Tamaki sog'lig'iga ta'siri - Health effects of tobacco
Tamaki iste'mol qilish, asosan, inson salomatligi va tashvishlariga salbiy ta'sir ko'rsatadi tamaki sog'lig'iga ta'siri uzoq tarixga ega. Tadqiqotlar asosan sigaretaga qaratilgan tamaki chekish.[1][2]
Tamaki tutuni tarkibida ko'proq 70 ta kimyoviy moddalar bu saraton kasalligini keltirib chiqaradi.[3] Tamaki tarkibida ham mavjud nikotin, bu juda yuqori qo'shadi psixoaktiv dori. Tamaki chekilganda, nikotin jismoniy va psixologik qaramlik. Sigaretalar sotilgan kam rivojlangan mamlakatlar smola tarkibida yuqori miqdordagi moy bor va filtrlash ehtimoli kam, bu esa ushbu hududlarda tamaki chekish bilan bog'liq kasalliklarga nisbatan zaiflikni kuchaytiradi.[4]
Tamaki iste'mol qilish eng katta narsa oldini olish mumkin bo'lgan o'lim sababi global miqyosda.[5] Tamaki iste'mol qiladigan odamlarning deyarli yarmi tamaki iste'mol qilishning asoratlari tufayli vafot etadi.[3] The Jahon Sog'liqni saqlash tashkiloti (JSST) hisob-kitoblariga ko'ra, har yili tamaki 6 millionga yaqin o'limga olib keladi (o'limning 10 foizga yaqini), ulardan 600 ming nafari chekmaydiganlarda bo'ladi. ikkinchi qo'l tutun.[3][6] 20-asrda tamaki 100 million odamning o'limiga sabab bo'lgan deb taxmin qilinadi.[3] Xuddi shunday, Qo'shma Shtatlar Kasalliklarni nazorat qilish va oldini olish markazlari tamaki iste'molini "rivojlangan mamlakatlarda inson salomatligi uchun eng muhim oldini olish mumkin bo'lgan xavf va butun dunyoda erta o'limning muhim sababi" deb ta'riflaydi.[7] Ayni paytda AQShda yiliga tamaki iste'mol qilishdan vafot etganlar soni tamaki sanoatida ishlayotganlar sonidan 4 taga ko'p bo'lib, 1 taga ko'p.[8] 2014 yilda ko'rib chiqilgan ma'lumotlarga ko'ra Nyu-England tibbiyot jurnali, tamaki tamaki, agar hozirgi chekish tartiblari saqlanib qolsa, XXI asrda taxminan 1 milliard odamni o'ldiradi, ularning yarmi 70 yoshgacha.[9]
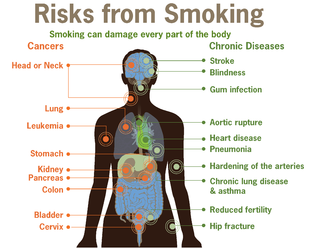
Tamaki iste'mol qilish odatda yurak, jigar va o'pka ta'sir qiladigan kasalliklarga olib keladi. Chekish asosiy yo'nalishdir xavf omili uchun yurak xurujlari, zarbalar, surunkali obstruktiv o'pka kasalligi (KOAH) (shu jumladan amfizem va surunkali bronxit ) va bir nechta saraton (xususan o'pka saratoni, gırtlak va og'iz saratoni, qovuq saratoni va oshqozon osti bezi saratoni ). Bu ham sabab bo'ladi periferik arterial kasallik va yuqori qon bosimi. Ta'siri odam qancha yil chekkaniga va qancha sigaret chekishiga bog'liq. Hayotdan oldin chekishni boshlash va undan yuqori sigaret chekish smola ushbu kasalliklar xavfini oshiradi. Shuningdek, atrof-muhit tamaki tutuni, yoki chekish, har qanday yoshdagi odamlarning sog'lig'iga salbiy ta'sir ko'rsatishi isbotlangan.[10] Tamakidan foydalanish muhim omil hisoblanadi tushish orasida homilador chekuvchilar va bu sog'liqning boshqa qator muammolariga hissa qo'shadi homila kabi erta tug'ilish, kam vazn, va imkoniyatning 1,4 dan 3 baravarigacha ko'payadi to'satdan chaqaloq o'lim sindromi (SIDS).[11] Hodisa erektil disfunktsiya chekuvchi erkaklarga nisbatan chekuvchilarga nisbatan 85 foizga yuqori.[12][13]
Bir qator mamlakatlar tamaki iste'molini nazorat qilish bo'yicha choralar ko'rishdi va ulardan foydalanish cheklangan ogohlantirish xabarlari qadoqlashda bosilgan. Qo'shimcha ravishda, tutunsiz qonunlar jamoat joylarida, masalan, ish joylarida, teatrlarda, barlarda va restoranlarda chekishni taqiqlash chekuvchilarning chekishlarini kamaytiradi va chekuvchilarni tark etishga yordam beradi, restoranlarga yoki barlarga salbiy iqtisodiy ta'sir ko'rsatmaydi.[3] Tamaki soliqlari narxni oshiradigan narsa, ayniqsa rivojlanayotgan mamlakatlarda ham samarali.[3]
Tamaki iste'mol qilish ba'zi kasalliklarni, shu jumladan og'izda saraton kasalligini keltirib chiqaradi degan fikr dastlab 1700 yillarning oxiri va 1800 yillarda tibbiyot hamjamiyati tomonidan keng qabul qilingan.[14] 1880-yillarda avtomatizatsiya sigaretalar narxini pasaytirdi va ulardan foydalanish kengaydi.[15][16] 1890-yillardan boshlab tamakidan foydalanish saraton va qon tomir kasalligi muntazam ravishda xabar berib turilgan; a meta-tahlil 167 ta boshqa asarga asoslanib, 1930 yilda nashr etilgan va tamaki iste'mol qilish saraton kasalligini keltirib chiqaradi degan xulosaga keldi.[17][18] 1930-yillarda va 1938 yilda tobora mustahkam kuzatuv dalillari nashr etildi. Ilm-fan tamaki iste'molchilarining hayoti ancha qisqaroqligini ko'rsatadigan qog'oz nashr etdi. Keys-tekshiruv ishlari nashr etilgan Natsistlar Germaniyasi 1939 va 1943 yillarda, 1948 yilda Niderlandiyada, lekin birinchi navbatda 1950 yilda AQSh va Buyuk Britaniya tadqiqotchilari tomonidan nashr etilgan beshta ish nazorati bo'yicha tadqiqotlar keng e'tiborni tortdi. Ushbu tadqiqotlar namoyish sifatida keng tanqid qilindi nedensellik emas, korrelyatsiya. 1950-yillarning boshlarida o'tkaziladigan istiqbolli kogort tadqiqotlarini kuzatib boring, aniqroq aniqlanishicha, chekuvchilar tezroq vafot etgan va o'lish ehtimoli ko'proq bo'lgan. o'pka saratoni va yurak-qon tomir kasalliklari.[14] Ushbu natijalar birinchi bo'lib 60-yillarning o'rtalarida tibbiyot jamoatchiligida keng qabul qilindi va keng jamoatchilik orasida e'lon qilindi.[14]
| Qismi bir qator kuni |
| Tamaki |
|---|
 |
| Tarix |
| Kimyo |
| Biologiya |
| Shaxsiy va ijtimoiy ta'sir |
| Ishlab chiqarish |
Tarix
Oldindan chekish
Tamakining sog'likka ta'siri haqida tashvish uzoq tarixga ega. Chekish oqibatida yo'tal, tomoq tirnash xususiyati va nafas qisilishi doimo aniq bo'lib kelgan.[iqtibos kerak ]
Dastlabki zamonaviy davrlarda G'arbiy Afrika Musulmon ulamolar tamaki chekishning sog'liqqa salbiy ta'sirini bilishar edi. Tamaki chekishning zarari hujjatlarda qayd etilgan Timbuktu qo'lyozmalari.[19]
Quvurlar bilan chekish asta-sekin 1700-yillarda bajarilgan ishlardan so'ng og'iz saraton kasalligining sababi sifatida qabul qilindi. Turli xil saraton kasalliklari va tamakidan foydalanish o'rtasidagi bog'liqlik 1800 yillarning oxiridan 1920 yillarning boshlariga qadar bir necha bor kuzatilgan. Tamaki iste'mol qilish va qon tomir kasallik haqida 1800 yillarning oxiridan boshlab xabar berilgan.[iqtibos kerak ]
Gideon Lincekum, amerikalik tabiatshunos va botanika tibbiyotining amaliyotchisi, 19-asrning boshlarida tamaki to'g'risida yozgan edi: "Ushbu zaharli o'simlik eski maktab fakulteti tomonidan dori sifatida juda ko'p ishlatilgan va minglab odamlar uni o'ldirgan ... bu juda xavfli maqola va uni xohlagancha ishlating, u har doim hayotiy energiyani ishlatilgan miqdorga mutanosib ravishda kamaytiradi - bu asta-sekin bo'lishi mumkin, ammo bu juda aniq ".[20]
Amerikaning janubida 1880-yillarda avtomatlashtirilgan sigareta ishlab chiqarish texnikasini ixtiro qilish arzon narxlarda sigaretalarni ommaviy ishlab chiqarish imkoniyatini yaratdi va chekish odatiy holga aylandi. Bu tamaki iste'molini zararli deb e'tiroz bildirgan va tamaki sotish va foydalanishga ba'zi taqiqlarni keltirib chiqargan qarama-qarshilikka va tamakini taqiqlash harakatiga olib keldi.[15] 1912 yilda amerikalik doktor Isaak Adler birinchi bo'lib o'pka saratoni chekish bilan bog'liqligini ta'kidladi.[21] 1924 yilda iqtisodchi Irving Fisher yozgan chekishga qarshi uchun maqola Reader Digest "... tamaki tananing butun ohangini pasaytiradi va uning hayotiy kuchi va qarshiligini pasaytiradi ... tamaki giyohvandlik zahari kabi, afyun kabi va alkogolga o'xshaydi, garchi odatda kamroq bo'lsa ham".[22] Reader Digest ko'p yillar davomida tez-tez chekishga qarshi maqolalar chop etmoqda.[iqtibos kerak ]
Gacha Birinchi jahon urushi, o'pka saratoni kamdan-kam uchraydigan kasallik deb hisoblangan, aksariyat shifokorlar kariyerasi davomida uni hech qachon ko'ra olmaydilar.[23][24] Urushdan keyin sigareta chekishni ommalashishi bilan birga, o'pka saratoni epidemiyasi paydo bo'ldi.[25]
Dastlabki kuzatuv ishlari
1890-yillardan boshlab tamaki iste'mol qilishning saraton va qon tomir kasalliklari bilan bog'liqligi to'g'risida muntazam ravishda xabar berib turilgan.[14] 1930 yilda, Fritz Likkint ning Drezden, Germaniya, nashr etilgan[18][17] a metanaliz tamaki iste'molini o'pka saratoni bilan bog'lashga qaratilgan 167 ta boshqa ishlarga asoslanib[17] Lickint buni ko'rsatdi o'pka saratoni chekuvchilar bo'lishi mumkin edi. Shuningdek, u o'pka saratoni ayollarga nisbatan to'rt yoki besh marta tez-tez uchraganini tushuntirish uchun eng yaxshi usul tamaki iste'mol qilishdir (ayollar chekkanligi sababli).[18] va chekishning jigar va siydik pufagi saratoniga sababchi ta'sirini muhokama qildi.[17]
Rolleston, J. D. (1932-07-01). "Chekish odati". Britaniya kambag'allik jurnali (alkogolizm va giyohvandlik). 30 (1): 1–27. doi:10.1111 / j.1360-0443.1932.tb04849.x. ISSN 1360-0443.
Ko'proq kuzatuv dalillari 1930-yillarda nashr etilgan va 1938 yilda, Ilm-fan tamaki iste'molchilarining hayoti ancha qisqaroqligini ko'rsatadigan qog'oz nashr etdi. U qurdi omon qolish egri chizig'i da saqlanadigan oilaviy tarix yozuvlaridan Jons Xopkins gigiena va jamoat salomatligi maktabi. Ushbu natija e'tiborga olinmadi yoki noto'g'ri tushuntirildi.[14]
Tamaki va yurak xurujlari o'rtasidagi bog'liqlik birinchi marta 1930 yilda qayd etilgan; katta amaliy-nazorat ishi 1940 yilda muhim birlashma topdi, ammo bunday xulosa tortishuvlarga sabab bo'lishi mumkinligi va shifokorlar bunga hali tayyor emasligi sababli sabab haqida biron bir narsa aytishdan qochishdi.[14]
Rasmiy dushmanlik 1939 va 1943 yillarda natsistlar nazorati bo'yicha tadqiqotlar nashr etilgan fashistlar Germaniyasida tamaki iste'mol qilish keng tarqalgan edi. Yana bir nafari 1948 yilda Gollandiyada nashr etilgan. 1939 yilda o'pka saratoni va chekishni davolash bo'yicha tadqiqot. Frants Hermann Myuller, uning metodikasida jiddiy zaif tomonlari bor edi, ammo tadqiqotni loyihalash muammolari keyingi tadqiqotlarda yaxshiroq hal qilindi.[14] Natsistlar rahbariyati bilan tamakiga qarshi tadqiqotlar va jamoat salomatligini muhofaza qilish choralari birlashishi ushbu tadqiqotlarga etarlicha e'tibor berilmasligiga sabab bo'lishi mumkin.[18] Ular nemis va golland tillarida ham nashr etilgan. Ushbu tadqiqotlar umuman e'tibordan chetda qoldi.[26] 1947 yilda Britaniya Tibbiy Kengashi o'pka saratoni o'limining ko'payishi sabablarini muhokama qilish uchun konferentsiya o'tkazdi; nemis tadqiqotlaridan bexabar, ular o'zlarini rejalashtirishdi va boshlashdi.[14]
1950 yilda AQSh va Buyuk Britaniya tadqiqotchilari tomonidan nashr etilgan beshta ish nazorati bo'yicha tadqiqotlar keng e'tiborni tortdi.[27] Eng kuchli natijalar "Chekish va o'pkaning karsinomasi. Dastlabki hisobot" tomonidan aniqlandi Richard Doll va Ostin tepaligi,[28][14] va 1950 yil Vaynder va Grem tadqiqotlari, "Tamaki chekish bronxiogen karsinomaning mumkin bo'lgan etiologik omili sifatida: olti yuz sakson to'rt isbotlangan holatni o'rganish" deb nomlangan. Ushbu ikkita tadqiqot eng katta tadqiqot bo'lib, sobiq chekuvchilarni chekuvchilar guruhidan ehtiyotkorlik bilan chiqarib tashlashdi. Qolgan uchta tadqiqotda, shuni ta'kidlash mumkinki, "chekish kuchli o'pka saratoniga sabab bo'lgan".[27] Doll and Hill gazetasida "og'ir sigaret chekuvchilar chekmaydiganlarga qaraganda ellik barobar ko'p o'pka saratoniga chalinganligi" xabar qilingan.[28][27]
Sabablilik
Holat nazorati bo'yicha o'tkazilgan tadqiqotlar chekish va o'pka saratoni, lekin namoyish qilmagani uchun tanqid qilindi nedensellik. Kuzatuv katta istiqbolli kohort tadqiqotlari 1950 yillarning boshlarida chekuvchilar tezroq vafot etishlarini va o'pka saratonidan o'lish ehtimoli yuqori ekanligini aniq ko'rsatdilar, yurak-qon tomir kasalliklari, va tadqiqotlar davom etganda uzaygan boshqa kasalliklar ro'yxati[14]
The Britaniya shifokorlari o'qishadi, a uzunlamasına o'rganish 40 mingga yaqin shifokorlarning 1951 yilda boshlangan.[29] 1954 yilga kelib u erda shifokorlarning uch yillik o'limidan dalillar bor edi, shu asosda hukumat chekish va o'pka saratoni ko'rsatkichlari bir-biriga bog'liq degan maslahat berdi.[30][29] (the Britaniya shifokorlari o'qishadi oxirgi marta 2001 yilda xabar qilingan,[29] shu vaqtgacha ≈40 ta bog'liq kasalliklar bo'lgan).[14] The Britaniya shifokorlari o'qishadi 1900-1909 yillarda tug'ilgan doimiy sigaret chekuvchilarning yarmiga yaqini o'zlarining qaramligidan o'ldirilganligini namoyish etdi ( logarifmlar 35-70, 70-80 va 80-90 yillarda omon qolish ehtimoli) va 1920-yillarda tug'ilgan doimiy sigaret chekuvchilarning uchdan ikki qismi, oxir-oqibat, ularning giyohvandligi tufayli o'ldiriladi.[iqtibos kerak ]
Jamiyatning xabardorligi
1953 yilda olimlar Sloan-Kettering instituti Nyu-York shahrida sichqonlar terisiga bo'yalgan sigaret qatroni o'limga olib keladigan saraton kasalligini keltirib chiqardi.[26] Ushbu ish ommaviy axborot vositalarining katta e'tiborini tortdi; The Nyu-York Tayms va Hayot ikkalasi ham masalani yoritgan. The Reader Digest "Kartonli saraton" nomli maqola chop etdi.[26]:14
1964 yil 11 yanvarda AQSh Bosh jarroh "s Chekish va sog'liq to'g'risida hisobot nashr etildi; bu millionlab amerikalik chekuvchilarni tark etishga, ba'zi reklamalarni taqiqlashga va tamaki mahsulotlariga ogohlantiruvchi yorliqlarni talab qilishga olib keldi.[iqtibos kerak ]
Ushbu natijalar birinchi bo'lib 60-yillarning o'rtalarida tibbiyot jamoatchiligida keng qabul qilindi va keng jamoatchilik orasida e'lon qilindi.[14] Tibbiy jamoatchilikning tamaki kasallikka chalinganligi haqidagi fikriga nikotinga qaram bo'lgan shifokorlarning tarafkashligi, yuqumli bo'lmagan kasalliklarga epidemiologik texnika va evristikani qo'llash uchun zarur bo'lgan moslashuvning yangiligi va tamaki sanoatining bosimi sabab bo'lgan.[14]
Chekishning sog'likka ta'siri ta'siri fanining rivojlanishi uchun muhim ahamiyatga ega epidemiologiya. Kanserogenlik mexanizmi radiomimetik yoki rentgenologik bo'lgani uchun, ta'sirlar stoxastik. Muayyan bayonotlar faqat ma'lum bir kasallikka chalinish ehtimoli nisbatan kamaygan yoki kamayganligi to'g'risida berilishi mumkin. Muayyan shaxs uchun tamaki tutuni va undan keyingi saraton kabi radiomimetik zahar ta'sirlanishining to'g'ridan-to'g'ri sababiy bog'liqligini aniq isbotlash mumkin emas; bunday bayonotlar faqat umumiy aholi darajasida bo'lishi mumkin. Tamaki ishlab chiqaruvchi kompaniyalar ushbu falsafiy e'tirozdan foydalanib, toksikani haqiqiy kasallik sifatida stoxastik ifodalashdagi sababiy bog'liqlik to'g'risida faqat ayrim holatlarni ko'rib chiqadigan klinisyenlarning shubhalarini ishlatishdi.[31]
Tamaki ishlab chiqaradigan kompaniyalarga nisbatan tamaki mahsulotlarining sog'liqqa ta'sirini o'rganib chiqqani uchun bir necha bor sud ishlari bo'lib o'tdi, ammo keyin topilmalarni bostirdi yoki ularni kamaytirilganligi yoki hech qanday xavf tug'dirmaydigan qilib formatladi.[31]
2006 yil mart oyida Shotlandiyada barcha yopiq jamoat joylarida chekishni taqiqlash joriy qilinganidan keyin 17 foizga pasayish yuz berdi[qachon? ] o'tkir koronar sindromga kasalxonaga yotqizilganida. Kamayishning 67 foizi chekmaydiganlarga to'g'ri keladi.[32]
Chekishning sog'liqqa ta'siri

