- ^ Solmi, F .; Xeys, J. F .; Lyuis, G.; Kirkbride, J. B. (2017 yil 31-iyul). "Qiziqish mushukni o'ldirdi: Buyuk Britaniyaning umumiy populyatsiyasida 13 yoshdan 18 yoshgacha bo'lgan davrda mushukka egalik va psixotik alomatlar o'rtasidagi bog'liqlikning isboti yo'q". Psixologik tibbiyot. 47 (9): 1659–1667. doi:10.1017 / S0033291717000125. PMC 5939988. PMID 28222824.
- ^ Cook, A. J. C.; Holliman, Richard; Gilbert, R. E.; Buffolano, W.; Zufferey, J.; Petersen, E.; Jenum, P. A.; Foulon, W.; Semprini, A. E. (2000-07-15). "Sources of toxoplasma infection in pregnant women: European multicentre case-control study- Commentary: Congenital toxoplasmosis—further thought for food". BMJ. 321 (7254): 142–147. doi:10.1136/bmj.321.7254.142. ISSN 0959-8138. PMC 27431. PMID 10894691.
- ^ Kathleen McAuliffe (March 2012). "How Your Cat is Making You Crazy". Atlantika. Arxivlandi from the original on 2012-08-16.
- ^ Flegr Jaroslav (2007). "Ta'siri Toksoplazma on human behavior". Shizofreniya byulleteni. 33 (3): 757–760. doi:10.1093/schbul/sbl074. PMC 2526142. PMID 17218612. Arxivlandi from the original on 2015-02-19.
- ^ Arthur Ashe, Tennis Star, is Dead at 49 Arxivlandi 2008 yil 10-dekabr, soat Orqaga qaytish mashinasi Nyu-York Tayms (02/08/93)
- ^ Merritt Butrick, A Biography Arxivlandi 2011-07-13 da Orqaga qaytish mashinasi Angelfire.com, accessdate Mar 18, 2011
- ^ "Pedro Zamora Biography :: HIV Aids Activism Biography". Arxivlandi asl nusxasidan 2016-04-05.
- ^ "The Face That Defined AIDS". Arxivlandi asl nusxasidan 2016-04-02.
- ^ "Pregnancy superfoods revealed". BBC yangiliklari. January 10, 2001. Arxivlandi from the original on January 5, 2007. Olingan 25 may, 2010.
- ^ "Olympics bid Coes finest race". The Times. London. June 26, 2005. Archived from asl nusxasi 2011 yil 10 mayda. Olingan 25 may, 2010.
- ^ "SPORTS PEOPLE; Coe's Disorder Rare". The New York Times. 3 sentyabr 1983 yil. Olingan 3 may 2018.
- ^ Brody, Jane E. (27 October 1982). "PERSONAL HEALTH". Nyu-York Tayms. Arxivlandi asl nusxasidan 2017 yil 27 avgustda.
- ^ Rigoulet, Jacques; Hennache, Alain; Lagourette, Pierre; George, Catherine; Longeart, Loïc; Le Net, Jean-Loïc; Dubey, Jitender P. (2014). "Toxoplasmosis in a bar-shouldered dove (Geopelia humeralis) from the Zoo of Clères, France". Parazit. 21: 62. doi:10.1051/parasite/2014062. ISSN 1776-1042. PMC 4236686. PMID 25407506.

- ^ a b Ma, Hongyu; Wang, Zedong; Wang, Chengdong; Li, Caiwu; Vey, Feng; Liu, Quan (2015). "Fatal Toxoplasma gondii infection in the giant panda". Parazit. 22: 30. doi:10.1051/parasite/2015030. ISSN 1776-1042. PMC 4626621. PMID 26514595. Arxivlandi from the original on 2016-01-01.

- ^ a b Dubey (2016), p. kerak.
