Tropik kasalliklarga beparvo qilingan - Neglected tropical diseases
| Tropik kasalliklarga beparvo qilingan | |
|---|---|
 | |
| Umumiy NTDlarning oltitasining global bir-biri bilan qoplanishi. Xususan, 2011 yilda gvineya qurtlari kasalligi, limfatik filariaz, onkocerciasis, shistosomiasis, tuproq bilan yuqadigan gelmintlar va traxoma. | |
| Mutaxassisligi | Yuqumli kasallik |
Tropik kasalliklarga beparvo qilingan (NTDlar) turli xil guruhdir tropik infektsiyalar kam daromadli populyatsiyada keng tarqalgan rivojlanayotgan mintaqalar ning Afrika, Osiyo, va Amerika.[1] Ularga turli xil patogenlar sabab bo'ladi viruslar, bakteriyalar, protozoa va parazit qurtlar (gelmintlar ). Ushbu kasalliklar uchta katta yuqumli kasalliklar bilan farqlanadi (OIV / OITS, sil kasalligi va bezgak ), bu odatda ko'proq davolanish va tadqiqot uchun mablag 'oladi.[2] Afrikaning Saxaradan janubida ushbu kasalliklarning ta'siri guruh bilan solishtirish mumkin bezgak va sil kasalligi.[3] NTD-ning birgalikdagi infektsiyasi, shuningdek, OIV / OITS va sil kasalligini o'limga olib kelishi mumkin.[4]
Ba'zi hollarda muolajalar nisbatan arzon. Masalan, davolash shistozomiya har bir bola uchun yiliga 0,20 AQSh dollarini tashkil etadi.[5] Shunga qaramay, 2010 yilda beparvo qilingan kasalliklarni nazorat qilish keyingi besh-etti yil ichida 2 milliarddan 3 milliard dollargacha mablag 'talab qilishi taxmin qilingan.[6] Ba'zi farmatsevtika kompaniyalari talab qilinadigan barcha dori terapiyasini xayr-ehson qilishga majbur bo'lishdi va ommaviy dorilarni qabul qilish (masalan, ommaviy degelmintizatsiya qilish ) bir nechta mamlakatlarda muvaffaqiyatli amalga oshirildi.[7] Biroq, profilaktika choralari ko'pincha rivojlangan dunyoda ko'proq mavjud, ammo kambag'al joylarda hamma uchun mavjud emas.[8]
Ichida rivojlangan mamlakatlar, e'tibordan chetda qolgan tropik kasalliklar jamiyatdagi eng qashshoqlarga ta'sir qiladi. Qo'shma Shtatlarda 1,46 milliongacha oila, shu jumladan 2,8 million bola kuniga ikki dollardan kam pulga yashaydi.[9] Bunday mamlakatlarda e'tibordan chetda qolgan tropik kasalliklarning og'irligi ko'pincha boshqa sog'liqni saqlash muammolari soyasida qolmoqda. Shu bilan birga, ko'plab bir xil masalalar rivojlanayotgan davlatlar kabi rivojlangan mamlakatlarda aholini xavf ostiga qo'yadi. Masalan, boshqa muammolar qashshoqlikdan kelib chiqishi mumkin, bu odamlarni ushbu kasallikning tarqalishiga olib keladi, masalan, etarli darajada etishmasligi uy-joy.[10]