Chekish odatda yurakka ta'sir qiladigan kasalliklarga olib keladi o'pka va odatda qo'llar yoki oyoqlar kabi joylarga ta'sir qiladi. Chekish bilan bog'liq sog'liqqa oid birinchi muammolarning alomatlari ko'pincha ekstremitalarda uyqusizlik bo'lib namoyon bo'ladi, chunki chekish asosiy xavf omilidir yurak xurujlari, surunkali obstruktiv o'pka kasalligi (KOAH), amfizem va saraton, ayniqsa o'pka saratoni, saraton kasalligi gırtlak va og'iz va oshqozon osti bezi saratoni.[34] Uzoq muddatli chekuvchilarda umr ko'rish davomiyligi ham qisqaradi, taxminlarga ko'ra 10 ga teng[29] 17.9 gacha[35] chekuvchilarga qaraganda yil kamroq.[36] Uzoq muddatli erkak sigaret chekuvchilarning taxminan yarmi chekish sababli kasallik tufayli vafot etadi.[37] Chekishning o'pka saratoni bilan bog'liqligi jamoatchilik fikri va etiologik jihatdan eng kuchli hisoblanadi. Erkak chekuvchilar orasida umr bo'yi o'pka saratoniga chalinish xavfi 17,2% ni tashkil qiladi; sigaret chekadigan ayollar orasida bu xavf 11,6% ni tashkil qiladi. Sigaret chekmaydiganlarda bu xavf sezilarli darajada past: erkaklarda 1,3% va ayollarda 1,4%.[38]
Biror kishi ko'paygan xavf yuqtirish kasalliklari odam chekishni davom etishi va chekilgan miqdori bilan bog'liq. Biroq, kuniga bir dona sigareta chekish ham xavfni oshiradi yurak tomirlari kasalligi taxminan 50% yoki undan ko'proqqa, va uchun qon tomir taxminan 30% ga. Kuniga 20 dona sigaret chekish yuqori xavfni keltirib chiqaradi, ammo mutanosib ravishda emas.[39][40]
Agar kimdir chekishni tashlasa, unda bu ehtimollik asta-sekin kamayadi, chunki tanadagi zarar tiklanadi. Ishdan bo'shatilgandan bir yil o'tgach, yurak xastaligiga chalinish xavfi sigaret chekadigan odamning yarmiga teng.[41] Chekishning sog'liq uchun xavfliligi barcha chekuvchilarda bir xil emas. Xavf chekadigan tamaki miqdoriga qarab farq qiladi, ko'proq chekadiganlar ko'proq xavf ostida. "Engil" deb nomlangan sigaret chekish xavfni kamaytirmaydi.[42]
O'lim
Chekish yiliga 5 millionga yaqin o'limga sabab bo'ladi.[43] Bu uni oldini olish mumkin bo'lgan erta o'limning eng keng tarqalgan sababiga aylantiradi.[44] Bir tadqiqot shuni ko'rsatdiki, sigaret chekadigan erkak va ayol o'rtacha 13,2 va 14,5 yillik hayotlarini yo'qotadi.[45] Boshqasi 6,8 yillik hayot yo'qotishlarini aniqladi.[46] Har bir chekilgan sigaret o'rtacha 11 daqiqani qisqartirishi taxmin qilinmoqda.[47][48][49] Butun umr chekuvchilarning kamida yarmi chekish natijasida erta vafot etadi.[29] Chekuvchilar 60 yoki 70 yoshgacha vafot etish ehtimoli chekuvchilarga qaraganda uch baravar ko'p.[29][50][51]
Qo'shma Shtatlarda sigaret chekish va tamaki tutuniga ta'sir qilish taxminan har beshinchi kishidan iborat,[52] yoki har yili kamida 443,000 bevaqt o'lim.[53] Buni kontekstga kiritish uchun ABC Piter Jennings (keyinchalik umrbod chekish odati tufayli o'pka saratonining asoratlaridan 67 yoshida vafot etgan) mashhur AQShda faqat tamaki uchga teng odam o'ldiradi jumbo jets har kuni halokatga uchragan odamlarga to'la, tirik qolganlari yo'q.[54] Dunyo miqyosida bu har soatda bitta jumbo jetga teng.[55]
2015 yilgi tadqiqotlar shuni ko'rsatdiki, Qo'shma Shtatlarda sigareta chekish sababli o'limning taxminan 17 foizi odatda bog'liq deb hisoblanadigan kasalliklardan tashqari.[56]
Hisob-kitoblarga ko'ra, har million sigareta uchun 1 dan 1,4 gacha o'lim holatlari mavjud. Darhaqiqat, sigaret ishlab chiqaradigan fabrikalar dunyo tarixidagi eng halokatli zavodlardir.[57][58] Eng ko'p ishlab chiqariladigan sigareta ishlab chiqaradigan fabrikalar va ularning har yili sog'lig'iga zarar etkazishi sababli ularning o'limiga olib keladigan o'lchovlar haqidagi quyidagi jadvalga qarang.[57]

Chekishdan o'lganlarning ulushi, 2017 y[59]

2017 yilda 100 ming kishiga to'g'ri keladigan chekish bilan bog'liq o'limlar soni[60]
Saraton

Tamaki iste'mol qilishning asosiy xavflari orasida ko'plab saraton turlari, xususan o'pka saratoni,[62] buyrak saratoni,[63] gırtlak saratoni va bosh va bo'yin,[64][65] qovuq saratoni,[66] qizilo'ngach saratoni,[67] oshqozon osti bezi saratoni[68] va oshqozon saratoni.[69] Tadqiqotlar tamaki tutuni, shu jumladan ikkilamchi tutun va bachadon bo'yni saratoni ayollarda.[70] Xavfning ozgina oshganligini ko'rsatadigan ba'zi dalillar mavjud miyeloid leykemiya,[71] skuamöz hujayrali sinonazal saraton, jigar saratoni, kolorektal saraton, saraton kasalligi o't pufagi, buyrak usti bezi, ingichka ichak va turli xil bolalik saratonlari.[69] O'rtasida mumkin bo'lgan aloqa ko'krak bezi saratoni va tamaki hali ham noaniq.[72][tibbiy ma'lumotnoma kerak ]
O'pka saratoni xavfi chekishga juda ta'sir qiladi, 90% hollarda tamaki chekish sabab bo'ladi.[73] O'pka saratoniga chalinish xavfi bir necha yil chekish va kuniga chekilgan sigaretalar soniga qarab ortadi.[74] Chekishni o'pka saratonining barcha pastki turlari bilan bog'lash mumkin. Kichik hujayrali karsinoma (SCLC) sigaret chekuvchilarda yuzaga keladigan deyarli 100% holatlar bilan eng yaqin bog'liqdir.[75] Saratonning ushbu shakli avtokrin o'sish davri bilan aniqlangan, proto-onkogen ning faollashishi va inhibatsiyasi o'smani bostiruvchi genlar. SCLC Feyrter hujayralari deb nomlangan bronxda joylashgan neyroendokrin hujayralardan kelib chiqishi mumkin.[76]
85 yoshgacha o'pka saratonidan vafot etish xavfi, o'limga sabab bo'ladigan sabablar bo'lmagan taqdirda, chekuvchi erkaklarda 22,1%, ayollarda 11,9%. Bir umr chekmaydiganlar uchun tegishli taxminlar Evropa kelib chiqishi bo'lgan erkak uchun 85 yoshgacha o'pka saratonidan o'lish ehtimoli 1,1% ni, ayol uchun 0,8% ni tashkil etadi.[77]
O'pka

Chekishda tutun tarkibidagi birikmalarga uzoq vaqt ta'sir qilish (masalan, uglerod oksidi va siyanid ) o'pkaning shikastlanishi va elastiklik yo'qolishi uchun javobgardir deb ishoniladi alveolalar, amfizemaga va KOAHga olib keladi. Surunkali obstruktiv o'pka kasalligi Chekish oqibatida kelib chiqqan (KOAH) - bu nafas qisilishi, xirillash, doimiy yo'tal bilan ifodalangan o'pka qobiliyatini doimiy, davolanmaydigan (ko'pincha terminal) pasayishi. balg'am va o'pkaning shikastlanishi, shu jumladan amfizem va surunkali bronxit.[78] Kanserogen akrolein va uning hosilalari KOAHda mavjud bo'lgan surunkali yallig'lanishni keltirib chiqaradi.[79]
Yurak-qon tomir kasalliklari
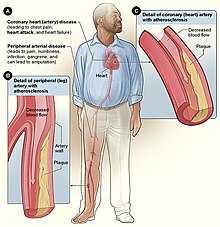

Tamaki tutunini nafas olish yurak va qon tomirlarida bir nechta tezkor ta'sirlarni keltirib chiqaradi. Bir daqiqada yurak urish tezligi ko'tarila boshlaydi, chekishning dastlabki 10 daqiqasida 30 foizga ko'payadi. Tamaki tutunidagi uglerod oksidi ta'sir qiladi salbiy ta'sir qonning kislorod tashish qobiliyatini kamaytirish orqali.[80]
Chekish ham imkoniyatni oshiradi yurak kasalligi, qon tomir, ateroskleroz va periferik qon tomir kasalligi.[81][82] Tamakining bir nechta tarkibiy qismlari qon tomirlarining torayishiga olib keladi, tiqilib qolish ehtimolini oshiradi va shu bilan a yurak xuruji yoki qon tomir. Xalqaro guruhi tomonidan o'tkazilgan tadqiqotga ko'ra tadqiqotchilar, 40 yoshgacha bo'lgan odamlar chekishsa, yurak xurujiga chalinish ehtimoli besh baravar yuqori.[83][84]
Tamaki tutuniga ta'sir qilish tanadagi oksidlanish stresini turli xil mexanizmlar, shu jumladan plazmadagi antioksidantlarning kamayishi bilan kuchaytirishi ma'lum. S vitamini.[85]
Amerikalik biologlarning so'nggi tadqiqotlari shuni ko'rsatdiki, sigaretaning tutuni yurak mushaklaridagi hujayralarni bo'linish jarayoniga ham ta'sir qiladi va yurak shaklini o'zgartiradi.[86]
Shuningdek, tamakidan foydalanish bilan bog'liq Buerger kasalligi (tromboangiit obliterans) qo'l va oyoq tomirlari va tomirlarining o'tkir yallig'lanishi va trombozi (pıhtılaşma).[87]
Sigaret chekish saraton xastaligi xavfini sigareta chekishga qaraganda ko'proq ko'payishiga olib keladigan bo'lsa-da, sigaret chekuvchilar sigaret chekmaydiganlar bilan taqqoslaganda ko'plab sog'liq muammolari, shu jumladan saraton xastaligi xavfini oshiradi.[88][89] Ikkinchi qo'l tutunga kelsak, NIH tadqiqotida bitta puro tomonidan hosil bo'lgan tutunning ko'pligi ta'kidlanib, "purolar ichki muhitga katta miqdordagi tamaki tutunini qo'shishi mumkin; va ko'plab sigaret chekuvchilar sigaret chekishda to'planishganda. Hodisada ishlab chiqarilgan ETS (ya'ni ikkinchi darajali tutun) miqdori ushbu muhitda ishlash uchun muntazam ravishda talab qilinadiganlar uchun sog'liq uchun etarli bo'ladi. "[90]
Chekish moyil qonda xolesterin miqdorini oshirish. Bundan tashqari, ning nisbati yuqori zichlikdagi lipoprotein (HDL, shuningdek, "yaxshi" xolesterin deb ham ataladi) ga past zichlikdagi lipoprotein (LDL, shuningdek, "yomon" xolesterin deb ham ataladi) chekuvchilarda chekuvchilarga nisbatan pastroq bo'ladi. Chekish ham darajalarini oshiradi fibrinogen va ortadi trombotsit qonning quyuqlashishi va pıhtılaşma ehtimoli yuqori bo'lgan ishlab chiqarish (ikkalasi ham qon ivishida ishtirok etadi). Uglerod oksidi gemoglobin bilan (qizil qon hujayralarida kislorod tashiydigan tarkibiy qism) bog'lanib, natijada kislorod yoki karbonat angidrid bilan bog'langan gemoglobinga qaraganda ancha barqaror kompleks hosil qiladi - natijada qon hujayralari faoliyati doimiy ravishda yo'qoladi. Qon hujayralari ma'lum vaqtdan so'ng tabiiy ravishda qayta ishlanib, yangi, funktsional qizil qon hujayralarini yaratishga imkon beradi. Ammo, agar uglerod oksidiga ta'sir qilish ularni qayta ishlashdan oldin ma'lum bir nuqtaga yetsa, gipoksiya (va keyinchalik o'lim) paydo bo'ladi. Bu omillarning barchasi chekuvchilarni turli xil shakllarni rivojlanish xavfiga ko'proq moyil qiladi arterioskleroz (tomirlarning qattiqlashishi). Arterioskleroz rivojlanib borgan sari, qattiq va toraygan qon tomirlari orqali qon osonlikcha oqadi va qon tromboz (pıhtı) hosil qilish ehtimoli yuqori bo'ladi. Qon tomirining to'satdan to'sib qo'yilishi infarktga olib kelishi mumkin (qon tomir yoki yurak xuruji). Shu bilan birga, shuni ham ta'kidlash joizki, chekishning yurakka ta'siri yanada nozikroq bo'lishi mumkin. Ushbu holatlar chekishni davolovchi tsiklni hisobga olgan holda asta-sekin rivojlanishi mumkin (chekish davrlari orasida inson tanasi o'zini davolaydi) va shuning uchun chekuvchi noxush dermatologik holatlarning yomonlashishi yoki saqlanib qolishi kabi ahamiyatsiz kasalliklarga duch kelishi mumkin. ekzema, qon ta'minoti kamayganligi sababli. Chekish ham ko'payadi qon bosimi va qon tomirlarini susaytiradi.[91]
Buyrak
Buyrak saratoni xavfini oshirishdan tashqari, chekish ham qo'shimcha hissa qo'shishi mumkin buyrak zarar. Sigaret chekuvchilar uchun sezilarli darajada xavf tug'diradi surunkali buyrak kasalligi chekmaydiganlarga qaraganda.[92] Chekish tarixi rivojlanishni rag'batlantiradi diabetik nefropatiya.[93]
Gripp
336 nafar sog'lom yigitdan iborat Isroil harbiy qismida (H1N1) grippining tarqalishini sigareta chekishni klinik ko'rinishda gripp bilan kasallanish bilan bog'liqligini aniqlash maqsadida o'tkazilgan tadqiqotlar shuni ko'rsatdiki, 168 nafar chekuvchilarning 68,5 foizida gripp bor. chekuvchilarning 47,2 foizi bilan. Gripp chekuvchilarda ham og'irroq bo'lgan; Ularning 50,6 foizi chekilganlarning 30,1 foiziga nisbatan ish kunlarini yo'qotgan yoki yotoqda dam olishni talab qilganlar, yoki ikkalasi ham.[94]
Janubiy Karolina harbiy akademiyasida 1968 yil Gonkong A2 grippi epidemiyasidan so'ng 1900 erkak kursantlar o'rtasida o'tkazilgan tadqiqotga ko'ra, chekuvchilar bilan taqqoslaganda, og'ir chekuvchilar (kuniga 20 dan ortiq sigareta) 21% ko'proq kasallikka chalingan va 20% ko'proq yotoqda dam olish, engil chekuvchilar (kuniga 20 ta sigareta yoki undan kam) 10% ko'proq kasallikka va 7% ko'proq yotoqda dam olishgan.[95]
Sigaretani chekishning epidemik grippga ta'siri 1811 erkak kollej o'quvchilari o'rtasida istiqbolli ravishda o'rganildi. Kundalik ravishda 21 va undan ortiq sigareta chekadiganlar orasida grippning klinik kasallanish darajasi chekmaydiganlarga qaraganda 21 foizga ko'pdir. Kuniga 1 dan 20 tagacha sigaret chekuvchilar orasida gripp bilan kasallanish chekmaydiganlar va og'ir sigaret chekuvchilar o'rtasida oraliq bo'lgan.[95]
1979 yilda Isroildagi ayollar uchun harbiy bazada gripp epidemiyasi kuzatilganda, gripp belgilari hozirgi chekuvchilarning 60.0 foizida va 41.6 foizida chekuvchilarda paydo bo'lganligi aniqlandi.[96]
Chekish yoshi kattaroq populyatsiyalarda nisbatan yuqori gripp xavfini keltirib chiqaradi. 1993- yil davomida 60-90 yoshdagi aholi yashaydigan odamlarni istiqbolli tadkikotida immunizatsiya qilinmagan odamlarning 23% sigaret chekadiganlar chekadiganlarning 6% bilan solishtirganda klinik grippga chalingan.[97]
Chekish butun aholini qamrab oladigan gripp epidemiyasining o'sishiga katta hissa qo'shishi mumkin.[94] Shu bilan birga, sigaret chekmaydiganlarning umumiy sonida gripp bilan kasallanishning sigaret chekuvchilarning ulushi hali aniqlanmagan.[iqtibos kerak ]
Og'iz