- ^ Rouatbi, Mariem; Amairiya, Safa; Amdouni, Yosra; Bussadun, Muhammad Anis; Ayadi, Ouarda; Al-Xosariy, Amira Adel Taxa; Rekik, Mourad; Ben Abdallah, Rim; Aoun, Karim; Dargut, Muhammad Aziz; Viland, Barbara; Garbi, Muhammad (2019). "Toxoplasma gondii Shimoliy Afrikada infektsiya va toksoplazmoz: sharh ". Parazit. 26: 6. doi:10.1051 / parazit / 2019006. ISSN 1776-1042. PMC 6376878. PMID 30767889.

- ^ Ekanayake, D. K .; Rajapakse, R. P V. J.; Dubey, J. P .; Dittus, W. P J. (2004). "Seroprevalans Toxoplasma gondii yirtqich toque makakalarida (Macaca sinica) Polonnaruwa, Shri-Lanka ". Parazitologiya jurnali. 90 (4): 870–871. doi:10.1645 / GE-291R. PMID 15357087. S2CID 23829241.
- ^ Xollings, Treysi; Jons, Menna; Muni, Nik; McCallum, Hamish (2013). "O'zgaruvchan landshaftlarda yovvoyi tabiat kasalliklari ekologiyasi: Mesopredator tarqalishi va toksoplazmoz". Xalqaro parazitologiya jurnali: parazitlar va yovvoyi tabiat. 2: 110–118. doi:10.1016 / j.ijppaw.2013.02.002. PMC 3862529. PMID 24533323.
- ^ Fankurt, Bronvin (2014 yil 5-oktabr). "Toksoplazmoz: qanday qilib yovvoyi mushuklar yovvoyi hayotni panjasini ko'tarmasdan o'ldiradi". Suhbat. Arxivlandi asl nusxasidan 2016 yil 23 dekabrda. Olingan 23 dekabr 2016.
- ^ a b v d Riaxi, Muhammad; Faxri, Yadulloh; Hanifehpur, Xuman; Valizoda, Sogra; Gulizoda, Majid; Xusseyni-Pouya, Roxane; Gamble, H.Ray (2017 yil sentyabr). "Toxoplasma gondii ning yovvoyi cho'chqalar orasida global seroprevalentligi: tizimli tahlil va meta-tahlil". Veterinariya parazitologiyasi. 244: 12–20. doi:10.1016 / j.vetpar.2017.07.013. PMID 28917302.
- ^ Chessa G, Chisu V, Porcu R, Masala G (2014). "Molekulyar xarakteristikasi Toxoplasma gondii Italiyaning Sardiniyadagi qo'ylar abortining II turi ".. Parazit. 21: 6. doi:10.1051 / parazit / 2014007. PMC 3927306. PMID 24534616.

- ^ a b v d Tenter AM, Heckeroth AR, Vayss LM (2000 yil noyabr). "Toxoplasma gondii: hayvonlardan odamlarga ". Xalqaro parazitologiya jurnali. 30 (12–13): 1217–58. doi:10.1016 / S0020-7519 (00) 00124-7. PMC 3109627. PMID 11113252.
- ^ Dubey (2016), 145-151 betlar.
- ^ Dubey JP, Sundar N, Hill D, Velmurugan GV, Bandini LA, Kwok OC, Majumdar D, Su C (iyul 2008). "Yuqori tarqalishi va ko'plab atipik genotiplari Toxoplasma gondii AQShda iste'mol qilish uchun mo'ljallangan qo'zichoqlardan ajratilgan ". Xalqaro parazitologiya jurnali. 38 (8–9): 999–1006. doi:10.1016 / j.ijpara.2007.11.012. PMID 18191859.
- ^ Dubey JP, Rajendran C, Ferreira LR, Martins J, Kvok OC, Hill DE, Villena I, Chjou X, Su S, Jons JL (iyul 2011). "Yuqori tarqalishi va genotiplari Toxoplasma gondii AQShda iste'mol qilish uchun mo'ljallangan echkilardan, chakana go'sht do'konidan ajratilgan ". Xalqaro parazitologiya jurnali. 41 (8): 827–33. doi:10.1016 / j.ijpara.2011.03.006. PMID 21515278.