Yigirma beparvo qilingan tropik kasalliklarga birinchi o'ringa qo'yilgan Jahon Sog'liqni saqlash tashkiloti (VOZ), ammo boshqa tashkilotlar NTDlarni boshqacha ta'riflashadi. Xromoblastomikoz va boshqa chuqur mikozlar, qoraqo'tir va boshqa ektoparazitlar va ilon chaqishi envenomation 2017 yilda ro'yxatga kiritilgan.[11] Ushbu kasalliklar umumiy 149 mamlakatda 1,4 milliarddan ortiq odamni qamrab olgan (shu jumladan 500 milliondan ortiq bolalar)[12] va rivojlanayotgan iqtisodiyotlarga har yili milliardlab dollar zarar etkazmoqda.[13] Ularning natijasi o'laroq, 2013 yilda 142 ming kishi o'lgan - bu 1990 yildagi 204 ming o'limga nisbatan.[14] Ushbu 20 kishidan ikkitasi maqsad qilingan yo'q qilish (drakunkulyaz (Gvineya-qurt kasalligi) 2015 yilgacha va yaws 2020 yilgacha), to'rttasi esa yo'q qilish uchun (traxoma, inson afrikalik tripanozomiya, moxov va limfatik filariaz ) 2020 yilgacha.[13]
Kasalliklar ro'yxati
O'rtasida ba'zi munozaralar mavjud JSSV, CDC va yuqumli kasalliklar bo'yicha mutaxassislar, qaysi kasalliklar beparvo qilingan tropik kasalliklar deb tasniflanadi. E'tiborsiz qoldirilgan tropik kasalliklar bo'yicha tadqiqotchi Fizi, e'tibordan chetda qolgan 13 tropik kasallikni qayd etdi: askariyaz, Buruli yarasi, Chagas kasalligi, drakunkulyaz, ankilomit infektsiya, inson Afrikalik tripanozomiya, Leyshmanioz, moxov, limfatik filariaz, onhocerciasis, shistozomiya, traxoma va trikuriyaz.[15] Fenvik beparvo qilingan 12 ta tropik kasallikni tan oladi: yuqoridagi kabi, ankilomitdan tashqari.[16]
Ushbu kasalliklar qo'zg'atuvchining to'rt xil sinfidan kelib chiqadi patogenlar: (i) protozoa (Chagas kasalligi, inson afrikalik tripanosomiozi, leyshmaniaziya uchun); (ii) bakteriyalar (Buruli yarasi, moxov, traxoma, yaws uchun), (iii) gelmintlar yoki metazoan qurtlar (sistitserkoz / taeniaz, drakunkulyoz, echinokokkoz, oziq-ovqat bilan bog'liq trematodiazlar, limfatik filariaz, onkocerciasis, shistosomiasis, tuproqdan yuqadigan gelmintoz ); va (iv) viruslar (deng va chikungunya, quturish).[iqtibos kerak ]
Jahon sog'liqni saqlash tashkiloti quyida keltirilgan yigirma kasallikni e'tibordan chetda qolgan tropik kasalliklar deb tan oladi.[17]
Buruli yarasi
Buruli yarasi bakteriya tomonidan kelib chiqadi Mikobakteriya yaralari.[21] Bu sabab bo'lgan organizmlar oilasi bilan bog'liq sil kasalligi va moxov, lekin Mikobakteriya yaralari to'qimalarni yo'q qiladigan toksin, mikolakton ishlab chiqaradi.[21] Buruli oshqozon yarasining tarqalishi noma'lum.[15] Ikkilamchi infektsiyalar o'limga olib kelishi mumkin bo'lsa-da, o'lim xavfi past.[22] Kasallik deformatsiya, nogironlik va terining shikastlanishi ko'rinishida bo'ladi, bu kasallikni erta davolash orqali oldini olish va antibiotiklar va jarrohlik amaliyoti bilan davolash mumkin.[22] U Afrika, Osiyo va Lotin Amerikasida joylashgan.[23]
Chagas kasalligi

Chagas kasalligi sifatida ham tanilgan Amerika tripanosomiozi. Chagas kasalligini yuqtirgan 15 millionga yaqin odam bor.[15] Kasallik ehtimoli immunitetga chalingan shaxslar, bolalar va qariyalar uchun yuqori, ammo erta davolansa juda past.