Ehtimol, paydo bo'lishi mumkin bo'lgan eng jiddiy og'iz holati shu og'iz saratoni. Shu bilan birga, chekish boshqa turli xil og'iz kasalliklari xavfini oshiradi, ba'zilari esa tamaki iste'molchilariga deyarli mutlaqo eksklyuzivdir. The Milliy sog'liqni saqlash institutlari, orqali Milliy saraton instituti, 1998 yilda "tamaki chekish turli xil saratonlarni, shu jumladan saratonni keltirib chiqarishi aniqlandi og'iz bo'shlig'i (lab, til, og'iz, tomoq), qizilo'ngach, gırtlak va o'pka."[90] Quvur chekish sog'liq uchun katta xavf tug'diradi,[98][99] ayniqsa og'iz saratoni.[100] Taxminan yarmi periodontit yoki tish atrofidagi yallig'lanish holatlari hozirgi yoki ilgari chekish bilan bog'liq. Tutunsiz tamaki sabablari gingival retsessiya va oq mukozal jarohatlar. Periodontit bilan og'rigan bemorlarning 90% gacha davolashning umumiy usullari yordam bermaydi. Sigaret chekuvchilar chekadiganlarga qaraganda suyaklarning balandligini sezilarli darajada ko'proq yo'qotishadi va bu chekish chekuvchilarga qaraganda ko'proq suyaklarning yo'qolishiga olib kelishi mumkin.[101]
Chekish tishlarni bo'yashda muhim omil ekanligi isbotlangan.[102][103] Galitoz yoki yomon hid tamaki chekuvchilar orasida keng tarqalgan.[104] Tishlarning yo'qolishi 2 ga teng ekanligi ko'rsatilgan[105] 3 martagacha[106] chekuvchilarda chekuvchilarga qaraganda ko'proq.[107] Bundan tashqari, asoratlar o'z ichiga olishi mumkin leykoplakiya, og'iz bo'shlig'ining shilliq pardalarida, shu jumladan tilda yopishgan oq plakatlar yoki yamaqlar.[108]
Infektsiya
Chekish yuqumli kasalliklarga, xususan o'pkada sezuvchanlik bilan ham bog'liq (zotiljam ). 20 dan ortiq chekish sigaretalar kuniga sil kasalligi xavfini ikki-to'rt baravar oshiradi,[109][110] va hozirgi chekuvchi bo'lib, patogen bakteriyalar sabab bo'lgan invaziv kasallik xavfining to'rt barobar ko'payishi bilan bog'liq. Streptokokk pnevmoniyasi.[111] Chekish bu va boshqa o'pka va nafas yo'llarining infektsiyalari xavfini strukturaning shikastlanishi va immunitet tizimiga ta'sir qilish orqali oshiradi deb ishoniladi. Immunitet tizimiga ta'siri CD4 + hujayralari ishlab chiqarishning nikotin bilan bog'liqligini o'z ichiga oladi, bu taxminiy ravishda OIVga sezuvchanlikning oshishi bilan bog'liq.[112]
Chekish xavfini oshiradi Kaposhi sarkomasi bo'lmagan odamlarda OIV infektsiyasi.[113] Bir tadqiqot shuni aniqladiki, faqat erkaklar populyatsiyasi bilan o'tkazilgan va tadqiqotning ayol ishtirokchilari uchun biron bir xulosaga kelmagan.[114]
Jinsiy ojizlik
Hodisa iktidarsizlik (jinsiy olatni erektsiyasiga erishish va uni saqlashda qiyinchilik) chekuvchilarga nisbatan chekuvchilarga nisbatan 85 foizga yuqori.[115] Chekish erektil disfunktsiyaning (ED) asosiy sababidir.[12][115] Bu iktidarsizlikni keltirib chiqaradi, chunki u targ'ib qiladi arterial torayish va zarar tomirlarning ichki qismini qoplagan hujayralar shuning uchun jinsiy olatni qon oqimini kamaytirishga olib keladi.[116]
Ayollarning bepushtligi
Chekish zararli hisoblanadi tuxumdonlar, potentsial sabab bo'lishi mumkin ayollarning bepushtligi, va zarar darajasi ayolning chekishi va davomiyligiga bog'liq. Sigaretadagi nikotin va boshqa zararli kimyoviy moddalar organizmning yaratilish qobiliyatiga xalaqit beradi estrogen, a gormon tartibga soluvchi follikulogenez va ovulyatsiya. Shuningdek, sigaret chekish follikulogenezga, embrionni tashishga xalaqit beradi. endometrial retseptivlik, endometrial angiogenez, bachadon qon oqimi va bachadon myometrium.[117] Ba'zi bir zararlarni qaytarib bo'lmaydi, ammo chekishni to'xtatish ko'proq zararni oldini oladi.[118][119] Chekuvchilar chekmaydiganlarga qaraganda 60 foiz ko'proq bepusht bo'lishadi.[120] Chekish ehtimoli kamayadi ekstrakorporal urug'lantirish (IVF) tirik tug'ilishni 34% ga oshiradi va EKT bilan homiladorlikning uzilish xavfini 30% ga oshiradi.[120]
Psixologik
Amerika psixologi "Chekuvchilar tez-tez chekish stressni engillashishiga yordam berishini ta'kidlaydilar. Ammo kattalardagi chekuvchilarning stress darajasi chekmaydiganlarga nisbatan bir oz yuqori, o'spirin sigaret chekuvchilar odatdagidek chekishni kuchaytirayotgani sababli stress kuchayib borayotgani haqida xabar berishadi. Nikotinga bog'liqlik kayfiyatni nazorat qilishda yordamchi rolini bajarishdan uzoqroq bo'lib, stressni kuchaytiradi, bu chekuvchilar tomonidan tasvirlangan kunlik kayfiyat tartibida, chekish paytida odatdagi kayfiyat va sigaretalar orasidagi kayfiyatning yomonlashuvi. Shunday qilib, chekish faqat davomida paydo bo'ladigan taranglik va asabiylikni qaytarishini aks ettiradi nikotinning etishmasligi. O'ziga qaram bo'lgan chekuvchilar odatdagidek bo'lishlari uchun nikotin kerak. "[121]
Darhol ta'sir
Foydalanuvchilar hissiyotlari haqida xabar berishadi dam olish, aniqlik, xotirjamlik va hushyorlik.[122] Chekishni yangi boshlaganlar duch kelishi mumkin ko'ngil aynish, bosh aylanishi, qon bosimining oshishi, tomirlarning torayishi va tez yurak urishi. Umuman olganda, noxush alomatlar vaqt o'tishi bilan yo'q bo'lib ketadi, takroriy foydalanish bilan, chunki tanani qurish a bag'rikenglik kabi sigaretadagi kimyoviy moddalarga nikotin.[iqtibos kerak ]
Stress
Chekuvchilar kundalik turmush tarzining yuqori darajasi haqida xabar berishadi.[123] Bir nechta tadqiqotlar vaqt o'tishi bilan stress hissiyotlarini kuzatib bordi va ishdan bo'shatgandan so'ng kamaygan stressni aniqladi.[124][125]
Tiyishdan saqlanishning zararli kayfiyat ta'siri, chekuvchilar nima uchun chekuvchilarga qaraganda ko'proq kunlik stressni boshdan kechirayotganlarini va chekishni tashlaganlarida kam stressli bo'lishlarini tushuntiradi. Mahrum qilishni bekor qilish, shuningdek, qo'zg'alish ma'lumotlarining aksariyatini tushuntiradi, chekilgan chekuvchilar chekmaydigan yoki chekmaydiganlarga qaraganda kamroq hushyor va kamroq ogoh bo'lishadi.[123]
So'nggi tadqiqotlar psixologik bezovtalik va tupurik o'rtasidagi ijobiy munosabatni ko'rsatdi kotinin chekish va chekmaydigan kattalardagi darajalar, bu ham chekish, ham chekish chekish, ruhiy stressning yuqori darajasiga olib kelishi mumkin.[126]
Ijtimoiy va xulq-atvorli
Tibbiyot tadqiqotchilari chekishni ajrashishni bashorat qilishini aniqladilar.[127] Chekuvchilarning ajralish ehtimoli chekuvchilarga nisbatan 53% ko'proq.[128]
Kognitiv funktsiya
Tamakidan foydalanish kognitiv disfunktsiyani ham keltirib chiqarishi mumkin. Xavfning ko'payishi ko'rinadi Altsgeymer kasalligi, garchi "ish nazorati va kohort tadqiqotlari chekish va AD o'rtasidagi bog'liqlik yo'nalishi bo'yicha qarama-qarshi natijalarga olib keladi".[129] Chekish demansga va kognitiv pasayishga hissa qo'shishi aniqlandi,[130] o'spirinlarda xotira va bilish qobiliyatining pasayishi,[131] va miyaning qisqarishi (miya atrofiyasi).[132][133]
Shunisi e'tiborliki, ba'zi tadqiqotlar Altsgeymer kasalligi bilan og'rigan bemorlarning chekish ehtimoli keng populyatsiyaga qaraganda ko'proq ekanligini aniqladilar, bu esa chekish Altsgeymerga qarshi bir oz himoya qiladi degan fikr bilan izohlanadi. Biroq, bu sohadagi tadqiqotlar cheklangan va natijalar qarama-qarshi; ba'zi tadqiqotlar shuni ko'rsatadiki, chekish Altsgeymer kasalligi xavfini oshiradi.[134] Yaqinda mavjud bo'lgan ilmiy adabiyotlarni o'rganish natijasida Altsgeymer xavfining pasayishi shunchaki chekuvchilar odatda Altsgeymer paydo bo'lgan yoshga etmasdan o'lishga moyil bo'lishlari mumkin degan xulosaga kelishdi. "Differentsial o'lim har doim muammo bo'lib, altsgeymer kasalligi bo'lgan 75 yoshgacha kasallanish darajasi juda past bo'lgan buzuqlikda chekishni ta'sirini tekshirishga ehtiyoj bor", deyiladi unda. sigaret chekmaydiganlarning 80 yoshigacha omon qolish ehtimoli atigi yarmi.[129]
Ba'zi eski tahlillar, chekmaydiganlar Altsgeymer kasalligiga chalinish ehtimoli chekuvchilarga qaraganda ikki baravar ko'p ekanligini ta'kidladilar.[135] Biroq, zamonaviy tahlil shuni ko'rsatdiki, profilaktika ta'sirini ko'rsatgan tadqiqotlarning aksariyati tamaki sanoati bilan yaqin aloqada bo'lgan. Tamaki lobbisi ta'siriga ega bo'lmagan tadqiqotchilar mutlaqo teskari xulosaga kelishdi: chekuvchilar Altsgeymer kasalligiga chalinganlarga qaraganda deyarli ikki baravar ko'pdir.[136]
Ilgari va hozirgi chekuvchilar kamroq kasallangan Parkinson kasalligi hech qachon chekmagan odamlarga nisbatan,[137][138] Mualliflarning ta'kidlashicha, Parkinson kasalligining bir qismi bo'lgan harakatlanish buzilishi odamlarni chekishga to'sqinlik qilishi, chekishning o'zi himoya qilishdan ko'ra ko'proq. Boshqa bir tadqiqotda Parkinson xavfini kamaytirishda nikotinning mumkin bo'lgan o'rni ko'rib chiqildi: nikotin dopaminerjik Parkinson kasalligida zararlangan miyaning tizimi, tamaki tutunidagi boshqa birikmalar esa inhibe qiladi MAO-B, dopaminni parchalash orqali oksidlovchi radikallar hosil qiluvchi ferment.[139]
Ko'p jihatdan, nikotin shunga o'xshash tarzda asab tizimida harakat qiladi kofein. Ba'zi yozuvlarda chekish ham ko'payishi mumkinligi aytilgan aqliy konsentratsiya; bitta tadqiqot hujjatlari normativlar bo'yicha ko'rsatkichlarni sezilarli darajada yaxshilaydi Advanced Raven Progressive Matrices testi chekishdan keyin.[140]
Aksariyat chekuvchilar, ularga kirish taqiqlanganda nikotin, asabiylashish, jitteriness, quruq og'iz va tez yurak urishi.[141] Ushbu alomatlarning paydo bo'lishi juda tez, nikotinning yarim umri atigi 2 soat.[142] The psixologik qaramlik bir necha oy yoki hatto ko'p yillar davom etishi mumkin. Ba'zilaridan farqli o'laroq rekreatsion dorilar, nikotin chekuvchi odamni o'lchov bilan o'zgartirmaydi vosita qobiliyatlari, hukm, yoki til dori ta'sirida bo'lgan qobiliyatlar. Tamakidan voz kechish klinik jihatdan jiddiy qayg'uga olib kelishi isbotlangan.[143]
A very large percentage of schizophrenics smoke tobacco as a form of self-medication.[144][145][146][147] The high rate of tobacco use by the mentally ill is a major factor in their decreased life expectancy, which is about 25 years shorter than the general population.[148] Following the observation that smoking improves condition of people with schizophrenia, in particular working memory deficit, nikotin yamoqlari had been proposed as a way to treat schizophrenia.[149] Some studies suggest that a link exists between smoking and mental illness, citing the high incidence of smoking amongst those suffering from shizofreniya[150] and the possibility that smoking may alleviate some of the symptoms of mental illness,[151] but these have not been conclusive. In 2015, a meta-analysis found that smokers were at greater risk of developing psychotic illness.[152]
Recent studies have linked smoking to anxiety disorders, suggesting the correlation (and possibly mechanism) may be related to the broad class of anxiety disorders, and not limited to just depression. Current and ongoing research attempt to explore the addiction-anxiety relationship. Data from multiple studies suggest that anxiety disorders and depression play a role in cigarette smoking.[153] A history of regular smoking was observed more frequently among individuals who had experienced a katta depressiv buzilish at some time in their lives than among individuals who had never experienced major depression or among individuals with no psychiatric diagnosis.[154] People with major depression are also much less likely to chiqish due to the increased risk of experiencing mild to severe states of depression, including a major depressive episode.[155] Depressed smokers appear to experience more withdrawal symptoms on quitting, are less likely to be successful at quitting, and are more likely to relapse.[156]
Homiladorlik
A number of studies have shown that tobacco use is a significant factor in tushish orasida homilador smokers, and that it contributes to a number of other threats to the health of the fetus. It slightly increases the risk of asab naychasining nuqsonlari.[157]
Environmental tobacco smoke exposure and maternal smoking during pregnancy have been shown to cause lower infant birth weights.[158]
Studies have shown an association between prenatal exposure to environmental tobacco smoke and conduct disorder in children.[tibbiy ma'lumotnoma kerak ] As well, post-natal tobacco smoke exposure may cause similar behavioral problems in children.[tibbiy ma'lumotnoma kerak ]
Dori vositalarining o'zaro ta'siri
Smoking is known to increase levels of liver enzymes that break down drugs and toxins. That means that drugs cleared by these enzymes are cleared more quickly in smokers, which may result in the drugs not working. Specifically, levels of CYP1A2 and CYP2A6 are induced:[159][160] substrates for 1A2 include kofein and tricyclic antidepressants such as amitriptilin; substrates for 2A6 include the anticonvulsant, valproik kislota.
Multigenerational effects
Other harm

Studies suggest that smoking decreases appetite, but did not conclude that overweight people should smoke or that their health would improve by smoking. This is also a cause of heart diseases.[161] Smoking also decreases weight by overexpressing the gene AZGP1 bu rag'batlantiradi lipoliz.[162]
Smoking causes about 10% of the global burden of fire deaths,[163] and smokers are placed at an increased risk of injury-related deaths in general, partly due to also experiencing an increased risk of dying in a motor vehicle crash.[164]
Smoking increases the risk of symptoms associated with Crohn kasalligi (a dose-dependent effect with use of greater than 15 cigarettes per day).[165][166][167][168] There is some evidence for decreased rates of endometrioz in infertile smoking women,[169] although other studies have found that smoking increases the risk in infertile women.[170] There is little or no evidence of a protective effect in fertile women. Some preliminary data from 1996 suggested a reduced incidence of bachadon miomasi,[171] but overall the evidence is unconvincing.[172]
Current research shows that tobacco smokers who are exposed to residential radon are twice as likely to develop lung cancer as non-smokers.[173] As well, the risk of developing lung cancer from asbestos exposure is twice as likely for smokers than for non-smokers.[174]
New research has found that women who smoke are at significantly increased risk of developing an qorin aorta anevrizmasi, a condition in which a weak area of the qorin aorta expands or bulges, and is the most common form of aorta anevrizmasi.[175]
Smoking leads to an increased risk of bone fractures, especially hip fractures.[176] It also leads to slower wound-healing after surgery, and an increased rate of postoperative healing complication.[177]
Tobacco smokers are 30-40% more likely to develop 2-toifa diabet than non-smokers, and the risk increases with the number of cigarettes smoked. Furthermore, diabetic smokers have worse outcomes than diabetic non-smokers.[178][179]
Foyda
In addition to the numerous documented negative health effects of smoking, several types of "smoker's paradoxes" (cases where smoking appears to have specific beneficial effects) have been observed.[180] Smoking may prevent Parkinson kasalligi.[181]
Mexanizm
Chemical carcinogens