- ^ Dubey JP (2010 yil fevral). "Toxoplasma gondii tovuqdagi yuqumli kasalliklar (Gallus domesticus): tarqalishi, klinik kasalligi, diagnostikasi va sog'liqni saqlashning ahamiyati ".. Zoonozlar va aholi salomatligi. 57 (1): 60–73. doi:10.1111 / j.1863-2378.2009.01274.x. PMID 19744305. S2CID 9228587.
- ^ Vayss va Kim (2011), p. 723.
- ^ Aroussi, Abdelkrim; Vignoles, Filipp; Dalmay, Fransua; Vimel, Lorens; Darde, Mari-Laur; Mercier, Aurélien; Ajzenberg, Daniel (2015). "Aniqlash Toxoplasma gondii Frantsiyadagi supermarketlarning ot go'shtidagi DNK va ikkita serologik tekshiruv natijalarini baholash ". Parazit. 22: 14. doi:10.1051 / parazit / 2015014. ISSN 1776-1042. PMC 4374124. PMID 25809058. Arxivlandi asl nusxasidan 2017-09-08.

- ^ Dubey, Jitender P. (2008-12-01). "Tarixi Toxoplasma gondii- dastlabki 100 yil ". Eukaryotik mikrobiologiya jurnali. 55 (6): 467–475. doi:10.1111 / j.1550-7408.2008.00345.x. ISSN 1550-7408. PMID 19120791.
- ^ Xatchison, VM (1965-05-29). "Toxoplasma gondii ning eksperimental o'tkazilishi". Tabiat. 206 (987): 961–2. Bibcode:1965 yil natur.206..961H. doi:10.1038 / 206961a0. PMID 5839865. S2CID 4207372.
- ^ a b v d Elmore SA, Jones JL, Conrad PA, Patton S, Lindsay DS, Dubey JP (2010 yil aprel). "Toxoplasma gondii: epidemiologiya, mushuklarning klinik jihatlari va oldini olish ".. Parazitologiya tendentsiyalari. 26 (4): 190–6. doi:10.1016 / j.pt.2010.01.009. PMID 20202907.
- ^ Jokelainen P, Simola O, Rantanen E, Näreaho A, Lohi H, Sukura A (noyabr 2012). "Finlyandiyada mushuk toksoplazmozi: kesma bo'yicha epidemiologik tadqiqotlar va seriyalarni o'rganish". Veterinariya diagnostikasi jurnali. 24 (6): 1115–24. doi:10.1177/1040638712461787. PMID 23012380.
- ^ Al-Kappani YM, Rajendran C, Ferreira LR, Kvok OC, Abu-Elvafa SA, Hilali M, Dubey JP (dekabr 2010). "Misrdan mushuklarda toksoplazmozning yuqori tarqalishi: hayotga yaroqliligini ajratish Toxoplasma gondii, to'qimalarning tarqalishi va izolyatsiyani belgilash ". Parazitologiya jurnali. 96 (6): 1115–8. doi:10.1645 / GE-2554.1. PMID 21158619. S2CID 25574092.
- ^ Dubey (2016), p. 95.
- ^ Dubey (2016), p. 46.
- ^ Andersen, Mark S.; Martin, Brent J.; Roemer, Gari V. (2004-12-15). "Erkin rouming mushuklarini boshqarish uchun evtanaziya va tuzoq-neytral qaytish samaradorligini baholash uchun matritsali populyatsiya modellaridan foydalanish". Amerika veterinariya tibbiyot assotsiatsiyasi jurnali. 225 (12): 1871–1876. doi:10.2460 / javma.2004.225.1871. ISSN 0003-1488. PMID 15643836. S2CID 17789584.
- ^ a b v d Vebster JP, Makkonki GA (iyun 2010). "Toxoplasma gondii- xostning o'zgargan xatti-harakatlari: harakat mexanizmiga oid ko'rsatmalar ". Folia Parasitologica. 57 (2): 95–104. doi:10.14411 / fp.2010.012. PMID 20608471.
- ^ Webster JP (2007 yil may). "Ta'siri Toxoplasma gondii hayvonlar harakati to'g'risida: mushuk va sichqonchani o'ynash " (PDF). Shizofreniya byulleteni. 33 (3): 752–6. doi:10.1093 / schbul / sbl073. PMC 2526137. PMID 17218613. Arxivlandi (PDF) asl nusxasidan 2015-09-04.