[24] Chagas kasalligi qurbonlarni tezda o'ldirmaydi, aksincha yillar davomida zaiflashadigan surunkali alomatlarni keltirib chiqaradi. Bunga sabab a vektorli[25] protozoa[24] bilan aloqa qilish orqali tarqaladi Trypanosoma cruzi triatominning yuqtirilgan najasi (qotil ) xato. Protozoan organizmga bug 'chaqishi, terining sinishi yoki shilliq pardalar orqali kirishi mumkin. Infektsiya yuqtirilgan ovqatni iste'mol qilish va ifloslangan tana suyuqligi bilan aloqa qilish natijasida kelib chiqishi mumkin.[24] Chagas kasalligining ikki bosqichi mavjud. O'tkir davr odatda asemptomatik tarzda kechadi. Birinchi alomatlar odatda teridir chancres, bir tomonlama binafsha orbital shish, mahalliy limfoadenopatiyalar va isitma infektsiya joyiga qarab turli xil alomatlar bilan birga keladi.[24] Surunkali bosqich umumiy infektsiyalarning 30 foizida uchraydi[15] va asemptomatik (eng ko'p tarqalgan), yurak va ovqat hazm qilish lezyonlari bo'lgan uchta shaklga ega bo'lishi mumkin.[24]
Chagas kasalligining oldini olish uchun hasharotlar chaqishi, insektitsid sepish, uy sharoitini yaxshilash, yotoq tarmoqlari, gigienik oziq-ovqat, tibbiy yordam, laboratoriya mashg'ulotlari va sinovlar orqali oldini olish mumkin.[24] Bundan tashqari, dori-darmon bilan davolash mumkin, ammo bu jiddiy yon ta'sirga ega bo'lishi mumkin.[24] Buni a orqali aniqlash mumkin serologik test, garchi test juda to'g'ri emas.[15]
Deng va chikungunya
50-100 million bor dang virusi har yili infektsiyalar.[26] Denge isitmasi odatda o'limga olib kelmaydi, ammo to'rt serotipdan bittasi bilan yuqtirish boshqa serotiplarga nisbatan sezgirlikni oshirishi va natijada o'limga olib kelishi mumkin bo'lgan kasallik bo'lib, og'ir dang kasalligi deb nomlanadi.[26] Denge isitmasi a flavivirus, va asosan ısırığıyla tarqaladi Aedes aegypti chivin.[26] Dangga yoki og'ir dengga qarshi davolanish bundan mustasno palliativ yordam.[26] Alomatlar yuqori isitma va grippga o'xshash alomatlardir.[26] Osiyo, Lotin Amerikasi va Shimoliy Avstraliyada joylashgan.[26]
Chikungunya yuqtirgan arboviral kasallikdir A. albopictus va A. aegypti chivinlar. Virus birinchi bo'lib 1952 yilda Tanzaniyadagi epidemiyadan ajratilgan.[27] Chikungunya virusi Alphavirus turiga mansub va Togaviridae oilasiga kiradi.[27] Chikungunya so'zi Makonde bu "engashadigan narsa" degan ma'noni anglatadi va bu zaiflashadigan og'riyotgan og'rig'ining bemorga ta'sirini anglatadi.[27] Odatda 5-7 kundan keyin paydo bo'ladigan alomatlar dang bilan aralashishi mumkin va ular orasida isitma, toshma, bosh og'rig'i, og'riyotgan og'riqlar va shish paydo bo'lishi mumkin.[28] Kasallik asosan Afrika va Osiyoda uchraydi.[29]
Drakunkuliaz

Drakunkuliaz Gvineya-qurt kasalligi deb ham ataladi. 2019 yilda 53 ta holat 4 ta davlatda qayd etilgan.[30] 1986 yildagi 3500000 holatdan sezilarli pasayish.[31] Bu o'limga olib kelmaydi, ammo bir necha oylik harakatsizlikka olib kelishi mumkin.[32] Bunga ifloslangan ichimlik suvi sabab bo'ladi suv burgalari bilan kasallangan gvineya-qurt lichinkalar.[32] Infektsiyadan taxminan bir yil o'tgach, og'riqli pufakcha paydo bo'ladi va bir yoki bir nechta qurtlar paydo bo'ladi. Qurtlar 1 tagacha bo'lishi mumkin m uzoq.