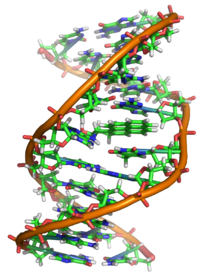
Smoke, or any partially burnt organic matter, contains kanserogenlar (cancer-causing agents). The potential effects of smoking, such as lung cancer, can take up to 20 years to manifest themselves. Historically, women began smoking ommaviy ravishda later than men, so an increased death rate caused by smoking amongst women did not appear until later. The male lung cancer death rate decreased in 1975 — roughly 20 years after the initial decline in cigarette consumption in men. A fall in consumption in women also began in 1975[183] but by 1991 had not manifested in a decrease in lung cancer-related mortalities amongst women.[184]
Smoke contains several carcinogenic pirolitik products that bind to DNK va sabab genetik mutatsiyalar. Particularly potent carcinogens are politsiklik aromatik uglevodorodlar (PAH), which are toxicated ga mutagen epoksidlar. The first PAH to be identified as a carcinogen in tobacco smoke was benzopiren, which has been shown to toxicate into an epoxide that irreversibly attaches to a cell's nuclear DNA, which may either kill the cell or cause a genetic mutation. If the mutation inhibits dasturlashtirilgan hujayralar o'limi, the cell can survive to become a cancer cell. Xuddi shunday, akrolin, which is abundant in tobacco smoke, also irreversibly binds to DNA, causes mutations and thus also cancer. However, it needs no activation to become carcinogenic.[185]
There are over 19 known carcinogens in cigarette smoke.[186] The following are some of the most potent carcinogens:
- Politsiklik aromatik uglevodorodlar bor smola components produced by piroliz in smoldering organic matter and emitted into smoke. Several of these PAH's are already toxic in their normal form, however, many of then can become more toxic to the liver. Tufayli hidrofob nature of PAH's they do not dissolve in water and are hard to expel from the body. In order to make the PAH more soluble in water, the liver creates an enzyme called Sitoxrom P450 which adds an additional kislorod to the PAH, turning it into a mutagen epoksidlar, which is more soluble, but also more reactive.[187] The first PAH to be identified as a carcinogen in tobacco smoke was benzopiren, which been shown to toxicate into a diol epoxide and then permanently attach to nuclear DNA, which may either kill the cell or cause a genetik mutatsiya. The DNA contains the information on how the cell function; in practice, it contains the recipes for protein synthesis. If the mutation inhibits dasturlashtirilgan hujayralar o'limi, the cell can survive to become a cancer, a cell that does not function like a normal cell. The carcinogenicity is radiomimetic, i.e. similar to that produced by ionizing nuclear radiation. Tobacco manufacturers have experimented with combustion less bug'lashtiruvchi technology to allow cigarettes to be consumed without the formation of carcinogenic benzopyrenes.[188] Although such products have become increasingly popular, they still represent a very small fraction of the market, and no conclusive evidence has shown to prove or disprove the positive health claims.[iqtibos kerak ]
- Akrolein is a pyrolysis product that is abundant in cigarette smoke. It gives smoke an acrid smell and an irritating, tear causing effect and is a major contributor to its carcinogenicity. Like PAH metabolites, acrolein is also an electrophilic alkillash agenti and permanently binds to the DNA base guanin, tomonidan conjugate addition followed by cyclization into a gemaminali. The acrolein-guanine adduct induces mutations during DNA copying and thus causes cancers in a manner similar to PAHs. However, acrolein is 1000 times more abundant than PAHs in cigarette smoke and is able to react as is, without metabolic activation. Acrolein has been shown to be a mutagen va kanserogen in human cells. The carcinogenicity of acrolein has been difficult to study by hayvonlar tajribasi, because it has such a toxicity that it tends to kill the animals before they develop cancer.[185] Generally, compounds able to react by conjugate addition kabi elektrofillar (deb nomlangan Mayklni qabul qiluvchilar keyin Mayklning reaktsiyasi ) are toxic and carcinogenic, because they can permanently alkylate DNA, similarly to xantal gazi yoki aflatoksin. Acrolein is only one of them present in cigarette smoke; masalan, krotonaldegid has been found in cigarette smoke.[189] Michael acceptors also contribute to the chronic inflammation present in tobacco disease.[79]
- Nitrosaminlar are a group of carcinogenic compounds found in cigarette smoke but not in uncured tobacco leaves. Nitrosamines form on flue-cured tobacco leaves during the curing process through a kimyoviy reaktsiya between nicotine and other compounds contained in the uncured leaf and various oxides of nitrogen found in all combustion gasses. Switching to Indirect fire curing has been shown to reduce nitrosamine levels to less than 0.1 parts per million.[190][191]
Sidestream tobacco smoke, or exhaled mainstream smoke, is particularly harmful. Because exhaled smoke exists at lower temperatures than inhaled smoke, chemical compounds undergo changes which can cause them to become more dangerous. As well, smoke undergoes changes as it ages, which causes the transformation of the compound NO into the more toxic NO2. Further, volatilization causes smoke particles to become smaller, and thus more easily embedded deep into the lung of anyone who later breathes the air.[192]
Radioactive carcinogens
In addition to chemical, nonradioactive carcinogens, tobacco and tobacco smoke contain small amounts of qo'rg'oshin-210 (210Pb) and polonyum-210 (210Po) both of which are radioactive carcinogens. The presence of polonium-210 in mainstream cigarette smoke has been experimentally measured at levels of 0.0263–0.036 pCi (0.97–1.33 mBq ),[193][194] which is equivalent to about 0.1 pCi per milligram of smoke (4 mBq/mg); or about 0.81 pCi of lead-210 per gram of dry condensed smoke (30 Bq/kg).
Tadqiqot tomonidan NCAR radiochemist Ed Martell suggested that radioactive compounds in cigarette smoke are deposited in "hot spots" where bronxial naychalar branch, that tar from cigarette smoke is resistant to dissolving in lung fluid and that radioactive compounds have a great deal of time to undergo radioaktiv parchalanish before being cleared by natural processes. Indoors, these radioactive compounds can linger in secondhand smoke, and greater exposure would occur when these radioactive compounds are inhaled during normal breathing, which is deeper and longer than when inhaling cigarettes. Damage to the protective epiteliy tissue from smoking only increases the prolonged retention of insoluble polonium-210 compounds produced from burning tobacco. Martell estimated that a carcinogenic radiation dose of 80–100 rads is delivered to the lung tissue of most smokers who die of lung cancer.[195][196][197]
Smoking an average of 1.5 packs per day gives a radiation dose of 60-160 mSv /year,[198][199] compared with living near a nuclear power station (0.0001 mSv/year)[200][201] or the 3.0 mSv/year average dose for Americans.[201][202]Some of the mineral apatite in Florida used to produce phosphate for U.S.A. tobacco crops contains uranium, radium, lead-210 and polonium-210 and radon.[203][204] The radioactive smoke from tobacco fertilized this way is deposited in lungs and releases radiation even if a smoker quits the habit. The combination of carcinogenic tar and radiation in a sensitive organ such as lungs increases the risk of cancer.[iqtibos kerak ]
In contrast, a 1999 review of tobacco smoke carcinogens published in the Milliy saraton instituti jurnali states that "levels of polonium-210 in tobacco smoke are not believed to be great enough to significantly impact lung cancer in smokers."[205] In 2011 Hecht has also stated that the "levels of 210Po in cigarette smoke are probably too low to be involved in lung cancer induction ..."[206]
Oxidation and inflammation
Erkin radikallar va pro-oxidants in cigarettes damage blood vessels and oxidize LDL cholesterol.[207] Only oxidized LDL cholesterol is taken-up by makrofaglar bo'lib, ular ko'pikli hujayralar, olib boradi aterosklerotik plakatlar.[207] Cigarette smoke increases proinflamatuar sitokinlar in the bloodstream, causing ateroskleroz.[207] The pro-oxidative state also leads to endotelial disfunktsiya,[207] which is another important cause of atherosclerosis.[208]
Nikotin

Nikotin, which is contained in cigarettes and other smoked tobacco products, is a stimulyator and is one of the main factors leading to continued tobacco smoking. Nikotin is a highly addictive psychoactive chemical. When tobacco is smoked, most of the nicotine is pyrolyzed; a dose sufficient to cause mild somatic dependency and mild to strong psychological dependency remains. The amount of nicotine absorbed by the body from smoking depends on many factors, including the type of tobacco, whether the smoke is inhaled, and whether a filter is used. There is also a formation of harmane (a MAO inhibitor ) dan asetaldegid in cigarette smoke, which seems to play an important role in nicotine addiction[209] probably by facilitating dopamine release in the nucleus accumbens in response to nicotine stimuli. According to studies by Henningfield and Benowitz, nicotine is more addictive than nasha, kofein, etanol, kokain va geroin when considering both somatic and psychological dependence. However, due to the stronger withdrawal effects of etanol, kokain va geroin, nicotine may have a lower potential for somatic dependence than these substances.[210][211] About half of Canadians who currently smoke have tried to quit.[212] McGill universiteti health professor Jennifer O'Loughlin stated that nicotine addiction can occur as soon as five months after the start of smoking.[213]
Ingesting a compound by smoking is one of the most rapid and efficient methods of introducing it into the bloodstream, second only to injection, which allows for the rapid feedback which supports the smokers' ability to titrlash their dosage. On average it takes about ten seconds for the substance to reach the brain. As a result of the efficiency of this delivery system, many smokers feel as though they are unable to cease. Of those who attempt cessation and last three months without succumbing to nicotine, most are able to remain smoke-free for the rest of their lives.[214][tekshirib bo'lmadi ] There exists a possibility of depression in some who attempt cessation, as with other psychoactive substances. Depression is also common in teenage smokers; teens who smoke are four times as likely to develop depressive symptoms as their nonsmoking peers.[215]
Although nicotine does play a role in acute episodes of some diseases (including qon tomir, iktidarsizlik va yurak kasalligi ) by its stimulation of adrenalin release, which raises blood pressure,[91] heart and respiration rate, and erkin yog 'kislotalari, the most serious longer term effects are more the result of the products of the smouldering combustion process. This has led to the development of various nicotine delivery systems, such as the nikotin patch yoki nikotin saqichi, that can satisfy the addictive craving by delivering nicotine without the harmful combustion by-products. This can help the heavily dependent smoker to quit gradually, while discontinuing further damage to health.[iqtibos kerak ]
Recent evidence has shown that smoking tobacco increases the release of dopamin in the brain, specifically in the mesolimbic pathway, the same neuro-reward circuit activated by drugs of abuse such as geroin va kokain. This suggests nicotine use has a pleasurable effect that triggers positive reinforcement.[216] One study found that smokers exhibit better reaction-time and memory performance compared to non-smokers, which is consistent with increased activation of dopamine receptors.[217] Neurologically, rodent studies have found that nicotine self-administration causes lowering of reward thresholds—a finding opposite that of most other drugs of abuse (e.g. cocaine and heroin).
The carcinogenity of tobacco smoke is not explained by nikotin per se, which is not carcinogenic or mutagenic, although it is a metabolic precursor for several compounds which are.[iqtibos kerak ] In addition, it inhibits apoptoz, therefore accelerating existing cancers.[218] Shuningdek, NNK, a nicotine derivative converted from nicotine, can be carcinogenic.
Shuni ta'kidlash joizki nikotin, although frequently implicated in producing tamaki addiction, is not significantly addictive when administered alone.[219][birlamchi bo'lmagan manba kerak ] The addictive potential manifests itself after co-administration of an MAOI, which specifically causes sezgirlik ning harakatlantiruvchi response in rats, a measure of addictive potential.[220]
Forms of exposure
Ikkinchi qo'l tutun

Second-hand smoke is a mixture of smoke from the burning end of a cigarette, pipe or cigar, and the smoke exhaled from the lungs of smokers. It is involuntarily inhaled, lingers in the air hours after cigarettes have been extinguished, and may cause a wide range of adverse health effects, including cancer, nafas olish yo'llari infektsiyalari va Astma.[221] Non-smokers who are exposed to second-hand smoke at home or work are thought, due to a wide variety of statistical studies, to increase their heart disease risk by 25–30% and their lung cancer risk by 20–30%. Second-hand smoke has been estimated to cause 38,000 deaths per year, of which 3,400 are deaths from lung cancer in non-smokers.[222]
The current US Surgeon General's Report concludes that there is no established risk-free level of exposure to ikkinchi qo'l tutun. Short exposures to second-hand smoke are believed to cause blood platelets to become stickier, damage the lining of qon tomirlari, decrease coronary flow velocity reserves, and reduce heart rate variability, potentially increasing the risk of yurak xuruji.[iqtibos kerak ] New research indicates that private research conducted by cigarette company Filipp Morris in the 1980s showed that second-hand smoke was toxic, yet the company suppressed the finding during the next two decades.[221]
Tamaki chaynash
Tamaki chaynash has been known to cause cancer, particularly of the og'iz va tomoq.[223] Ga ko'ra Xalqaro saraton tadqiqotlari agentligi, "Some health scientists have suggested that smokeless tobacco should be used in smoking cessation programmes and have made implicit or explicit claims that its use would partly reduce the exposure of smokers to carcinogens and the risk for cancer. These claims, however, are not supported by the available evidence."[223] Og'zaki va tupurilgan tamaki xavfini oshiradi leykoplakiya, uchun kashshof og'iz saratoni.[224]
Sigaretalar
Like other forms of smoking, puro smoking poses a significant health risk depending on dosage: risks are greater for those who inhale more when they smoke, smoke more cigars, or smoke them longer.[89] The risk of dying from any cause is significantly greater for cigar smokers, with the risk particularly higher for smokers less than 65 years old, and with risk for moderate and deep inhalers reaching levels similar to cigarette smokers.[225] The increased risk for those smoking 1–2 cigars per day is too small to be statistically significant,[226] and the health risks of the 3/4 of cigar smokers who smoke less than daily are not known[227] and are hard to measure. Although it has been claimed that people who smoke few cigars have no increased risk, a more accurate statement is that their risks are proportionate to their exposure.[88] Health risks are similar to sigaret smoking in nikotin giyohvandlik, periodontal health, tooth loss, and many types of cancer, including cancers of the og'iz, throat, and qizilo'ngach. Cigar smoking also can cause cancers of the o'pka va gırtlak, where the increased risk is less than that of cigarettes. Many of these cancers have extremely low cure rates. Cigar smoking also increases the risk of lung and heart diseases such as surunkali obstruktiv o'pka kasalligi.[89]
Narxlar
A common belief among users is that the smoke of a nargile (waterpipe, narghile) is significantly less dangerous than that from cigarettes.[228] The water moisture induced by the hookah makes the smoke less irritating and may give a false sense of security and reduce concerns about true health effects.[229] Doctors at institutions including the Mayo klinikasi have stated that use of hookah can be as detrimental to a person's health as smoking cigarettes,[230][231] and a study by the World Health Organization also confirmed these findings.[232]
Each hookah session typically lasts more than 40 minutes, and consists of 50 to 200 inhalations that each range from 0.15 to 0.50 liters of smoke.[233][234] In an hour-long smoking session of hookah, users consume about 100 to 200 times the smoke of a single cigarette;[233][235] Da o'rganish Periodontologiya jurnali found that water pipe smokers were marginally more likely than regular smokers to show signs of gum disease, showing rates 5-fold higher than non-smokers rather than the 3.8-fold risk that regular smokers show.[236] Ga binoan USA Today, people who smoked water pipes had five times the risk of lung cancer of non-smokers.[237]
A study on hookah smoking and cancer in Pokiston was published in 2008. Its objective was "to find serum CEA levels in ever/exclusive hookah smokers, i.e. those who smoked only hookah (no cigarettes, bidis, etc.), prepared between 1 and 4 times a day with a quantity of up to 120 g of a tobacco-molasses mixture each (i.e. the tobacco weight equivalent of up to 60 cigarettes of 1 g each) and consumed in 1 to 8 sessions". Carcinoembryonic antigen (CEA) is a marker found in several forms of cancer. Levels in exclusive hookah smokers were lower compared to cigarette smokers although the difference was not as statistically significant as that between a hookah smoker and a non-smoker. Also, the study concluded that heavy hookah smoking (2–4 daily preparations; 3–8 sessions a day; >2 hrs to ≤ 6 hours) substantially raises CEA levels.[238] Hookah smokers were nearly 6 times more likely to develop lung cancer as compared to healthy non-smokers in Kashmir (India).[239]
Tamakiga botirish
Dipping tobacco, commonly referred to as snuff, is also put in the mouth, but it is a flavored powder. it is placed between the cheek and gum. Dipping tobacco does not need to be chewed for the nicotine to be absorbed. First-time users of these products often become nauseated and dizzy. Long-term effects include bad breath, yellowed teeth, and an increased risk of oral cancer.[iqtibos kerak ]
Users of dipping tobacco are believed to face less risk of some cancers than are smokers, but are still at greater risk than people who do not use any tobacco products.[240] They also have an equal risk of other health problems directly linked to nicotine, such as increased rate of ateroskleroz.[iqtibos kerak ]
Oldini olish
Education and counselling by physicians of children and adolescents have been found to be effective in decreasing tobacco use.[241]

Average price of a pack of 20 cigarettes, measured in international dollars in 2014.[242]

Taxes as a share of cigarette price, 2014[243]

Types of bans on tobacco advertising, 2014[244]