- ^ a b Berdoy, M.; Vebster, J. P .; Macdonald, D. W. (2000 yil 7-avgust). "Yuqtirilgan kalamushlarda o'limga olib keladigan tortishish Toxoplasma gondii". Qirollik jamiyati materiallari B: Biologiya fanlari. 267 (1452): 1591–4. doi:10.1098 / rspb.2000.1182. PMC 1690701. PMID 11007336.
- ^ Vyas A, Kim SK, Giacomini N, Boothroyd JC, Sapolsky RM (2007 yil 10-aprel). "Tomonidan qo'zg'atilgan xatti-harakatlar o'zgarishi Toksoplazma kemiruvchilarni yuqtirish mushuk hidlaridan nafratlanish uchun juda xosdir ". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 104 (15): 6442–7. Bibcode:2007PNAS..104.6442V. doi:10.1073 / pnas.0608310104. PMC 1851063. PMID 17404235.
- ^ Xiao J, Kannan G, Jones-Brando L, Brannock C, Krasnova IN, Kadet JL, Pletnikov M, Yolken RH (2012 yil 29-mart). "Surunkali ta'sir ko'rsatadigan gen ekspressioni va xatti-harakatlaridagi jinsga xos o'zgarishlar Toksoplazma sichqonlarga yuqtirish ". Nevrologiya. 206: 39–48. doi:10.1016 / j.neuroscience.2011.12.051. PMID 22240252. S2CID 24725619.
- ^ Lamberton PH, Donnelly CA, Webster JP (sentyabr 2008). "Ning o'ziga xos xususiyatiToxoplasma gondii- xatti-harakatni aniq va aniq bo'lmagan mezbonga etkazish xavfiga o'zgartirdi ". Parazitologiya. 135 (10): 1143–50. doi:10.1017 / S0031182008004666. PMID 18620624.
- ^ a b Xari Dass SA, Vyas A (dekabr 2014). "Toxoplasma gondii infektsiya xujayrali medial amigdaladagi epigenetik modulyatsiya orqali kalamushlarda yirtqichlardan nafratlanishni kamaytiradi ". Molekulyar ekologiya. 23 (24): 6114–6122. doi:10.1111 / mec.12888. PMID 25142402.
- ^ a b Flegr J, Markosh A (2014 yil dekabr). "Epigenetik muhandislik durdonasi - qanday qilib Toxoplasma gondii reprogrammes qo'rquvni jinsiy tortishish holatiga o'tkazish uchun miyani joylashtiradi ". Molekulyar ekologiya. 23 (24): 5934–5936. doi:10.1111 / mec.13006. PMID 25532868. S2CID 17253786.
- ^ McCowan TJ, Dhasathati A, Carvelli L (Fevral 2015). "Amfetaminning epigenetik mexanizmlari". J. Addict. Oldingi. 2015 (S1): 1-7. ISSN 2330-2178. PMC 4955852. PMID 27453897.
Qo'shadi giyohvand moddalar tomonidan kelib chiqqan epigenetik modifikatsiyalar neyronlarning plastisiyasida va giyohvandlik bilan bog'liq xulq-atvorda muhim rol o'ynaydi. AMPHning genlarni boshqarishga ta'sirini o'rgangan bir nechta tadqiqotlar bo'lsa-da (1-jadval), hozirgi ma'lumotlar AMPH giston / DNKning o'zaro ta'sirini o'zgartirish va natijada ba'zi genlarning repressiyasini va boshqa genlarning faollashishini keltirib chiqaradigan transkripsiya omillarini jalb qilish uchun bir nechta darajada harakat qiladi. Muhimi, ba'zi tadqiqotlar AMPH tomonidan kelib chiqadigan epigenetik regulyatsiyani ushbu preparat tomonidan kelib chiqadigan xulq-atvor natijalari bilan o'zaro bog'liq bo'lib, shuning uchun epigenetikani qayta qurish AMPH tomonidan kelib chiqadigan xatti-harakatlar o'zgarishi asosida yotadi. Agar bu haqiqat bo'lsa, giston asetilatsiyasini, metilatsiyasini yoki DNK metilatsiyasini inhibe qiluvchi o'ziga xos dori vositalaridan foydalanish AMFga qaramlikni oldini olish va / yoki bekor qilish va DEHBni davolashda AMPH tomonidan hosil bo'ladigan yon ta'sirlarni yumshatish uchun muhim terapevtik alternativ bo'lishi mumkin.