[32]Odatda uni Jahon sog'liqni saqlash tashkiloti ko'ngillilari davolaydilar, ular qurtlardan kelib chiqqan jarohatlarni tozalaydi va bog'laydi va har kuni qaytib kelib, qurtni yana bir necha dyuymga tortib oladi.[32] Drakunkuliazni suvni filtrlash, kasallik tarqalishini oldini olish uchun zudlik bilan kasallikni aniqlash, sog'liqni saqlashni o'rganish va hovuzlarni larvitsid bilan davolash orqali oldini olish mumkin. An yo'q qilish dastur tarqalishini kamaytirdi.[32] 2014 yildan boshlab[yangilash], to'rtta endemik mamlakat Chad, Efiopiya, Mali va Janubiy Sudan.[32]
Exinokokkoz
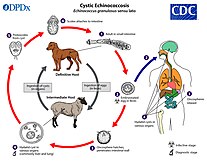
Stavkalari echinokokkoz Qishloq joylarida bu ko'rsatkich yuqoriroq va hozirgi kunda bu kasallikka chalingan milliondan ortiq odam bor.[33] Davolash qilinmagan alveolyar echinokokkoz o'limga olib keladi.[34] Bunga yutish sabab bo'ladi parazitlar hayvonlarning najasida.[35] Kasallikning ikkita versiyasi mavjud: kist va alveolyar. Ikkala versiya ham bir necha yil davomida asemptomatik inkubatsiya davrini o'z ichiga oladi. Kistik versiyada jigar kistalari qorin og'rig'iga, ko'ngil aynishiga va qayt qilishga olib keladi, o'pkada kistalar surunkali yo'tal, ko'krak qafasi og'rig'i va nafas qisilishiga olib keladi. Alveolyar echinokokkozda vazn yo'qotish, qorin og'rig'i, umumiy sog'liq hissi va jigar etishmovchiligi belgilaridan tashqari, odatda jigarda birlamchi kist rivojlanadi.[34]
Ekinokokkozni davolash uchun jarrohlik va dori vositalaridan ikkalasini ham qo'llash mumkin.[34] Buning oldini olish uchun itlarni degelmintizatsiya qilish, sanitariya, hayvonlarning najasini to'g'ri yo'q qilish, sog'liqni saqlash bo'yicha ta'lim va chorvachilikka qarshi emlash kerak.[36] Kistik echinokokkoz O'rta er dengizi mintaqasining sharqiy qismida, Afrikaning shimoliy qismida, janubiy va sharqiy Evropada, Janubiy Amerikaning janubiy qismida va Markaziy Osiyoda uchraydi. Alveolyar echinokokkoz Xitoyning g'arbiy va shimoliy qismida, Rossiyada, Evropada va Shimoliy Amerikada joylashgan.[35] Bu orqali tashxis qo'yish mumkin tasvirlash texnikasi va serologik testlar.[36]
Endemik treponematozlar (Yaws)

Ning tarqalishi to'g'risida cheklangan ma'lumotlar mavjud yaws, garchi bu birinchi navbatda bolalarga ta'sir qiladi.[37] O'lim xavfi juda past, ammo kasallik davolanmasa buzilish va nogironlikni keltirib chiqaradi.[37] Eng ko'p uchraydigan alomat - bu terining shikastlanishi.[37] Bu surunkali bakterial infeksiya bo'lib, teriga tegishi bilan yuqadi va spiroket bakteriya Treponema pallidum pertenue.[37] Antibiotiklar bilan davolanadi va yaxshilangan gigiena va sanitariya yordamida oldini olish mumkin.[37] Yawlar asosan Amerika, Afrika, Osiyo va Tinch okeanining iliq, nam, tropik mintaqalarida keng tarqalgan.[37]
Oziq-ovqat bilan bog'liq trematodiazlar