Support to help quit tobacco use, 2014[245]
Foydalanish


Though tobacco may be consumed by either smoking or other smokeless methods such as chewing, the Jahon Sog'liqni saqlash tashkiloti (WHO) only collects data on smoked tobacco.[1] Smoking has therefore been studied more extensively than any other form of tobacco consumption.[2]
In 2000, smoking was practiced by 1.22 billion people, predicted to rise to 1.45 billion people in 2010 and 1.5 to 1.9 billion by 2025. If prevalence had decreased by 2% a year since 2000 this figure would have been 1.3 billion in 2010 and 2025.[246] Despite dropping by 0.4 percent from 2009 to 2010, the United States still reports an average of 17.9 percent usage.[52]
As of 2002, about twenty percent of young teens (13–15) smoked worldwide, with 80,000 to 100,000 children taking up the addiction every day, roughly half of whom live in Asia. Half of those who begin smoking in o'spirin years are projected to go on to smoke for 15 to 20 years.[247]
Teens are more likely to use e-cigarettes than cigarettes. About 31% of teenagers who use e-cigs started smoking within 6 months, compared to 8% of non-smokers. Manufacturers don't have to report what is in e-cigs, and most teens either say its just flavoring, or don't know.[248][249]
The JSSV states that "Much of the disease burden and premature mortality attributable to tobacco use disproportionately affect the poor". Of the 1.22 billion smokers, 1 billion live in developing or transitional nations. Rates of smoking have leveled off or declined in the rivojlangan dunyo.[250] In rivojlanayotgan dunyo, however, tobacco consumption was rising by 3.4% per year as of 2002.[247]
The WHO in 2004 projected 58.8 million deaths to occur globally,[251]:8 from which 5.4 million are tobacco-attributed,[251]:23 and 4.9 million as of 2007.[252] As of 2002, 70% of the deaths are in developing countries.[252]
The shift in prevalence of tobacco smoking to a younger demographic, mainly in the developing world, can be attributed to several factors. The tobacco industry spends up to $12.5 billion annually on advertising, which is increasingly geared towards adolescents in the developing world because they are a very vulnerable audience for the marketing campaigns. Adolescents have more difficulty understanding the long-term health risks that are associated with smoking and are also more easily influenced by "images of romance, success, sophistication, popularity, and adventure which advertising suggests they could achieve through the consumption of cigarettes". This shift in marketing towards adolescents and even children in the tobacco industry is debilitating to organizations' and countries' efforts to improve child health and mortality in the developing world. It reverses or halts the effects of the work that has been done to improve health care in these countries, and although smoking is deemed as a "voluntary" health risk, the marketing of tobacco towards very impressionable adolescents in the developing world makes it less of a voluntary action and more of an inevitable shift.[4]
Many government regulations have been passed to protect citizens from harm caused by public environmental tobacco smoke. The "Pro-Children Act of 2001" prohibits smoking within any facility that provides health care, day care, library services, or elementary and secondary education to children in the US.[253]On May 23, 2011, Nyu-York shahri enforced a smoking ban for all parks, beaches, and pedestrian malls in an attempt to eliminate threats posed to civilians by environmental tobacco smoke.[254]
Shuningdek qarang
- E. Cuyler Hammond
- Sigaret tutuni kanserogenlari ro'yxati
- Elektron sigaretlarning xavfsizligi
- Elektron sigaretalarning salbiy ta'siri
Adabiyotlar
- ^ a b "Prevalence of current tobacco use among adults aged=15 years (percentage)". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasi 2008-12-11. Olingan 2009-01-02.
- ^ a b "Mayo report on addressing the worldwide tobacco epidemic through effective, evidence-based treatment". Jahon Sog'liqni saqlash tashkiloti. p. 2018-04-02 121 2. Olingan 2009-01-02.
- ^ a b v d e f "Tobacco Fact sheet N°339". 2014 yil may. Olingan 13 may 2015.
- ^ a b Nichter M, Cartwright E (1991). "Saving the Children for the Tobacco Industry". Har chorakda tibbiy antropologiya. 5 (3): 236–56. doi:10.1525/maq.1991.5.3.02a00040. JSTOR 648675.
- ^ a b Jahon sog'liqni saqlash tashkiloti (2008). Jahon sog'liqni saqlash tashkilotining 2008 yilgi global tamaki epidemiyasi to'g'risida hisoboti: MPOWER to'plami (PDF). Jeneva: Jahon sog'liqni saqlash tashkiloti. p. 8. ISBN 978-92-4-159628-2.
- ^ "O'limning eng yaxshi 10 sababi". Olingan 13 may 2015.
- ^ "Nicotine: A Powerful Addiction Arxivlandi 2009-05-01 da Orqaga qaytish mashinasi." Centers for Disease Control and Prevention.
- ^ "These Two Industries Kill More People Than They Employ". IFLScience. Olingan 2019-03-09.
- ^ Jha P, Peto R (January 2014). "Global effects of smoking, of quitting, and of taxing tobacco". Nyu-England tibbiyot jurnali. 370 (1): 60–8. doi:10.1056/nejmra1308383. PMID 24382066. S2CID 4299113.
- ^ Vainio H (June 1987). "Is passive smoking increasing cancer risk?". Skandinaviya ish, atrof-muhit va sog'liqni saqlash jurnali. 13 (3): 193–6. doi:10.5271/sjweh.2066. PMID 3303311.
- ^ "The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General" (PDF). Atlanta, U.S., page 93: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2006 yil. Olingan 2009-02-15.CS1 tarmog'i: joylashuvi (havola)
- ^ a b Peate I (2005). "Chekishning erkaklarning reproduktiv salomatligiga ta'siri". Britaniya hamshiralik jurnali. 14 (7): 362–6. doi:10.12968 / bjon.2005.14.7.17939. PMID 15924009.
- ^ Korenman SG (2004). "Erektil disfunktsiya epidemiologiyasi". Endokrin. 23 (2–3): 87–91. doi:10.1385 / ENDO: 23: 2-3: 087. PMID 15146084. S2CID 29133230.
- ^ a b v d e f g h men j k l m Doll R (June 1998). "Uncovering the effects of smoking: historical perspective" (PDF). Tibbiy tadqiqotlarda statistik usullar. 7 (2): 87–117. doi:10.1177/096228029800700202. PMID 9654637. S2CID 154707. Arxivlandi asl nusxasi (PDF) 2018-10-01 kunlari. Olingan 2018-09-30.
- ^ a b Alston LJ, Dupré R, Nonnenmacher T (2002). "Social reformers and regulation: the prohibition of cigarettes in the United States and Canada". Iqtisodiy tarixdagi tadqiqotlar. 39 (4): 425–445. doi:10.1016/S0014-4983(02)00005-0.
- ^ James R (2009-06-15). "A Brief History Of Cigarette Advertising". TIME. Olingan 2012-03-25.
- ^ a b v d Haustein K (2004). "Fritz Lickint (1898–1960) – Ein Leben als Aufklärer über die Gefahren des Tabaks". Suchtmed (nemis tilida). 6 (3): 249–255. Arxivlandi asl nusxasi 2014 yil 5-noyabrda.
- ^ a b v d Proktor RN (2001 yil fevral). "Sharh: Shairer va Shonigerning unutilgan tamaki epidemiologiyasi va natsistlarning irqiy poklik izlashi". Xalqaro epidemiologiya jurnali. 30 (1): 31–4. doi:10.1093 / ije / 30.1.31. PMID 11171846.
- ^ Djian, Jan-Mishel (2007 yil 24-may). Timbuktu qo'lyozmalari: Afrikaning yozma tarixi ochildi Arxivlandi 11 November 2009 at the Orqaga qaytish mashinasi. Unesco, ID 37896.
- ^ Lincecum, Gideon. "Nicotiana tabacum". Giden Lincecum Herbarium. Texas universiteti. Olingan 9 dekabr 2012.
- ^ Adler IA (1980). "Classics in oncology. Primary malignant growths of the lung. Isaac A. Adler, A.M., M.D". Ca. 30 (5): 295–301. doi:10.3322/canjclin.30.5.295. PMID 6773624. S2CID 6967224.
- ^ Irving Fisher (1924). "Does tobacco injure the human body?". Readers Digest. Arxivlandi asl nusxasi on 2014-04-18.
- ^ Witschi H (2001 yil noyabr). "O'pka saratonining qisqa tarixi". Toksikologik fanlar. 64 (1): 4–6. doi:10.1093 / toxsci / 64.1.4. PMID 11606795.
- ^ Adler I (1912). Primary malignant growths of the lungs and bronchi: a pathological and clinical study. Nyu-York: Longmans, Yashil. OCLC 14783544.[sahifa kerak ], keltirilgan Spiro SG, Silvestri GA (sentyabr 2005). "One hundred years of lung cancer". Amerika nafas olish va tanqidiy tibbiyot jurnali. 172 (5): 523–9. doi:10.1164 / rccm.200504-531OE. PMID 15961694. S2CID 21653414.
- ^ Milliy saraton instituti. "20 Year Lag Time Between Smoking and Lung Cancer". Arxivlandi asl nusxasi 2003 yil 17 fevralda.
- ^ a b v Oreskes N Conway EM (2010). Shubha savdogarlari: qanday qilib bir necha olimlar tamaki tutunidan global isishgacha bo'lgan masalalarda haqiqatni yashirganlar. San Francisco, CA: Bloomsbury Press. p.15. ISBN 978-1-59691-610-4.
- ^ a b v Michaels, David (2008). Doubt is their product: how industry's assault on science threatens your health. Oksford [Oksfordshir]: Oksford universiteti matbuoti. pp.4–5. ISBN 978-0-19-530067-3.
- ^ a b Doll R, Hill AB (September 1950). "Smoking and carcinoma of the lung; preliminary report". British Medical Journal. 2 (4682): 739–48. doi:10.1136 / bmj.2.4682.739. PMC 2038856. PMID 14772469.
- ^ a b v d e f Doll R, Peto R, Boreham J, Sutherland I (iyun 2004). "Mortality in relation to smoking: 50 years' observations on male British doctors". BMJ. 328 (7455): 1519. doi:10.1136/bmj.38142.554479.AE. PMC 437139. PMID 15213107.
- ^ Doll R, Hill AB (June 2004). "The mortality of doctors in relation to their smoking habits: a preliminary report. 1954". BMJ. 328 (7455): 1529–33, discussion 1533. doi:10.1136 / bmj.328.7455.1529. PMC 437141. PMID 15217868.
- ^ a b Brandt AM (2007). The cigarette century: the rise, fall and deadly persistence of the product that defined America. Nyu-York: Perseus Books guruhining a'zosi bo'lgan asosiy kitoblar. ISBN 978-0-465-07047-3.
- ^ Pell JP, Haw S, Cobbe S, Newby DE, Pell AC, Fischbacher C, McConnachie A, Pringle S, Murdoch D, Dunn F, Oldroyd K, Macintyre P, O'Rourke B, Borland W (July 2008). "Smoke-free legislation and hospitalizations for acute coronary syndrome" (PDF). Nyu-England tibbiyot jurnali. 359 (5): 482–91. doi:10.1056 / NEJMsa0706740. hdl:1893/16659. PMID 18669427.
- ^ Nutt D, King LA, Saulsbury V, Blakemore C (2007 yil mart). "Iste'mol qilinadigan giyohvandlik vositalarining zararini baholash uchun oqilona o'lchovni ishlab chiqish". Lanset. 369 (9566): 1047–53. doi:10.1016 / s0140-6736 (07) 60464-4. PMID 17382831. S2CID 5903121.
- ^ ASPA. "Health Effects of Tobacco". Arxivlandi asl nusxasi 2014-09-20. Olingan 8 sentyabr 2014.
- ^ "Life Expectancy at Age 30: Nonsmoking Versus Smoking Men". Onlaynda tamaki hujjatlari. Arxivlandi asl nusxasi 2012-04-19. Olingan 2012-05-06.
- ^ Ferrucci L, Izmirlian G, Leveille S, Phillips CL, Corti MC, Brock DB, Guralnik JM (April 1999). "Smoking, physical activity, and active life expectancy". Amerika Epidemiologiya jurnali. 149 (7): 645–53. doi:10.1093/oxfordjournals.aje.a009865. PMID 10192312.
- ^ Doll R, Peto R, Wheatley K, Gray R, Sutherland I (October 1994). "Mortality in relation to smoking: 40 years' observations on male British doctors". BMJ. 309 (6959): 901–11. doi:10.1136/bmj.309.6959.901. PMC 2541142. PMID 7755693.
- ^ Villeneuve PJ, Mao Y (1994). "Lifetime probability of developing lung cancer, by smoking status, Canada". Kanada jamoat salomatligi jurnali. 85 (6): 385–8. PMID 7895211.
- ^ Kenneth Johnson (Jan 24, 2018). "Just one cigarette a day seriously elevates cardiovascular risk". British Medical Journal. 360: k167. doi:10.1136 / bmj.k167. PMID 29367307. S2CID 46825572.
- ^ "Kuniga atigi bitta sigareta yurakka jiddiy muammolarni keltirib chiqarishi mumkin". Yangi olim. 2020 yil 3-fevral.
- ^ "Ishdan bo'shatishning afzalliklari - Amerika o'pka uyushmasi". Chekishni to'xtating. Amerika o'pka assotsiatsiyasi. Olingan 2012-05-06.
- ^ "Engil sigaretalar va saraton xavfi". Milliy saraton instituti. 2005-08-18. Olingan 8 sentyabr 2014.
- ^ Rizzuto D, Fratiglioni L (2014). "O'lim va omon qolish bilan bog'liq turmush tarzi omillari: mini-sharh". Gerontologiya. 60 (4): 327–35. doi:10.1159/000356771. PMID 24557026.
- ^ Samet JM (2013 yil may). "Tamaki chekish: dunyo bo'ylab oldini olish mumkin bo'lgan kasallikning asosiy sababi". Ko'krak qafasi xirurgiyasi klinikalari. 23 (2): 103–12. doi:10.1016 / j.thorsurg.2013.01.009. PMID 23566962.
- ^ Kasalliklarni nazorat qilish va oldini olish markazlari (CDC) (2002 yil aprel). "Chekish bilan bog'liq yillik o'lim, yo'qotilgan potentsial hayot yillari va iqtisodiy xarajatlar - Amerika Qo'shma Shtatlari, 1995-1999". MMWR. Kasallik va o'lim bo'yicha haftalik hisobot. 51 (14): 300–3. PMID 12002168.
- ^ Streppel MT, Boshuizen HC, Ocké MC, Kok FJ, Kromhout D (2007 yil aprel). "Uzoq muddatli sigareta, sigara va trubadan chekishga nisbatan o'lim va umr ko'rish davomiyligi: Zutphen Study". Tamaki nazorati. 16 (2): 107–13. doi:10.1136 / tc.2006.017715. PMC 2598467. PMID 17400948.
- ^ "Arxivlangan nusxa" (PDF). Arxivlandi asl nusxasi (PDF) 2009-12-29 kunlari. Olingan 2009-11-13.CS1 maint: nom sifatida arxivlangan nusxa (havola)
- ^ "Sog'liqni saqlash | Sigaretlarning hayoti 11 daqiqaga qisqardi'". BBC yangiliklari. 1999-12-31. Olingan 2012-03-25.
- ^ Shou, M. (2000). "Tutun vaqti? Bir sigaret hayotingizni 11 daqiqaga qisqartiradi". BMJ. 320 (7226): 53. doi:10.1136 / bmj.320.7226.53. PMC 1117323. PMID 10617536.
- ^ Mamun AA, Peeters A, Barendregt J, Willekens F, Nusselder V, Bonneux L (mart 2004). "Chekish yurak-qon tomir kasalliklari bo'lgan va bo'lmagan hayot davomiyligini pasaytiradi: Framingham Heart Study-ning hayotiy tahlili". European Heart Journal. 25 (5): 409–15. doi:10.1016 / j.ehj.2003.12.015. PMID 15033253.
- ^ Thun MJ, Day-Lally, CA, Calle EE, Flandriya WD, Heath CW (sentyabr 1995). "Sigaret chekuvchilar orasida haddan tashqari o'lim: 20 yillik intervaldagi o'zgarishlar". Amerika sog'liqni saqlash jurnali. 85 (9): 1223–30. doi:10.2105 / AJPH.85.9.1223. PMC 1615570. PMID 7661229.
- ^ a b "Amerika sog'liqni saqlash reytingi - 2011" (PDF). Birlashgan sog'liqni saqlash jamg'armasi. 2011 yil dekabr. P. 12.
- ^ Kasalliklarni nazorat qilish va oldini olish markazlari (CDC) (2008 yil noyabr). "Chekish bilan bog'liq o'lim, yo'qotilgan potentsial hayot yillari va mahsuldorlikning yo'qolishi - Amerika Qo'shma Shtatlari, 2000-2004". MMWR. Kasallik va o'lim bo'yicha haftalik hisobot. 57 (45): 1226–8. PMID 19008791.
- ^ Never Say Die, ABC News maxsus Piter Jennings tomonidan 27.06.1996
- ^ "XXI asr tamaki qurbonlaridan bir milliardni ko'rishi mumkin" (PDF). Tamaki yangiliklari. 3 (12): 1. 2007. Arxivlangan asl nusxasi (PDF) 2012-04-26. Olingan 2012-05-06.
- ^ Carter BD, Abnet CC, Feskanich D, Freedman ND, Hartge P, Lewis CE, Ockene JK, Prentice RL, Speizer FE, Thun MJ, Jacobs EJ (2015 yil fevral). "Chekish va o'lim - belgilangan sabablardan tashqari". Nyu-England tibbiyot jurnali. 372 (7): 631–40. doi:10.1056 / NEJMsa1407211. PMID 25671255. S2CID 34821377.