- ^ Walker DM, Cates HM, Heller EA, Nestler EJ (2015 yil fevral). "Xromatin holatlarini suiiste'mol qilish bilan tartibga solish". Curr. Opin. Neyrobiol. 30: 112–121. doi:10.1016 / j.conb.2014.11.002. PMC 4293340. PMID 25486626.
- ^ Nestler EJ (2014 yil yanvar). "Giyohvandlikning epigenetik mexanizmlari". Neyrofarmakologiya. 76 (Pt B): 259-268. doi:10.1016 / j.neuropharm.2013.04.004. PMC 3766384. PMID 23643695.
Giston asetilatsiyasining qisqa muddatli o'sishi, odatda, giyohvand moddalarga nisbatan ta'sirini kuchaytiradi, barqaror o'sish esa HDAC inhibitörlerinin tizimli yoki NAc ichidagi ma'muriyatining harakatlariga asoslangan holda kokain ta'siriga qarshi turadi. ... NAc tarkibidagi G9a ning genetik yoki farmakologik blokadasi kokain va afyunlarga xatti-harakatlarni kuchaytiradi, G9a funktsiyasini oshirish esa teskari ta'sir ko'rsatadi (Maze va boshq., 2010; Sun va boshq., 2012a). G9a va H3K9me2 ning giyohvand moddalar bilan bog'liq bunday regulyatsiyasi, shuningdek, hayvonlarni keyingi surunkali stressning zararli ta'siriga sezgir qiladi (Covington va boshq., 2011). G9a ning regulyatsiyasi NAc neyronlarining dendritik arborizatsiyasini oshiradi va sinaptik funktsiyaga taalluqli ko'plab oqsillarning ko'payishi bilan bog'liq bo'lib, bu o'zgaruvchan G9a / H3K9me2 ni giyohvandlik bilan bog'liq sinaptik plastisitda bevosita bog'laydi (Maze va boshq., 2010).
G9a NAc-da epigenetik regulyatsiya uchun juda muhim nazorat nuqtasi bo'lib ko'rinadi, chunki biz uning ikkita salbiy teskari ko'chadan ishlashini bilamiz. U giyohvandlik uchun muhim bo'lgan uzoq davom etadigan transkripsiya omili bo'lgan DFOSB induktsiyasiga qarshi turadi (Robison va Nestler, 2011), DFOSB esa G9a ekspresiyasini bostiradi (Maze va boshq., 2010; Sun va boshq., 2012a). ... Bundan tashqari, G9a uzoq vaqt davomida HDAC inhibisyonunda NAc da indüklenir, bu yuqorida ta'kidlanganidek, ushbu sharoitda kokainning xulq-atvor ta'sirining paradoksal susayishini tushuntiradi (Kennedi va boshq., 2013). GABAA retseptorlari subbirligi genlari ushbu qayta aloqa davri tomonidan boshqariladiganlar qatoriga kiradi. Shunday qilib, surunkali kokain yoki uzoq davom etadigan HDAC inhibatsiyasi NAcdagi bir nechta GABAA retseptorlari subbirliklarini keltirib chiqaradi, bu esa inhibitiv postsinaptik oqimlar (IPSC) chastotasining ko'payishi bilan bog'liq. Ajoyib kontrastda G9a induktsiyasini keltirib chiqaradigan va H3K9me2 ning global darajasining oshishiga olib keladigan kokain va HDAC inhibisyonuna ta'sir qilish GABAA retseptorlari blokadasiga va IPSC regulyatsiyasiga olib keladi. - ^ Vanagas L, Jeffers V, Bogado SS, Dalmasso MC, Sallivan WJ, Angel SO (oktyabr 2012). "Toksoplazma giston atsetilatsiyasini qayta tiklovchi vositalar yangi dori-darmon sifatida". Infektsiyaga qarshi terapiyani ekspertizasi. 10 (10): 1189–1201. doi:10.1586 / eri.12.100. PMC 3581047. PMID 23199404.