Oziq-ovqat bilan yuqadigan trematod infektsiyalari kiradi klonoroz, opistorxoz, fastsiyoliaz va paragonimiya. Ushbu yuqumli kasalliklar zoonoz bo'lib, birinchi navbatda uy yoki yovvoyi hayvonlarga ta'sir qiladi, shuningdek, odamlarga ham yuqadi. Ular parazitlarning lichinkali bosqichlari bilan ifloslangan, masalan, xom baliq kabi ovqat iste'mol qilish orqali olinadi. Kamida 40 million odam yuqtirgan deb o'ylashadi.[38]

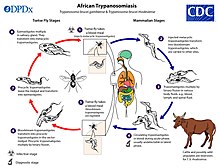
Inson afrikalik tripanosomiozi
Afrikalik tripanozomiya shuningdek, afrikalik uyqu kasalligi deb ham ataladi. Hozirda 10 mingdan kam holatlar mavjud.[39] Inson afrikalik tripanosomiozi vektorli, va tsetse pashshasining ısırığıyla tarqaldi.[25] Eng ko'p uchraydigan alomatlar isitma, bosh og'rig'i, limfadenopatiya, tungi uyqu tartibi, shaxsning o'zgarishi, kognitiv pasayish va koma. Kasallik davolanmasa, har doim o'limga olib keladi. Davolashning hozirgi shakllari juda toksik va samarasiz, chunki qarshilik tarqalmoqda. Bu arzon narx orqali aniqlanadi serologik sinov.[tibbiy ma'lumotnoma kerak ]
Leyshmanioz
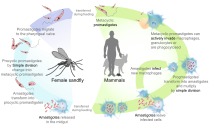
Ning uchta shakli leyshmanioz ichki organlar (Kala-azar ), teri va mukokutan.[40] Taxminan 12 million odam yuqtirgan.[15] Davolash qilinmasa o'lim bilan yakunlanadi va visseral leyshmaniozdan har yili 20000 o'lim ro'y beradi.[41] Bu vektorli ısırığından kelib chiqqan kasallik pashshalar.[25] Visseral leyshmaniozning kamida 90 foizi Bangladesh, Braziliya, Efiopiya, Hindiston, Janubiy Sudan va Sudanda uchraydi. Teri leyshmaniozi Afg'oniston, Jazoir, Braziliya, Kolumbiya, Eron, Pokiston, Peru, Saudiya Arabistoni va Suriyada uchraydi. Mukokutan leyshmaniozning 90 foizga yaqini Boliviya, Braziliya va Peruda uchraydi.[40]
Profilaktikaning yagona usuli - bu emlash, bu qumtepaning chaqishi va oldini olish bosqichida. Tashxisni klinik belgilar, serologik testlar yoki parazitologik testlarni aniqlash orqali aniqlash mumkin.[42] Leyshmaniozni qimmat dorilar yordamida davolash mumkin.[43]
Moxov
JSSTning so'nggi ma'lumotlariga ko'ra, 208 619 ta yangi holat moxov 2018 yilda 127 mamlakatdan xabar berilgan.[44] Angola, Braziliya, Markaziy Afrika Respublikasi, Kongo Demokratik Respublikasi, Hindiston, Madagaskar, Mozambik, Nepal va Tanzaniyada joylashgan.[45] O'tmishdagi yoki hozirgi moxovlik sababli hozirgi kunda nogiron yoki buzilgan bir milliondan ikki milliongacha odam bor.[46] Bunga bakteriyalar sabab bo'ladi va yuqtirgan odamlarning og'iz va burun tomchilari orqali yuqadi.[47] Agar moxov davolanmasa, buzilish va jismoniy nuqsonlarni keltirib chiqaradi. Agar u erta davolansa, davolanadi.[46]Davolash uchun ko'p dori terapiyasi kerak.[45] The BCG emlash moxovga qarshi ba'zi bir profilaktik ta'sirga ega. Moxov 5-20 yillik inkubatsiya davriga ega va uning belgilari teri, asab, ko'z va oyoq-qo'llarning shikastlanishi.[47]

Lenfatik filariaz