- ^ a b Proktor, Robert N (2012-02-16). "Chekish-o'pka saratoniga aloqador kashfiyot tarixi: daliliy an'analar, korporativ inkor, global to'lov: 1-jadval".. Tamaki nazorati. 21 (2): 87–91. doi:10.1136 / tamaki nazorati-2011-050338. ISSN 0964-4563. PMID 22345227.
- ^ Koen, Bernard L. (1991 yil sentyabr). "Kengaytirilgan va yangilangan xatarlar katalogi". Sog'liqni saqlash fizikasi. 61 (3): 317–335. doi:10.1097/00004032-199109000-00002. ISSN 0017-9078. PMID 1880022.
- ^ "Chekishdan o'limlarning ulushi". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ "Chekishdan o'lim darajasi". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ "Tamaki bilan bog'liq saraton kasalligidan o'lim ulushi". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ "O'pka saratoni va chekish" (PDF). Ma'lumotlar sahifasi. www.LegacyForHealth.org. 2010-11-23. Arxivlandi asl nusxasi (PDF) 2013-03-15. Olingan 2012-05-06.
- ^ Lipvort L, Tarone RE, McLaughlin JK (2006 yil dekabr). "Buyrak hujayralari karsinomasining epidemiologiyasi". Urologiya jurnali. 176 (6 Pt 1): 2353-8. doi:10.1016 / j.juro.2006.07.130. PMID 17085101.
- ^ "Tomoq saratoni xavfi va sabablari". Cancer Research UK. Olingan 21 iyun 2015.
- ^ "Bosh va bo'yin saratoni: xavf omillari va oldini olish". ASCO. 2012-06-26. Olingan 21 iyun 2015.
- ^ Boffetta P (sentyabr, 2008 yil). "Tamaki chekish va qovuq saratoni xavfi". Skandinaviya urologiya va nefrologiya jurnali. Qo'shimcha. 42 (218): 45–54. doi:10.1080/03008880802283664. PMID 18815916. S2CID 39577281.
- ^ "Qizilo'ngach saratoni". Amerika saraton kasalligi jamiyati. 2011-08-11. Olingan 2012-05-06.
- ^ Iodice S, Gandini S, Maisonneuve P, Lowenfels AB (iyul 2008). "Tamaki va oshqozon osti bezi saratoni xavfi: qayta ko'rib chiqish va meta-tahlil". Langenbekning jarrohlik arxivi. 393 (4): 535–45. doi:10.1007 / s00423-007-0266-2. PMID 18193270. S2CID 23516238.
- ^ a b Kuper H, Boffetta P, Adami XO (sentyabr 2002). "Tamaki iste'mol qilish va saraton kasalligining sababi: o'sma turi bo'yicha assotsiatsiya". Ichki kasalliklar jurnali. 252 (3): 206–24. doi:10.1046 / j.1365-2796.2002.01022.x. PMID 12270001. S2CID 6132726.
- ^ Vineis P, Alavanja M, Buffler P, Fontam E, Francheski S, Gao YT, Gupta Kompyuter, Xakshu A, Matos E, Samet J, Sitas F, Smit J, Stayner L, Straif K, Thun MJ, Vichmann HE, Vu AH , Zaridze D, Peto R, Doll R (2004 yil yanvar). "Tamaki va saraton: so'nggi epidemiologik dalillar". Milliy saraton instituti jurnali. 96 (2): 99–106. doi:10.1093 / jnci / djh014. PMID 14734699.
- ^ Sasco AJ, Secretan MB, Straif K (2004 yil avgust). "Tamaki chekish va saraton kasalligi: so'nggi epidemiologik dalillarni qisqacha ko'rib chiqish". O'pka saratoni. 45 Qo'shimcha 2: S3-9. doi:10.1016 / j.lungcan.2004.07.998. PMID 15552776.
- ^ "Ko'krak bezi saratoniga olib keladigan xavf omillari qanday?". Amerika saraton kasalligi jamiyati. Olingan 31 may 2015.
- ^ Pesch, B., Kendzia, B., Gustavsson, P., Jokel, K.-H., Johnen, G., Pohlabeln, H.,… Brüning, T. (2012). Sigareta chekish va o'pka saratoni - asosiy gistologik turlar uchun nisbiy xavf tahminlari, vaziyatni nazorat qilish ishlarini birlashtirilgan tahlilidan. Xalqaro saraton jurnali. Journal International Du Cancer, 131 (5), 1210-1219.
- ^ Amerika Qo'shma Shtatlari Sog'liqni saqlash va odamlarga xizmat ko'rsatish vazirligi. Chekishning sog'liq uchun oqibatlarini kamaytirish: 25 yillik taraqqiyot. Bosh jarrohning hisoboti. Kimdan http://profiles.nlm.nih.gov/ps/retrieve/ResourceMetadata/NNBBXS Kirish: 2012 yil noyabr
- ^ Kalemkerian, G. P., Akerley, W., Bogner, P., Borghaei, H., Chow, L. Q., Downey, R. J.,… Hyuz, M. (2013). Kichik hujayrali o'pka saratoni: Onkologiya bo'yicha klinik qo'llanma. Milliy keng qamrovli saraton tarmog'i jurnali: JNCCN, 11 (1), 78-98.
- ^ Champaneria MC, Modlin IM, Kidd M, Eick GN (2006). "Fridrix Feyrter: tarqoq tizimdagi aniq aql". Neyroendokrinologiya. 83 (5–6): 394–404. doi:10.1159/000096050. PMID 17028417. S2CID 25627846.
- ^ Thun MJ, Xannan LM, Adams-Kempbell LL, Boffetta P, Buring JE, Feskanich D, Flandriya WD, Jee SH, Katanoda K, Kolonel LN, Li IM, Marugame T, Palmer JR, Riboli E, Sobue T, Avila-Tang E, Wilkens LR, Samet JM (sentyabr 2008). "Chekmaydigan odamlarda o'pka saratonining paydo bo'lishi: 13 kogortani tahlil qilish va 22 ta saratonni ro'yxatga olish bo'yicha tadqiqotlar". PLOS tibbiyoti. 5 (9): e185. doi:10.1371 / journal.pmed.0050185. PMC 2531137. PMID 18788891.
- ^ Devereux G (2006 yil may). "O'pka surunkali obstruktiv kasalligining ABC. Ta'rifi, epidemiologiyasi va xavf omillari". BMJ. 332 (7550): 1142–4. doi:10.1136 / bmj.332.7550.1142. PMC 1459603. PMID 16690673.
- ^ a b Facchinetti F, Amadei F, Geppetti P, Tarantini F, Di Serio C, Dragotto A, Gigli PM, Catinella S, Civelli M, Patacchini R (2007 yil noyabr). "Sigaret tutunidagi alfa, beta-to'yinmagan aldegidlar odam makrofaglaridan yallig'lanish vositachilarini chiqaradi". Amerika nafas olish hujayralari va molekulyar biologiya jurnali. 37 (5): 617–23. doi:10.1165 / rcmb.2007-0130OC. PMID 17600310.
- ^ Glantz SA, Parmley WW (1995 yil aprel). "Passiv chekish va yurak xastaligi. Mexanizmlar va xavf". JAMA. 273 (13): 1047–53. CiteSeerX 10.1.1.598.9772. doi:10.1001 / jama.1995.03520370089043. PMID 7897790.
- ^ Shoh RS, Koul JW (2010 yil iyul). "Chekish va qon tomir: qancha ko'p cheksangiz, shunchalik ko'p zarba berasiz". Kardiyovaskulyar terapiyani ekspertizasi. 8 (7): 917–32. doi:10.1586 / erc.10.56. PMC 2928253. PMID 20602553.
- ^ "Chekish yurak va qon tomirlariga qanday ta'sir qiladi?". NHLBI. Olingan 9 sentyabr 2015.
- ^ "Sog'liqni saqlash: yosh chekuvchilarning yurak xuruji xavfi". BBC. 2004-08-24. Olingan 2005-12-18.
- ^ Mähönen MS, McElduff P, Dobson AJ, Kuulasmaa KA, Evans AE (2004). "Jahon sog'liqni saqlash tashkilotining MONICA loyihasi populyatsiyasida hozirgi chekish va o'limga olib kelmaydigan miokard infarkti xavfi". Tamaki nazorati. 13 (3): 244–250. doi:10.1136 / tc.2003.003269. PMC 1747894. PMID 15333879.
- ^ Saha SP, Bhalla DK, Whayne TF, Gairola C (Kuz 2007). "Sigaretaning tutuni va sog'likka salbiy ta'siri: tadqiqot tendentsiyalari va kelajakdagi ehtiyojlarga umumiy nuqtai". Xalqaro angiologiya jurnali. 16 (3): 77–83. doi:10.1055 / s-0031-1278254. PMC 2733016. PMID 22477297.
- ^ "Sigaret tutuni yurak shaklini o'zgartiradi". InfoNIAC.com. Olingan 2009-01-10.
- ^ Joys JW (1990 yil may). "Buerger kasalligi (tromboangiit obliterans)". Shimoliy Amerikaning revmatik kasalliklar klinikalari. 16 (2): 463–70. PMID 2189162.
- ^ a b Berns DM (1998). "Sigaret chekish: fanga umumiy nuqtai va hozirgi holat" (PDF). Shopland DR-da Burns DM, Hoffmann D, Cummings KM, Amacher RH (tahr.). Sigaretalar: sog'liqqa ta'siri va tendentsiyalari. Chekish va tamakiga qarshi monografiya № 9. Milliy saraton instituti. 1-20 betlar.
- ^ a b v Symm B, Morgan MV, Blackshear Y, Tinsley S (iyul 2005). "Sigaret chekish: e'tiborsiz qoldirilgan sog'liq uchun tahdid" Birlamchi profilaktika jurnali. 26 (4): 363–75. doi:10.1007 / s10935-005-5389-z. PMID 15995804. S2CID 23999589.
- ^ a b Milliy sog'liqni saqlash institutlari (1998-04-10). "Sigara monografiyasi haqida ma'lumot: Sigaretalar: sog'liqqa ta'siri va tendentsiyalari". Arxivlandi asl nusxasi 2008-05-13 kunlari. Olingan 2008-01-04.
- ^ a b Narkeviç K, Kjeldsen SE, Hedner T (2005). "Chekish gipertoniya kasalligini keltirib chiqaradimi?". Qon bosimi. 14 (2): 69–71. doi:10.1080/08037050510034202. PMID 16036482. S2CID 40476025.
- ^ Yacoub R, Habib H, Lahdo A, Al Ali R, Varjabedian L, Atalla G, Kassis Akl N, Aldakheel S, Alahdab S, Albitar S (2010 yil noyabr). "Chekish va surunkali buyrak kasalligi o'rtasidagi assotsiatsiya: vaziyatni nazorat qilish". BMC sog'liqni saqlash. 10: 731. doi:10.1186/1471-2458-10-731. PMC 3004836. PMID 21108832.
- ^ Savicki PT, Didjurgeit U, Mühlhauzer I, Bender R, Heinemann L, Berger M (fevral 1994). "Chekish diabetik nefropatiyaning rivojlanishi bilan bog'liq". Qandli diabetga yordam. 17 (2): 126–31. doi:10.2337 / diacare.17.2.126. PMID 8137682. S2CID 22581830.
- ^ a b Kark JD, Lebiush M, Rannon L (1982 yil oktyabr). "Sigareta chekish yosh yigitlarda (h1n1) gripp epidemiyasi xavfi sifatida". Nyu-England tibbiyot jurnali. 307 (17): 1042–6. doi:10.1056 / NEJM198210213071702. PMID 7121513.
- ^ a b Finklea JF, Sandifer SH, Smit DD (Noyabr 1969). "Sigaret chekish va epidemik gripp". Amerika Epidemiologiya jurnali. 90 (5): 390–9. doi:10.1093 / oxfordjournals.aje.a121084. PMID 5356947.
- ^ Kark JD, Lebiush M (may 1981). "Harbiy xizmatga chaqirilgan ayollarda chekish va epidemiyaga qarshi grippga o'xshash kasallik: qisqacha so'rov". Amerika sog'liqni saqlash jurnali. 71 (5): 530–2. doi:10.2105 / AJPH.71.5.530. PMC 1619723. PMID 7212144.
- ^ Nicholson KG, Kent J, Hammersley V (1999 yil avgust). "1993-4 yil qish paytida Lestershirda yashovchi qariyalar orasida A grippi; sigaret chekish xavf omil sifatida va grippga qarshi emlash samaradorligi". Epidemiologiya va infektsiya. 123 (1): 103–8. doi:10.1017 / S095026889900271X. PMC 2810733. PMID 10487646.
- ^ Amerika saraton kasalligi jamiyati (2004). "Chekish, tamaki va sog'liqqa oid savollar". Milliy saraton institutining JNCI jurnali. 96 (11): 853–861. doi:10.1093 / jnci / djh144. PMID 15173269. Olingan 2008-01-04.
- ^ Henley SJ, Thun MJ, Chao A, Calle EE (iyun 2004). "Faqatgina trubka chekish va saraton va boshqa kasalliklardan o'lim o'rtasidagi bog'liqlik". Milliy saraton instituti jurnali. 96 (11): 853–61. doi:10.1093 / jnci / djh144. PMID 15173269.
- ^ Hayot fanlari bo'yicha komissiya. Ekologik tamaki tutuni: ta'sirni o'lchash va sog'liqqa ta'sirini baholash (1986). Olingan 2008-01-04.
- ^ Jonson GK, Slach NA (2001 yil aprel). "Tamakidan foydalanishning periodontal holatga ta'siri". Tish ta'limi jurnali. 65 (4): 313–21. doi:10.1002 / j.0022-0337.2001.65.4.tb03401.x. PMID 11336116.
- ^ Reibel J (2003). "Tamaki va og'iz kasalliklari. Tavsiyalar bilan dalillarni yangilang". Tibbiyot printsiplari va amaliyoti. 12 Qo'shimcha 1: 22-32. doi:10.1159/000069845. PMID 12707498.
- ^ Ness L, Rozekrans D, Velford JF (1977 yil yanvar). "Ingliz populyatsiyasida tishlarni tashqi bo'yashiga ta'sir qiluvchi omillarni epidemiologik o'rganish". Jamiyat stomatologiyasi va og'iz epidemiologiyasi. 5 (1): 55–60. doi:10.1111 / j.1600-0528.1977.tb01617.x. PMID 264419.
- ^ "Chekishni tashlashda sizga yordam beraman!". Arxivlandi asl nusxasi 2008-08-28 kunlari. Olingan 2008-01-04.
- ^ Züllich G, Damm KH, Braun V, Lisboa BP (may 1975). "Kalamushlarda [G-3H] digoksin oksidining safro bilan chiqarilgan metabolitlari bo'yicha tadqiqotlar". Archives Internationales de Pharmacodynamie et de Therapie. 215 (1): 160–7. PMID 1156044.
- ^ Ditrix T, Maserejian NN, Joshipura KJ, Krall EA, Garsiya RI (2007 yil aprel). "AQSh sog'liqni saqlash sohasidagi erkaklar orasida tamakidan foydalanish va tishni yo'qotish hollari". Tish tadqiqotlari jurnali. 86 (4): 373–7. doi:10.1177/154405910708600414. PMC 2582143. PMID 17384035.
- ^ Al-Bayaty FH, Vohid NA, Bulgiba AM (Fevral 2008). "Yamaning Sanadagi tanlangan populyatsiyasida chekuvchilar va chekuvchilarning tish o'limi". Periodontal tadqiqotlar jurnali. 43 (1): 9–13. doi:10.1111 / j.1600-0765.2007.00988.x. PMID 18230101.
- ^ "Leykoplakiya sabablari". Mayo klinikasi. Olingan 31 may 2015.
- ^ Devies PD, Yew WW, Ganguli D, Davidow AL, Reyxman LB, Dheda K, Rook GA (2006 yil aprel). "Chekish va sil kasalligi: epidemiologik assotsiatsiya va immunopatogenez". Tropik tibbiyot va gigiena qirollik jamiyatining operatsiyalari. 100 (4): 291–8. doi:10.1016 / j.trstmh.2005.06.034. PMID 16325875.
- ^ Jha P, Jacob B, Gajalakshmi V, Gupta PC, Dhingra N, Kumar R, Sinha DN, Dikshit RP, Parida DK, Kamadod R, Boreham J, Peto R (mart 2008). "Hindistonda chekish va o'lim holatlarini nazorat qiluvchi milliy vakolatxonasi". Nyu-England tibbiyot jurnali. 358 (11): 1137–47. doi:10.1056 / NEJMsa0707719. PMID 18272886. S2CID 92980.
- ^ Nuorti JP, Butler JC, Farley MM, Harrison LH, McGeer A, Kolczak MS, Breiman RF (mart 2000). "Sigaret chekish va invaziv pnevmokokk kasalligi. Faol bakteriyalar yadrosi kuzatuv guruhi". Nyu-England tibbiyot jurnali. 342 (10): 681–9. doi:10.1056 / NEJM200003093421002. PMID 10706897.
- ^ Arcavi L, Benowitz NL (2004 yil noyabr). "Sigaret chekish va yuqtirish". Ichki kasalliklar arxivi. 164 (20): 2206–16. doi:10.1001 / archinte.164.20.2206. PMID 15534156.
- ^ Goedert JJ, Vitale F, Lauria C, Serraino D, Tamburini M, Montella M, Messina A, Brown EE, Rezza G, Gafà L, Romano N (Noyabr 2002). "Klassik Kaposi sarkomasi uchun xavf omillari". Milliy saraton instituti jurnali. 94 (22): 1712–8. doi:10.1093 / jnci / 94.22.1712. PMID 12441327.
- ^ "MEDLINEplus: Chekish noyob saraton xavfini kamaytiradi". Olingan 8 sentyabr 2014.
- ^ a b "Tamaki haqida ma'lumotnoma". Arxivlandi asl nusxasi 2006-07-15 kunlari. Olingan 2006-07-15.
- ^ Kendirci M, Nowfar S, Hellstrom WJ (2005 yil yanvar). "Erektil funktsiyaga qon tomir xavf omillarining ta'siri". Bugungi dorilar. 41 (1): 65–74. doi:10.1358 / nuqta.2005.41.1.875779. PMID 15753970.
- ^ Dechanet C, Anahory T, Mathieu Daude JK, Quantin X, Reyftmann L, Hamamah S, Hedon B, Dechaud H (2011). "Sigaretaning ko'payishini reproduktsiyaga ta'siri". Inson ko'payishining yangilanishi. 17 (1): 76–95. doi:10.1093 / humupd / dmq033. PMID 20685716.
- ^ FERTILITY FAKT> Ayollar uchun xavf-xatar Arxivlandi 2007-09-22 da Orqaga qaytish mashinasi Amerika Reproduktiv Tibbiyot Jamiyati (ASRM) tomonidan. 2009 yil 4-yanvarda olingan
- ^ "protectyourfertility.com" (PDF). Arxivlandi asl nusxasi (PDF) 2015 yil 24 sentyabrda. Olingan 8 sentyabr 2014.
- ^ a b tug'ish bo'yicha xizmatlar: foydalanishga topshirish uchun yordam - 2009 yil iyun, Buyuk Britaniya Sog'liqni saqlash vazirligidan
- ^ Parrott AC (1999 yil oktyabr). "Sigaret chekish stressni keltirib chiqaradimi?". Amerikalik psixolog. 54 (10): 817–20. doi:10.1037 / 0003-066X.54.10.817. PMID 10540594.
- ^ Lagrue G, Lebargy F, Cormier A (2001). "Des récepteurs nikotiniques à la dépendance tabagique: istiqbollari thérapeutiques" [Nikotinik retseptorlardan chekishga qaramlikgacha: Terapevtik istiqbollar]. Alcoologie va Addictologie (frantsuz tilida). 23 (2 ta qo'shimcha): 39S-42S.
- ^ a b Parrott AC (1998 yil yanvar). "Nesbittning Paradoksi hal qilindi? Sigaret chekish paytida stress va qo'zg'alish modulyatsiyasi". Giyohvandlik. 93 (1): 27–39. CiteSeerX 10.1.1.465.2496. doi:10.1046 / j.1360-0443.1998.931274.x. PMID 9624709.
- ^ Xyuz JR (1992 yil oktyabr). "O'zini tashlab ketadigan narsalarda tamakidan voz kechish". Konsalting va klinik psixologiya jurnali. 60 (5): 689–97. doi:10.1037 / 0022-006X.60.5.689. PMID 1401384.
- ^ Koen S, Lixtenshteyn E (1990). "Sezilgan stress, chekishni tashlash va chekish qayt qilish". Sog'liqni saqlash psixologiyasi. 9 (4): 466–78. doi:10.1037/0278-6133.9.4.466. PMID 2373070.