- ^ Bouchut A, Chavla AR, Jeffers V, Xudmon A, Sallivan VJ (2015). "Kortikal astrositlarda oqsilli lizin atsetilatsiyasi va miya parazitiga yuqish paytida yuz beradigan o'zgarishlar Toxoplasma gondii". PLOS ONE. 10 (3): e0117966. Bibcode:2015PLoSO..1017966B. doi:10.1371 / journal.pone.0117966. PMC 4364782. PMID 25786129.
- ^ McConkey GA, Martin HL, Bristow GC, Webster JP (2013 yil 1-yanvar). "Toxoplasma gondii infektsiya va o'zini tutish - joylashuvi, joylashuvi, joylashuvi? ". Eksperimental biologiya jurnali. 216 (Pt 1): 113-9. doi:10.1242 / jeb.074153. PMC 3515035. PMID 23225873.
- ^ a b Afonso C, Payxão VB, Kosta RM (2012). Hakimi (tahrir). "Surunkali Toksoplazma infektsiya xostning tuzilishini va xavfini o'zgartiradi ". PLOS ONE. 7 (3): e32489. Bibcode:2012PLoSO ... 732489A. doi:10.1371 / journal.pone.0032489. PMC 3303785. PMID 22431975.
- ^ Gonsales LE, Rojnik B, Urrea F, Urdaneta H, Petrosino P, Colasante C, Pino S, Hernandez L (2007 yil 12-fevral). "Toxoplasma gondii kalamushlarda plyus-labirint va ijtimoiy ta'sir o'tkazish testlarida o'lchangan infektsiyaning past xavotiri: xulq-atvori tahlili ". Xulq-atvorni o'rganish. 177 (1): 70–9. doi:10.1016 / j.bbr.2006.11.012. PMID 17169442. S2CID 33572709.
- ^ Conrad PA, Miller MA, Kreuder C, Jeyms ER, Mazet J, Dabritz H, Jessup DA, Gulland F, Grigg ME (2005). "Uzatish Toksoplazma: dengiz quyruqlarini qo'riqchilar sifatida o'rganishdan olingan maslahatlar Toxoplasma gondii dengiz muhitiga tushish ". Xalqaro parazitologiya jurnali. 35 (11–12): 1155–68. doi:10.1016 / j.ijpara.2005.07.002. PMID 16157341.
- ^ "Rivojlanayotgan dunyoda kasalliklarni davolash". Nation Science juma kuni haqida suhbat. Milliy jamoat radiosi. 2005 yil 16-dekabr. Arxivlandi asl nusxasidan 2006 yil 27 aprelda.
- ^ "Dengiz samurini o'ldiradigan mushuklarda parazit". NOAA jurnali. Milliy Okean va atmosfera boshqarmasi. 21 yanvar 2003. Arxivlangan asl nusxasi 2007 yil 25 dekabrda. Olingan 24-noyabr 2007.
- ^ Diep, Frensi (3 sentyabr, 2019). "Kaliforniyadagi dengiz samolyotlarini o'ldirish nima? Uy mushuklari". Nyu-York Tayms. Olingan 9 sentyabr 2019.
- ^ a b Douson, Tereza. "Mushuk kasalligi yo'qolib ketish xavfi ostida bo'lgan rohiblarning muhrlarini tahdid qilmoqda". Ilmiy Amerika. Olingan 11 oktyabr 2017.
- ^ Honnold, SP; Braun, R; Skott, DP; Sreekumar, C; Dubey, JP (iyun 2005). "Gavayi rohibining muhridagi toksoplazmoz (Monachus schauinslandi)". Parazitologiya jurnali. 91 (3): 695–7. doi:10.1645 / GE-469R. PMID 16108571. S2CID 13562317.