- ^ Hamer M, Stamatakis E, Batti GD (avgust 2010). "Kattalardagi chekilgan chekish va ruhiy salomatlik ob'ektiv ravishda baholandi: Shotlandiya sog'liqni saqlash tadqiqotining tasavvurlari va istiqbolli dalillari". Umumiy psixiatriya arxivi. 67 (8): 850–5. doi:10.1001 / arxgenpsixiatriya.2010.76. PMID 20529994.
- ^ Bachman JG, Wadsworth KN, O'Malley PM, Johnston LD, Schulenberg JE (1997). Yoshlik davrida chekish, ichkilikbozlik va giyohvand moddalarni iste'mol qilish: yangi erkinliklar va yangi majburiyatlarning ta'siri. Hillsdeyl, NJ: L. Erlbaum Associates. p.70. ISBN 978-0-8058-2547-3.
- ^ Doherty EW, Doherty WJ (1998). "Sizning ko'zingizga tutun tushadi: Amerika kattalaridagi milliy namunadagi sigaret chekish va ajralish". Oilalar, tizimlar va sog'liq. 16 (4): 393–400. doi:10.1037 / h0089864.
- ^ a b Almeyda OP, Xulz GK, Lourens D, Fliker L (2002 yil yanvar). "Chekish Altsgeymer kasalligi uchun xavf omili sifatida: vaziyatni nazorat qilish va kohort tadqiqotlarini muntazam ravishda ko'rib chiqishda qarama-qarshi dalillar". Giyohvandlik. 97 (1): 15–28. doi:10.1046 / j.1360-0443.2002.00016.x. PMID 11895267. S2CID 22936675.
- ^ Anstey KJ, fon Sanden C, Salim A, O'Kearney R (2007 yil avgust). "Chekish demans va kognitiv pasayish uchun xavfli omil sifatida: istiqbolli tadqiqotlar meta-tahlili". Amerika Epidemiologiya jurnali. 166 (4): 367–78. doi:10.1093 / aje / kwm116. PMID 17573335.
- ^ Jacobsen LK, Krystal JH, Mencl WE, Westerveld M, Frost SJ, Pugh KR (yanvar 2005). "Chekish va chekishni taqiqlashning o'spirin tamaki chekuvchilarida ongga ta'siri". Biologik psixiatriya. 57 (1): 56–66. doi:10.1016 / j.biopsych.2004.10.022. PMID 15607301. S2CID 10146493.
- ^ Brody AL, Mandelkern MA, Jarvik ME, Li GS, Smit EC, Xuang JK, Bota RG, Bartzokis G, London ED (yanvar 2004). "Chekuvchilar va chekuvchilar o'rtasidagi mintaqaviy kulrang moddalar hajmi va zichligi o'rtasidagi farqlar". Biologik psixiatriya. 55 (1): 77–84. doi:10.1016 / S0006-3223 (03) 00610-3. PMID 14706428. S2CID 25442824.
- ^ Akiyama H, Meyer JS, Mortel KF, Terayama Y, Tornbi JI, Konno S (noyabr 1997). "Oddiy odamning qarishi: miya atrofiyasini keltirib chiqaradigan omillar". Nevrologiya fanlari jurnali. 152 (1): 39–49. doi:10.1016 / S0022-510X (97) 00141-X. PMID 9395125. S2CID 24676760.
- ^ Kataldo JK, Prochaska JJ, Glantz SA (2010). "Sigaret chekish Altsgeymer kasalligi uchun xavf omilidir: tamaki sanoatiga mansubligini nazorat qiluvchi tahlil". Altsgeymer kasalligi jurnali. 19 (2): 465–80. doi:10.3233 / JAD-2010-1240. PMC 2906761. PMID 20110594.
- ^ Fratiglioni L, Vang XX (2000 yil avgust). "Chekish va Parkinson va Altsgeymer kasalligi: epidemiologik tadqiqotlarni qayta ko'rib chiqish". Xulq-atvorni o'rganish. 113 (1–2): 117–20. doi:10.1016 / S0166-4328 (00) 00206-0. PMID 10942038. S2CID 4045868.
- ^ Kataldo JK, Prochaska JJ, Glantz SA (Iyul 2010). "Sigaret chekish Altsgeymer kasalligi uchun xavf omilidir: tamaki sanoatiga mansubligini nazorat qiluvchi tahlil". Altsgeymer kasalligi jurnali. 19 (2): 465–80. doi:10.3233 / JAD-2010-1240. PMC 2906761. PMID 20110594.
- ^ Allam MF, Kempbell MJ, Hofman A, Del Castillo AS, Fernández-Crehuet Navajas R (iyun 2004). "Chekish va Parkinson kasalligi: istiqbolli tadqiqotlarni muntazam ravishda ko'rib chiqish". Harakatning buzilishi. 19 (6): 614–21. doi:10.1002 / mds.20029. PMID 15197698. S2CID 36001133.
- ^ Allam MF, Kempbell MJ, Del Kastillo AS, Fernández-Crehuet Navajas R (2004). "Parkinson kasalligi chekishdan saqlaydi?". Xulq-atvor nevrologiyasi. 15 (3–4): 65–71. doi:10.1155/2004/516302. PMC 5488608. PMID 15706049.
- ^ Quik M (sentyabr 2004). "Chekish, nikotin va Parkinson kasalligi". Nörobilimlerin tendentsiyalari. 27 (9): 561–8. doi:10.1016 / j.tins.2004.06.008. PMID 15331239. S2CID 42385863.
- ^ Stough C, Mangan G, Bates T, Pellett O (1994 yil noyabr). "Chekish va Raven IQ". Psixofarmakologiya. 116 (3): 382–4. doi:10.1007 / BF02245346. PMID 7892431. S2CID 19155259.
- ^ Jarvis MJ (2004 yil yanvar). "Nega odamlar chekishadi". BMJ. 328 (7434): 277–9. doi:10.1136 / bmj.328.7434.277. PMC 324461. PMID 14751901.
- ^ "NICOU - Klinik: Nikotin va metabolitlar, siydik". www.mayomedicallaboratories.com. Olingan 2018-01-03.
- ^ Xyuz JR (2006 yil aprel). "Tamakidan voz kechishning klinik ahamiyati". Nikotin va tamaki tadqiqotlari. 8 (2): 153–6. doi:10.1080/14622200500494856. PMID 16766409.
- ^ McNeill A (2001). "Chekish va ruhiy salomatlik - adabiyotga sharh" (PDF). SmokeFree London dasturi. Olingan 2008-10-05. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ Meltzer H, Gill B, Petticrew M, Xinds K (1995). OPCS Psixiatriya kasalligi bo'yicha hisobot 3: Psixiatrik kasalliklarga chalingan kattalarning iqtisodiy faoliyati va ijtimoiy faoliyati. London, Buyuk Britaniyaning ish yuritish idorasi.[sahifa kerak ]
- ^ Kelly C, McCreadie RG (1999 yil noyabr). "Nitsddale, Shotlandiyadagi shizofreniya kasallarining chekish odatlari, hozirgi alomatlari va premorbid xususiyatlari". Amerika psixiatriya jurnali. 156 (11): 1751–7. doi:10.1176 / ajp.156.11.1751 (harakatsiz 2020-10-17). PMID 10553739.CS1 maint: DOI 2020 yil oktyabr holatiga ko'ra faol emas (havola)
- ^ Xyuz JR, Xatsukami DK, Mitchell JE, Dahlgren LA (avgust 1986). "Psixiatriya ambulatoriyalari orasida chekishning tarqalishi". Amerika psixiatriya jurnali. 143 (8): 993–7. CiteSeerX 10.1.1.470.8010. doi:10.1176 / ajp.143.8.993. PMID 3487983.
- ^ Shreder SA (sentyabr 2007). "Shattak ma'ruzasi. Biz bundan ham yaxshiroq - Amerika xalqining sog'lig'ini yaxshilashimiz mumkin". Nyu-England tibbiyot jurnali. 357 (12): 1221–8. doi:10.1056 / NEJMsa073350. PMID 17881753. S2CID 12299551.
- ^ Jorj T (2002-07-22). "Shizofreniya va chekish". Sog'liqni saqlash hisoboti. ABC Radio National (Avstraliya Broadcasting Corporation). Olingan 2012-05-06.
- ^ Sacco KA, Bannon KL, George TP (2004 yil dekabr). "Nikotinik retseptorlari mexanizmlari va normal holatdagi va neyropsikiyatrik kasalliklar". Psixofarmakologiya jurnali. 18 (4): 457–74. doi:10.1177/0269881104047273. PMC 1201375. PMID 15582913.
- ^ Kumari V, Postma P (2005). "Shizofreniyada nikotindan foydalanish: o'z-o'zini davolash gipotezasi". Neyrologiya va biobehavioral sharhlar. 29 (6): 1021–34. doi:10.1016 / j.neubiorev.2005.02.006. PMID 15964073. S2CID 15581894.
- ^ Gurillo P, Jauhar S, Murray RM, MacCabe JH (avgust 2015). "Tamakidan foydalanish psixozni keltirib chiqaradimi? Tizimli tekshirish va meta-tahlil". Lanset. Psixiatriya. 2 (8): 718–725. doi:10.1016 / S2215-0366 (15) 00152-2. PMC 4698800. PMID 26249303.
- ^ Anda RF, Uilyamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL (sentyabr 1990). "Depressiya va chekish dinamikasi. Milliy istiqbol". JAMA. 264 (12): 1541–5. doi:10.1001 / jama.1990.03450120053028. PMID 2395193.
- ^ Glassman AH, Helzer JE, Covey LS, Kottler LB, Stetner F, Tipp JE, Jonson J (sentyabr 1990). "Chekish, chekishni tashlash va katta depressiya". JAMA. 264 (12): 1546–9. doi:10.1001 / jama.1990.03450120058029. PMID 2395194.
- ^ Covey LS, Glassman AH, Stetner F (1998). "Sigaret chekish va katta depressiya". Qo'shadi kasalliklari jurnali. 17 (1): 35–46. doi:10.1300 / J069v17n01_04. PMID 9549601.
- ^ Hall SM, Muñoz RF, Reus VI, Sees KL (oktyabr 1993). "Nikotin, salbiy ta'sir va depressiya". Konsalting va klinik psixologiya jurnali. 61 (5): 761–7. doi:10.1037 / 0022-006X.61.5.761. PMID 7902368.
- ^ Vang M, Vang ZP, Gong R, Zhao ZT (2014 yil yanvar). "Homiladorlik paytida onaning chekishi va nasl-nasabdagi naycha nuqsonlari: meta-tahlil". Bolaning asab tizimi. 30 (1): 83–9. doi:10.1007 / s00381-013-2194-5. PMID 23760473. S2CID 40996359.
- ^ Uord S, Lyuis S, Koulman T (2007 yil may). "Homiladorlik paytida onaning chekishi va atrofdagi tamaki tutunining tarqalishi va tug'ilish vazniga ta'siri: Millennium Cohort yordamida retrospektiv o'rganish". BMC sog'liqni saqlash. 7: 81. doi:10.1186/1471-2458-7-81. PMC 1884144. PMID 17506887.
- ^ Kroon LA (sentyabr 2007). "Chekish bilan giyohvandlikning o'zaro ta'siri". Amerika sog'liqni saqlash tizimi farmatsiyasi jurnali. 64 (18): 1917–21. doi:10.2146 / ajhp060414. PMID 17823102. S2CID 5397510.
- ^ Ande A, McArthur C, Ayuk L, Avasom C, Achu PN, Njinda A, Sinha N, Rao PS, Agudelo M, Nookala AR, Simon S, Kumar A, Kumar S (2015). "OIV bilan kasallangan odamlarda virusning yuki, sitokinlar, oksidlovchi stress va sitokrom P450 fermentlariga engil va o'rtacha chekishning ta'siri". PLOS ONE. 10 (4): e0122402. Bibcode:2015PLoSO..1022402A. doi:10.1371 / journal.pone.0122402. PMC 4399877. PMID 25879453.
- ^ Chen X, Vlahos R, Bozinovski S, Jons J, Anderson GP, Morris MJ (aprel 2005). "Qisqa muddatli sigareta tutunining tana vazniga, ishtahaga va sichqonlarda miya neyropeptidiga ta'siri". Nöropsikofarmakologiya. 30 (4): 713–9. doi:10.1038 / sj.npp.1300597. PMID 15508020. Xulosa – News-Medical.Net.
- ^ Vanni H, Kazeros A, Vang R, Xarvi BG, Ferris B, De BP, Kerolan BJ, Xyubner RH, O'Konnor TP, Kristal RG (may, 2009). "Sigaret chekish odamda yog'ni kamaytiradigan AZGP1 genining haddan tashqari ta'sirlanishiga olib keladi". Ko'krak qafasi. 135 (5): 1197–1208. doi:10.1378 / ko'krak.08-1024. PMC 2679098. PMID 19188554.
- ^ Leistikow BN, Martin DC, Milano CE (avgust 2000). "Yong'in shikastlanishi, falokatlar va sigareta va sigaret chiroqlarining harajatlari: global nuqtai". Profilaktik tibbiyot. 31 (2 Pt 1): 91-9. doi:10.1006 / pmed.2000.0680. PMID 10938207. S2CID 11722177.
- ^ Leistikow BN, Martin DC, Samuels SJ (2000 yil dekabr). "Chekuvchilarda shikastlanish o'limi haddan oshdi: 1990-95 yillarda Amerika Qo'shma Shtatlarining milliy kohort tadqiqotlari". Shikastlanishning oldini olish. 6 (4): 277–80. doi:10.1136 / ip.6.4.277. PMC 1730660. PMID 11144627.
- ^ Cosnes J, Carbonnel F, Carrat F, Beaugerie L, Cattan S, Gendre J (1999 yil noyabr). "Hozirgi va ilgari chekilgan sigaretaning Crohn kasalligining klinik yo'nalishiga ta'siri". Alimentar farmakologiya va terapiya. 13 (11): 1403–11. doi:10.1046 / j.1365-2036.1999.00630.x. PMID 10571595. S2CID 6620451.
- ^ Calkins BM (dekabr 1989). "Ichakning yallig'lanishli yallig'lanishida chekishning rolini meta-tahlil qilish". Ovqat hazm qilish kasalliklari va fanlari. 34 (12): 1841–54. doi:10.1007 / BF01536701. PMID 2598752. S2CID 5775169.
- ^ Lakatos PL, Szamosi T, Lakatos L (dekabr 2007). "Ichakning yallig'lanishli kasalliklarida chekish: yaxshi, yomonmi yoki xunukmi?". Jahon Gastroenterologiya jurnali. 13 (46): 6134–9. doi:10.3748 / wjg.13.6134. PMC 4171221. PMID 18069751.
- ^ Mahid SS, Minor KS, Soto RE, Hornung CA, Galandiuk S (2006 yil noyabr). "Chekish va yallig'lanishli ichak kasalligi: meta-tahlil". Mayo klinikasi materiallari. 81 (11): 1462–71. doi:10.4065/81.11.1462. PMID 17120402.
- ^ Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ (2004 yil oktyabr). "Demografik, antropometrik va turmush tarzi omillari bo'yicha laparoskopik tasdiqlangan endometrioz bilan kasallanish". Amerika Epidemiologiya jurnali. 160 (8): 784–96. doi:10.1093 / aje / kwh275. PMID 15466501.
- ^ Calhaz-Jorge C, Mol BW, Nunes J, Costa AP (sentyabr 2004). "Portugaliyaning bepusht populyatsiyasida endometriozning klinik bashorat qiluvchi omillari". Inson ko'payishi. 19 (9): 2126–31. doi:10.1093 / humrep / deh374. PMID 15229202.
- ^ Baron JA (1996 yil yanvar). "Nikotin va sigareta chekishning foydali ta'siri: haqiqiy, mumkin va soxta". Britaniya tibbiyot byulleteni. 52 (1): 58–73. doi:10.1093 / oxfordjournals.bmb.a011533. PMID 8746297.
- ^ Shvarts SM, Marshall LM, Baird DD (oktyabr 2000). "Bachadon leiomyomati etiologiyasini tushunishga epidemiologik hissa qo'shish". Atrof muhitni muhofaza qilish istiqbollari. 108 5-qo'shimcha: 821-7. doi:10.1289 / ehp.00108s5821. JSTOR 3454313. PMID 11035989.
- ^ Lyubin JH, Shtayndorf K (yanvar 1995). "Sigaretadan foydalanish va Qo'shma Shtatlarda radonga tegishli o'pka saratonini baholash". Radiatsion tadqiqotlar. 141 (1): 79–85. Bibcode:1995 RadR..141 ... 79L. doi:10.2307/3579093. JSTOR 3579093. PMID 7997518.
- ^ Reid A, de Klerk NH, Ambrosini GL, Berry G, Musk AW (2006 yil avgust). "O'pka saratoni xavfi asbestga ta'sir qilishni to'xtatgandan va chekishni tashlagan vaqtdan beri ko'paymoqda". Kasbiy va atrof-muhit tibbiyoti. 63 (8): 509–12. doi:10.1136 / oem.2005.025379. PMC 2078130. PMID 16849527.
- ^ Lederle FA, Larson JK, Margolis KL, Allison MA, Freiberg MS, Cochrane BB, Graettinger WF, Curb JD (oktyabr 2008). "Ayollar salomatligi tashabbusida qorin aorta anevrizmasi: kohort o'rganish". BMJ. 337: a1724. doi:10.1136 / bmj.a1724. PMC 2658825. PMID 18854591. Xulosa – Bugungi tibbiy yangiliklar.
- ^ Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman JA, Fujiwara S, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (fevral 2005). "Chekish va sinish xavfi: meta-tahlil". Osteoporoz Xalqaro. 16 (2): 155–62. doi:10.1007 / s00198-004-1640-3. PMID 15175845. S2CID 19890259.
- ^ Sørensen LT (aprel 2012). "Jarohatni davolash va jarrohlik yo'li bilan yuqtirish. Chekish va chekishni tashlashning klinik ta'siri: tizimli tahlil va meta-tahlil". Jarrohlik arxivi. 147 (4): 373–83. doi:10.1001 / archsurg.2012.5. PMID 22508785.
- ^ "Chekish va diabet". Kasalliklarni nazorat qilish va oldini olish markazlari. 23 aprel 2018 yil.
- ^ "2014 yilgi umumiy jarrohning hisoboti: Chekishning sog'liq uchun oqibatlari - 50 yillik taraqqiyot". Kasalliklarni nazorat qilish va oldini olish markazlari. 5 mart 2018 yil.
- ^ Cohen DJ, Doucet M, Cutlip DE, Ho KK, Popma JJ, Kuntz RE (avgust 2001). "Teri osti koronar aralashuvidan keyin chekishning klinik va angiografik restenozga ta'siri: chekuvchilarning yana bir paradoksimi?". Sirkulyatsiya. 104 (7): 773–8. doi:10.1161 / hc3201.094225. PMID 11502701.
- ^ Goldman SM (2014). "Atrof-muhit toksinlari va Parkinson kasalligi". Farmakologiya va toksikologiyaning yillik sharhi. 54: 141–64. doi:10.1146 / annurev-pharmtox-011613-135937. PMID 24050700.
- ^ Pradhan P, Tirumala S, Liu X, Sayer JM, Jerina DM, Yeh HJ (may 2001). "(+) - (7S, 8R, 9S, 10R) -7,8-dihidroksi-9,10-epoksi-7,8,9,10-tetrahidrobenzoning trans-ochilgan (10S) -dA qo'shimchasining eritma tuzilishi [a] piren to'liq komplementar DNK dupleksida: katta sin konformatsiyasining dalili ". Biokimyo. 40 (20): 5870–81. doi:10.1021 / bi002896q. PMID 11352722.
- ^ Bray F, Tyczynski JE, Parkin DM (2004 yil yanvar). "Yuqoriga ko'tarilasizmi yoki pastga tushasizmi? 1967 yildan 1999 yilgacha Evropa Ittifoqining 15 mamlakatida o'pka saratoni epidemiyasining o'zgaruvchan bosqichlari". Evropa saraton jurnali. 40 (1): 96–125. doi:10.1016 / j.ejca.2003.08.005. PMID 14687795.
- ^ Jons M, Fosberi R, Teylor D (2000). "O'z-o'zini baholash savollariga javoblar". Biologiya 1. Kembrij ilg'or fanlari. p. 250. ISBN 978-0-521-78719-2.
- ^ a b Feng Z, Xu V, Xu Y, Tang MS (2006 yil oktyabr). "Akrolein - bu sigareta bilan bog'liq o'pka saratonining asosiy agenti: mutanosib issiq p53 nuqtalarida imtiyozli bog'lanish va DNKning tiklanishiga to'sqinlik qilish". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 103 (42): 15404–9. Bibcode:2006 yil PNAS..10315404F. doi:10.1073 / pnas.0607031103. PMC 1592536. PMID 17030796.
- ^ Doktor C. Everett Koop. "Chekish va tutunsiz tamaki". Arxivlandi asl nusxasi 2006 yil 23 iyulda. Olingan 15 iyul, 2006.
- ^ Hecht, S. S. (1999). "Tamaki tutunidagi kanserogen moddalar va o'pka saratoni". Milliy saraton institutining JNCI jurnali. 91 (14): 1194–1210. doi:10.1093 / jnci / 91.14.1194. PMID 10413421. Olingan 8 sentyabr 2014.
- ^ "Benzopiren bilan DNKning o'zaro ta'siri". DNK. Arxivlandi asl nusxasi 2004 yil 23 dekabrda. Olingan 5 mart, 2005.
- ^ Kataoka H, Sumida A, Makita M (1997). "Sigaret tutunidagi alifatik va aromatik aldegidlarni gaz fotometrik aniqlash bilan gaz xromatografiyasi yordamida aniqlash". Xromatografiya. 44 (9–10): 491–6. doi:10.1007 / BF02466742. S2CID 97329744.
- ^ Sumner PE, Mur JM, Boyette MD. "Tamaki bilan davolash uchun omborlarni qayta jihozlash" (PDF). Qo'shimcha muhandislik nashrlari. Jorjiya universiteti qishloq xo'jaligi va atrof-muhit fanlari kolleji. Olingan 2012-05-06.
- ^ NOVA. "Xavfsizroq sigaret izlang".
- ^ Godish T (2001). Yopiq atrof-muhit sifati. Michigan, Chelsi: Lyuis noshirlari. 77-9 betlar. ISBN 978-1-56670-402-1.
- ^ "Chekish, sog'liq va shaxs". REBEK. 2015 yil 13-may. Arxivlangan asl nusxasi 2015-05-18. Olingan 2015-05-13.
- ^ AQSh armiyasi Salomatlikni mustahkamlash va profilaktika tibbiyoti markazi. "Potentsial ta'sir qilish va / yoki ifloslanishning radiologik manbalari" (PDF). Arxivlandi asl nusxasi (PDF) 2006 yil 12 dekabrda.
- ^ Martell EA (mart 1983). "Chekuvchilarning bronxial bifurkatsiyada alfa-radiatsiya dozasi, ichkarida radon nasliga ta'sir qilish". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 80 (5): 1285–9. Bibcode:1983PNAS ... 80.1285M. doi:10.1073 / pnas.80.5.1285. PMC 393580. PMID 6572389.
- ^ Muggli ME, Ebbert JO, Robertson C, Xurt RD (sentyabr 2008). "Uyqudagi gigantni uyg'otish: tamaki sanoatining polonyum-210 chiqishiga munosabati". Amerika sog'liqni saqlash jurnali. 98 (9): 1643–50. doi:10.2105 / AJPH.2007.130963. PMC 2509609. PMID 18633078.
- ^ Rego B (sentyabr 2009). "Polonium qisqacha bayoni: saraton, nurlanish va tamaki sanoatining yashirin tarixi" (PDF). Isis; fan tarixi va uning madaniy ta'siriga bag'ishlangan xalqaro sharh. 100 (3): 453–84. doi:10.1086/644613. PMID 19960838. Arxivlandi asl nusxasi (PDF) 2016-03-04 da. Olingan 2014-07-20.
- ^ Radiatsion xavfsizlik bo'limi tadqiqot xizmatlari idorasi. "F. Radiatsiya ta'sirining odatiy manbalari". Amerika Qo'shma Shtatlarining Sog'liqni saqlash milliy institutlari. Arxivlandi asl nusxasi 2013-06-13. Olingan 2012-05-06.
- ^ "Xray va KT imtihonlari uchun radiatsiya xavfi -". dozalash jadvali. Birlashgan radiologlar. Arxivlandi asl nusxasi 2012 yil 26 aprelda. Olingan 2012-05-06.
- ^ "Radiatsion xatarlar va haqiqatlar" (PDF). Qo'shma Shtatlar atrof-muhitni muhofaza qilish agentligi. 2014-07-16.
- ^ a b "Har kuni radiatsiya ta'sirida". Old chiziq. Jamoat eshittirish tizimi.
- ^ "Yaponiya portlashidan keyin radiatsiya qo'rqadi". BBC. 2011-07-21.
- ^ Proktor RN (2006-12-01). "Poloniy bilan puflash". The New York Times.
- ^ "Tamaki tutuni | Radiatsiyadan himoya". Qo'shma Shtatlar atrof-muhitni muhofaza qilish agentligi. Olingan 2012-05-06.
- ^ Hecht SS (iyul 1999). "Tamaki tutunidagi kanserogenlar va o'pka saratoni". Milliy saraton instituti jurnali. 91 (14): 1194–210. doi:10.1093 / jnci / 91.14.1194. PMID 10413421.
- ^ Hecht, S. S. (2011). "Tamaki tutuni kanserogenlari va o'pka saratoni". Penningda T. M. (tahrir). Kimyoviy kanserogenez. Totova, NJ: Springer. p. 67. ISBN 9781617379949.
- ^ a b v d Messner B, Bernxard D (2014). "Chekish va yurak-qon tomir kasalliklari: endotelial disfunktsiya mexanizmlari va erta aterogenez". Arterioskleroz, tromboz va qon tomir biologiyasi. 34 (3): 509–515. doi:10.1161 / ATVBAHA.113.300156. PMID 24554606.
- ^ Bonetti PO, Lerman LO, Lerman A (2003). "Endotelial disfunktsiya: aterosklerotik xavf belgisi". Arterioskleroz, tromboz va qon tomir biologiyasi. 23 (2): 168–175. doi:10.1161 / 01.ATV.0000051384.43104.FC. PMID 12588755. S2CID 34213675.
- ^ Talhout R, Opperhuizen A, van Amsterdam JG (2007 yil oktyabr). "Tamaki tutuniga qaramlikda asetaldegidning roli". Evropa neyropsikofarmakologiyasi. 17 (10): 627–36. doi:10.1016 / j.euroneuro.2007.02.013. PMID 17382522. S2CID 25866206.
- ^ Xilts PJ (1994-08-02). "Giyohvand moddalarning nisbatan o'ziga qaramligi". Nyu-York Tayms. Olingan 2012-05-06.
- ^ "Henningfield-Benowitz moddalarini taqqoslash jadvallari". Olingan 2012-05-06.
- ^ "AADAC | Tamaki haqidagi haqiqat - giyohvandlik". Alberta sog'liqni saqlash xizmatlari. Arxivlandi asl nusxasi 2014-02-25.
- ^ Gervais A, O'Loughlin J, Meshefedjian G, Bancej C, Tremblay M (avgust 2006). "O'smirlar orasida chekishdan foydalanishning tabiiy rivojlanish bosqichidagi muhim voqealar". CMAJ. 175 (3): 255–61. doi:10.1503 / cmaj.051235. PMC 1513423. PMID 16880445.
- ^ Milliy saraton instituti. "Chekishning zarari va sog'liqqa chekishning foydalari". Ma'lumotlar sahifasi. Amerika Qo'shma Shtatlarining Sog'liqni saqlash milliy institutlari. Olingan 2012-05-06.
- ^ Smit D (2000). "Chekish o'spirin depressiyasini kuchaytiradi". Psixologiya bo'yicha monitor. Amerika psixologik assotsiatsiyasi. Olingan 2012-05-06.
- ^ Giyohvandlik bo'yicha Milliy institut. "Materiya bo'yicha aql: tamakiga qaramlik". Amerika Qo'shma Shtatlarining Sog'liqni saqlash milliy institutlari. Arxivlandi asl nusxasi 2012-05-05 da. Olingan 2012-05-06.
- ^ Parkin C, Fairweather DB, Shamsi Z, Stanley N, Hindmarch I (mart 1998). "Sigareta chekishni tungi ishlashga ta'siri". Psixofarmakologiya. 136 (2): 172–8. doi:10.1007 / s002130050553. PMID 9551774. S2CID 22962937.
- ^ Maneckjee R, Minna JD (1994 yil oktyabr). "Opioidlar qo'zg'atadi, nikotin esa odamning o'pka saraton hujayralarida apoptozni bostiradi". Hujayraning o'sishi va farqlanishi. 5 (10): 1033–40. PMID 7848904.
- ^ Guillem K, Vouillac C, Azar MR, Parsons LH, Koob GF, Cador M, Stinus L (sentyabr 2005). "Monoamin oksidaza inhibatsiyasi kalamushlarda nikotinni o'z-o'zini boshqarish motivatsiyasini keskin oshiradi". Neuroscience jurnali. 25 (38): 8593–600. doi:10.1523 / JNEUROSCI.2139-05.2005. PMC 6725504. PMID 16177026.
- ^ Villégier AS, Blanc G, Glowinski J, Tassin JP (sentyabr 2003). "Nikotinga nisbatan vaqtinchalik xatti-harakatlarning sezgirligi monoamin oksidaz inhibitörleri bilan uzoq muddatli bo'ladi". Farmakologiya Biokimyo va o'zini tutish. 76 (2): 267–74. doi:10.1016 / S0091-3057 (03) 00223-5. PMID 14592678. S2CID 30370768.
- ^ a b "Tamaki tutun". Amerika o'pka assotsiatsiyasi. 2007 yil iyun. Olingan 2012-05-06.
- ^ ""Tamakisiz Florida ", Kasalliklarni nazorat qilish va oldini olish bo'yicha ma'lumotlar markazlari". Olingan 8 sentyabr 2014.
- ^ a b IARC-ning odamlarga kanserogen xavfini baholash bo'yicha ishchi guruhi (2007). "Tutunsiz tamaki va ba'zi bir tamakiga xos N-nitrosaminlar" (PDF). Odamlarga kanserogen xavfni baholash bo'yicha IARC monografiyalari. 89: 1–592. PMC 4781254. PMID 18335640.
- ^ "Saraton nima?". Batafsil qo'llanma. Amerika saraton kasalligi jamiyati. 2011-04-11.
- ^ Dollar KM, Mix JM, Kozlowski LT (may, 2008). "Kichik sigaralar, katta sigaralar: Internetdagi zararlar va zararlarni kamaytirish bo'yicha kamchiliklar va komissiyalar". Nikotin va tamaki tadqiqotlari. 10 (5): 819–26. CiteSeerX 10.1.1.1009.3126. doi:10.1080/14622200802027214. PMID 18569755.
- ^ Shanks TG, Berns DM (fevral, 1988). "Tamaki chekishining kasallik oqibatlari" (PDF). Shopland DR-da Burns DM, Hoffmann D, Cummings KM, Amacher RH (tahr.). Sigaretalar: sog'liqqa ta'siri va tendentsiyalari. Chekish va tamakiga qarshi monografiya № 9. Milliy saraton instituti. 105-60 betlar.
- ^ "Tamaki chekish va saraton kasalligi haqida savollar va javoblar". Milliy saraton instituti. 2000-03-07. Olingan 2008-10-21.
- ^ Misner, Jared (2009 yil 18-noyabr). "UF tadqiqotida o'spirinlar orasida ko'proq nargile tutuni bor". Mustaqil Florida alligatori.
- ^ Knishkowy B, Amitai Y (iyul 2005). "Suv quvurlari (nargile) chekish: paydo bo'lgan sog'liq uchun xavfli xatti-harakatlar". Pediatriya. 116 (1): e113-9. doi:10.1542 / peds.2004-2173. PMID 15995011.
- ^ Xurt RD (2010-02-20). "Nargile chekish: bu sigaretadan xavfsizroqmi?". Mayo klinikasi.
- ^ "MISIR: suv quvurini chekish sil kasalligining katta xavfini tug'diradi". IRIN. 2008 yil 24 mart.
- ^ "Misrliklar quvur chekish to'g'risida ogohlantirdilar". Avstraliyalik. Reuters. 2007 yil 17 mart.
- ^ a b Shihad A, Azar S, Antonios C, Haddad A (sentyabr 2004). "Nargile cube kafelarini chekishning topografik modeliga qarab: Livanning Beyrut shahridagi yuqori ijtimoiy-iqtisodiy ahvolda uchuvchi tadqiqot". Farmakologiya Biokimyo va o'zini tutish. 79 (1): 75–82. doi:10.1016 / j.pbb.2004.06.005. PMID 15388286. S2CID 29182130.
- ^ Djordjevich MV, Stellman SD, Zang E (2000 yil yanvar). "Sigaret chekuvchilarga etkazib beriladigan nikotin va o'pka kanserogenlari dozalari". Milliy saraton instituti jurnali. 92 (2): 106–11. doi:10.1093 / jnci / 92.2.106. PMID 10639511.
- ^ "JSST nargile sigareta kabi xavf tug'dirishi mumkinligi to'g'risida ogohlantiradi". USA Today. Associated Press. 2007 yil 29 may.
- ^ Natto SB (2005). "Saudiya Arabistoni aholisida tamaki chekish va periodontal sog'liq". Shved Dental Journal. Qo'shimcha (176): 8-52, tarkib. PMID 16223098.
- ^ Koch V (2005-12-28). "Nargile tendentsiyasi puflamoqda". USA Today. Olingan 2010-05-04.[yaxshiroq manba kerak ]
- ^ Sajid KM, Chaouachi K, Mahmud R (may 2008). "Narxni chekish va saraton kasalligi: eksklyuziv / har doim chekadigan odamlarda karsinoembriyonik antigen (CEA)". Zararni kamaytirish jurnali. 5: 19. doi:10.1186/1477-7517-5-19. PMC 2438352. PMID 18501010.
- ^ Koul PA, Hajni MR, Shayx MA, Xon UH, Shoh A, Xon Y, Ohangar AG, Tasleem RA (2011). "Hindiston yarim orolining Kashmir vodiysida nargile chekish va o'pka saratoni". Osiyo Tinch okeani saratonining oldini olish jurnali. 12 (2): 519–24. PMID 21545223.
- ^ Boffetta P, Hecht S, Grey N, Gupta P, Straif K (iyul 2008). "Tutunsiz tamaki va saraton". Lanset. Onkologiya. 9 (7): 667–75. doi:10.1016 / S1470-2045 (08) 70173-6. PMID 18598931.
- ^ "Bemorlar uchun xulosalar. Bolalar va o'spirinlarda tamaki iste'mol qilinishini oldini olish bo'yicha birlamchi tibbiy yordam: AQSh profilaktika xizmatlari ishchi guruhining tavsiyanomasi". Ichki tibbiyot yilnomalari. 159 (8): I-36. 2013 yil oktyabr. doi:10.7326/0003-4819-159-8-201310150-00699. PMID 23974179. S2CID 28035258.
- ^ "Bir quti sigaretaning o'rtacha narxi". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ "Soliqlar sigareta narxining ulushi sifatida". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ "Tamaki reklamasini taqiqlash to'g'risida". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ "Tamaki iste'molidan voz kechishda yordam berish". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ Guindon GE, Boisclair D (2003). Tamakidan foydalanishning o'tmishi, hozirgi va kelajakdagi tendentsiyalari (PDF). Vashington: Xalqaro tiklanish va taraqqiyot banki / Jahon banki. 13-16 betlar. ISBN 978-1-932126-66-2. Olingan 2009-03-22.
- ^ a b "WHO / WPRO chekish statistikasi". Jahon sog'liqni saqlash tashkilotining G'arbiy Tinch okeani mintaqaviy vakolatxonasi. 2002-05-28. Arxivlandi asl nusxasi 2009-11-08 kunlari. Olingan 2009-01-01.
- ^ "Yoshlar va elektron sigaretalar". Giyohvandlik bo'yicha Milliy institut. 2016-02-01. Olingan 2018-12-23.
- ^ "Bolalar, o'spirinlar va yosh kattalar uchun elektron sigareta xavfi to'g'risida tezkor ma'lumotlar". CDC. 2018-12-03. Olingan 2018-12-23.
- ^ Kasalliklarni nazorat qilish va oldini olish markazlari (CDC) (2007 yil noyabr). "Kattalar orasida sigaret chekish - Amerika Qo'shma Shtatlari, 2006 yil". MMWR. Kasallik va o'lim bo'yicha haftalik hisobot. 56 (44): 1157–61. PMID 17989644.
- ^ a b "2004 yilgi kasallikning global yukini yangilash" (PDF). Jahon Sog'liqni saqlash tashkiloti. 2008 yil. Olingan 2008-01-01.
- ^ a b "WHO / WPRO-Tobacco faktlari varaqasi". Jahon sog'liqni saqlash tashkilotining G'arbiy Tinch okeani mintaqaviy vakolatxonasi. 2007-05-29. Arxivlandi asl nusxasi 2009-02-07 da. Olingan 2009-01-01.
- ^ Boshlang'ich va o'rta ta'lim | Ekologik tamaki tutuni | 2001 yilgi "Bolalarni qo'llab-quvvatlash to'g'risida" gi qonun Bolalar xizmatlari uchun chekish chekmaslik siyosati | 4303-bo'lim
- ^ Colgrove J, Bayer R, Bachynski KE (iyun 2011). "Yashiradigan joy qolmadi? Chekishni jamoat joylaridan haydash". Nyu-England tibbiyot jurnali. 364 (25): 2375–7. doi:10.1056 / NEJMp1104637. PMID 21612464. S2CID 205107540.
Bibliografiya
- "Jahon tamaki epidemiyasi bo'yicha JSST hisoboti" (PDF). Jahon Sog'liqni saqlash tashkiloti. 2008 yil. Olingan 2008-01-01.
- "2004 yilgi kasallikning global yukini yangilash" (PDF). Jahon Sog'liqni saqlash tashkiloti. 2008 yil. Olingan 2008-01-01.
- "1-bob: Kirish va sababiy xulosaga yondashish" (PDF). 2004 yil umumiy jarrohning ma'ruzasi - chekishning sog'liq uchun oqibatlari (PDF). Vashington: Sog'liqni saqlash va aholiga xizmat ko'rsatish departamenti, Kasalliklarni nazorat qilish va oldini olish markazlari, Surunkali kasalliklarning oldini olish va salomatlikni targ'ib qilish milliy markazi, Chekish va sog'liq bo'yicha idora. 2004 yil. Olingan 2009-05-24.
- "Tamaki tutuniga beixtiyor ta'sir qilishning sog'liq uchun oqibatlari: general jarrohning hisoboti" (PDF). Atlanta, AQSh: AQSh Sog'liqni saqlash va aholiga xizmat ko'rsatish vazirligi, Kasalliklarni nazorat qilish va oldini olish markazlari, Surunkali kasalliklarning oldini olish va sog'liqni saqlashni qo'llab-quvvatlash milliy markazi, Chekish va sog'liq bo'yicha idora. 2006 yil. Olingan 2009-02-15.
- "2004 yil saraton kasalligi bo'yicha raqamlar va raqamlar: saraton kasalligining asosiy faktlari". Amerika saraton kasalligi jamiyati. Arxivlandi asl nusxasi 2009-02-12. Olingan 2009-01-21.
- Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo M, Pukkala E, Skytthe A, Hemminki K (2000 yil iyul). "Saraton kasalligini keltirib chiqaradigan atrof-muhit va irsiy omillar - Shvetsiya, Daniya va Finlyandiya egizaklari guruhlari tahlili". Nyu-England tibbiyot jurnali. 343 (2): 78–85. doi:10.1056 / NEJM200007133430201. PMID 10891514.
- Montesano R, Hall J (oktyabr 2001). "Odam saratonining ekologik sabablari". Evropa saraton jurnali. 37 Qo'shimcha 8: S67-87. doi:10.1016 / S0959-8049 (01) 00266-0. PMID 11602374.