- ^ "3 shizofreniya". Arxivlandi asl nusxasidan 2010-01-02.
- ^ "Mushuklar tomonidan tarqalgan parazit Kvebekning yo'qolib ketish xavfi ostidagi belugalariga (kitlariga) tahdid solmoqda" CBC yangiliklari. 15-oktabr, 2018. Muallif Sidxarta Banerji.
- ^ Massi, Gloeta N.; Bare, Maykl V.; Villegas, Erik N .; Qora, Maykl V. (2010). "Olib olish va uzatish Toxoplasma gondii migratsion, filtr bilan oziqlanadigan baliqlar tomonidan ookistalar ". Veterinariya parazitologiyasi. 169 (3–4): 296–303. doi:10.1016 / j.vetpar.2010.01.002. ISSN 0304-4017. PMID 20097009.
- ^ a b v Fuglevich, AJ; Piotrowski, P; Stodolak, A (sentyabr 2017). "Toksoplazmoz va shizofreniya o'rtasidagi munosabatlar: sharh". Klinik va eksperimental tibbiyotdagi yutuqlar. 26 (6): 1031–1036. doi:10.17219 / acem / 61435. PMID 29068607.
- ^ a b v d Vebster JP, Kaushik M, Bristow GC, Makkonki GA (2013 yil 1-yanvar). "Toxoplasma gondii yuqumli kasallik, yirtqichlikdan shizofreniyaga qadar: hayvonlarning xatti-harakatlari inson xatti-harakatlarini tushunishda bizga yordam bera oladimi? ". Eksperimental biologiya jurnali. 216 (Pt 1): 99-112. doi:10.1242 / jeb.074716. PMC 3515034. PMID 23225872.
- ^ a b Flegr J (2013 yil 1-yanvar). "Yashirin ta'sir Toksoplazma inson shaxsiga, fiziologiyasiga va morfologiyasiga yuqish: ijobiy va salbiy tomonlari Toksoplazma- manipulyatsiya gipotezasini o'rganishda inson modeli ". Eksperimental biologiya jurnali. 216 (Pt 1): 127-33. doi:10.1242 / jeb.073635. PMID 23225875.
- ^ a b Torrey EF, Bartko JJ, Yolken RH (2012). "Toksoplazmoz gondii va shizofreniya uchun boshqa xavf omillari: yangilanish ". Shizofreniya byulleteni. 38 (3): 642–647. doi:10.1093 / schbul / sbs043. PMC 3329973. PMID 22446566. Arxivlandi asl nusxasidan 2015-09-04.
- ^ a b Arias, men; Sorlozano, A; Villegas, E; de Dios Luna, J; McKenney, K; Servilya, J; Gutyerrez, B; Gutierrez, J (aprel 2012). "Shizofreniya bilan bog'liq bo'lgan yuqumli kasalliklar: meta-tahlil". Shizofreniya tadqiqotlari. 136 (1–3): 128–36. doi:10.1016 / j.schres.2011.10.026. PMID 22104141. S2CID 2687441. Arxivlandi (PDF) asl nusxasidan 2015-09-04.
- ^ a b Flegr J (2013). "Qanday qilib va nima uchun toksoplazma bizni aqldan ozdiradi". Parazitologiya tendentsiyalari. 29 (4): 156–163. doi:10.1016 / j.pt.2013.01.007. PMID 23433494.
- ^ Torrey EF, Yolken RH (2007 yil may). "Shizofreniya va toksoplazmoz". Shizofreniya byulleteni. 33 (3): 727–8. doi:10.1093 / schbul / sbm026. PMC 2526129. PMID 17426051.
- ^ de Barros, JLVM; Barbosa, IG; Salem, H; Rocha, NP; Kummer, A; Okusaga, OO; Soares, JK; Teixeira, AL (fevral 2017). "Toxoplasma gondii infektsiyasi va bipolyar buzilish o'rtasida biron bir bog'liqlik bormi? Tizimli tahlil va meta-tahlil". Affektiv buzilishlar jurnali. 209: 59–65. doi:10.1016 / j.jad.2016.11.016. PMID 27889597.
- ^ Pearce BD, Kruszon-Moran D, Jons JL (2012 yil 15-avgust). "O'rtasidagi munosabatlar Toxoplasma gondii sog'liqni saqlash va ovqatlanish bo'yicha uchinchi milliy so'rovda infektsiya va kayfiyatning buzilishi ". Biologik psixiatriya. 72 (4): 290–5. doi:10.1016 / j.biopsych.2012.01.003. PMC 4750371. PMID 22325983.
- ^ Sugden, Karen; Moffitt, Terri E.; Pinto, Laurian; Pulton, Richi; Uilyams, Benjamin S.; Kaspi, Avshalom; Tanovits, Herbert B. (2016 yil 17-fevral). "Yo'q Toksoplazma Gondii Odamlarda miya va xatti-harakatlarning buzilishi bilan bog'liq infektsiya? Aholining vakili tug'ilish kohortidan dalillar ". PLOS ONE. 11 (2): e0148435. Bibcode:2016PLoSO..1148435S. doi:10.1371 / journal.pone.0148435. PMC 4757034. PMID 26886853.
- ^ Stascheit F, Pol F, Harms L, Rosche B (2015). "Toxoplasma gondii seropozitivlik skleroz bilan salbiy bog'liqdir ". Neyroimmunologiya jurnali. 285: 119–124. doi:10.1016 / j.jneuroim.2015.05.011. PMID 26198927. S2CID 33082008.
- ^ a b v d e Yan, Chao; Liang, Li-Jun; Chjen, Kuy-Yang; Chju, Xing-Quan (2016). "Toxoplasma gondii paydo bo'lishi, tarqalishi va tarqalishiga atrof-muhit omillarining ta'siri". Parazitlar va vektorlar. 9 (137): 137. doi:10.1186 / s13071-016-1432-6. PMC 4785633. PMID 26965989.
- ^ Dolgin, Elie (2017 yil 30 mart). "Iqlim o'zgarishi: muzlar erishi bilan". Tabiat. 543 (7647): S54-S55. Bibcode:2017Natur.543S..54D. doi:10.1038 / 543S54a. PMID 28355191. S2CID 4448339.
- Ushbu maqolaning ayrim qismlari umumiy foydalanish joyidan olingan CDC ma'lumotlari: Toksoplazmoz
Bibliografiya
- Vayss, L. M .; Kim, K. (28 aprel 2011). Toxoplasma gondii: Apicomplexan modeli. Perspektivlari va usullari. Akademik matbuot. ISBN 978-0-08-047501-1. Olingan 12 mart 2013.
- Dubey, J. P. (2016). Hayvonlar va odamlarning toksoplazmozisi (2-nashr). CRC Press. ISBN 978-1-4200-9237-0.
- Dubey JP, Lindsay DS, Speer CA (aprel 1998). "Tuzilmalari Toxoplasma gondii taxyzoitlar, bradizoidlar va sporozoitlar va biologiya va to'qima kistalarining rivojlanishi ". Klinik mikrobiologiya sharhlari. 11 (2): 267–299. doi:10.1128 / CMR.11.2.267. PMC 106833. PMID 9564564.
- Jaroslav Flegr (2011). Pozor, Toxo!. Academia, Praga, Chexiya. ISBN 978-80-200-2022-2.
Tashqi havolalar
- Mushuklar bilan yuqadigan parazit odamlarga qanday yuqadi (National Geographic)
- Toksoplazmoz da Merck diagnostika va terapiya qo'llanmasi Professional nashr
- Toksoplazmoz Sog'liqni saqlash agentligi (HPA) da, Buyuk Britaniya
- Toksoplazmozning rasmlari Tibbiy rasmlar ma'lumotlar bazasi
- Video-intervyu professor bilan Robert Sapolskiy Toksoplazmoz va uning inson xatti-harakatlariga ta'siri to'g'risida (24:27 min)
- "Toksoplazmoz". MedlinePlus. AQSh milliy tibbiyot kutubxonasi.
| Tasnifi | |
|---|---|
| Tashqi manbalar |