Lenfatik filariaz ham sifatida tanilgan fil. Taxminan 120 million odam yuqtirgan[48] va deformatsiyalari bilan 40 mln.[16] Taxminan uchdan ikki qismi Janubiy-G'arbiy Osiyoda va uchdan bir qismi Afrikada.[48] Lenfatik filariaz kamdan-kam hollarda o'limga olib keladi.[49] Lenfatik filariaz, umrbod ta'sir qiladi, masalan, oyoq-qo'llarning limfoödemasi, jinsiy a'zolar kasalligi va og'riqli takrorlanadigan hujumlar. Aksariyat odamlar asemptomatik, ammo limfatik zararga ega. Yuqtirilgan odamlarning 40 foizigacha buyragi shikastlangan.[50] Bu vektorli chivinlar orqali yuqadigan nematod qurtlari keltirib chiqaradigan kasallik.[25][50]
U tejamkor antihelminthic muolajalari bilan davolanishi mumkin,[51] va terini yuvish shikastlanishni sekinlashtirishi yoki hatto qaytarishi mumkin.[52] Barmoq bilan qon tekshiruvi tashxisi qo'yilgan.[49]
Onchocerciasis

Onchocerciasis "daryoning ko'rligi" deb ham nomlanadi. 20 million odam yuqtirgan[53] tarqalishi esa qishloq joylarida yuqori.[54] 99 foizdan ko'prog'i Afrikaning Sahroi Sahroda.[54] Bu ko'rlik, terida toshmalar, shikastlanishlar, kuchli qichishish va terining depigmentatsiyasini keltirib chiqaradi.[55] Bu vektorli filariya qurtlari yuqtirgan qora chivinlar keltirib chiqaradigan kasallik.[25][55]
Buni davolash mumkin ivermektin.[55] Bu hasharotlarga qarshi püskürtme yoki oldini olish bilan dozalash orqali oldini olish mumkin ivermektin.[54] Alomatlar odatda qichima va terining shikastlanishi.[54]
Quturish

Ning ikki shakli mavjud quturish: g'azablangan va shol. Har yili quturishdan 60 ming o'lim qayd etiladi.[56] Bu asosan Osiyo va Afrikada uchraydi.[56] Qishloq joylarda keng tarqalgan va bu bolalarga nomutanosib ta'sir qiladi.[57] Quturish odatda alomatlar paydo bo'lgandan keyin o'limga olib keladi.[58] Bunga sabab a lyssavirus yuqtirgan hayvonlarning yaralari yoki chaqishi orqali yuqadi.[57] Birinchi alomatlar bir oydan uch oygacha inkubatsiya davridan keyin paydo bo'ladigan yuqumli joy yaqinidagi isitma va og'riqdir. G'azablangan (tez-tez uchraydigan) quturish giperaktivlik, hidrofobiya, aerofobiya keltirib chiqaradi va kardio-nafas yo'llarining to'xtashi natijasida o'lim bir necha kun ichida sodir bo'ladi. Paralitik quturish falajdan komadan o'limgacha sekin rivojlanishni keltirib chiqaradi.[57]
Itlarda emlash orqali uni oldini olish mumkin,[57] va tishlangan yaralarni tozalash va dezinfektsiya qilish (ta'sirdan keyingi profilaktika ).[58] Kuchli alomatlar paydo bo'lishidan oldin tashxis qo'yish mumkin emas. Semptomlar paydo bo'lgandan keyin uni to'qimalarni sinash orqali aniqlash mumkin.[57]
Shistosomoz

200 milliondan ortiq holatlar mavjud shistozomiya.[16] Kasalliklarning taxminan 85 foizi Afrikaning Sahroi sharqida.[16] Kasallik siydik pufagi saratonini keltirib chiqarishi bilan o'limga olib kelishi mumkin gematemez.[16] Shistosoma turlar odamlar va chuchuk suvli salyangozlar o'rtasida o'zgarib turadigan murakkab hayot aylanishiga ega. Infektsiya parazitni olib yuradigan salyangozlar yashaydigan ifloslangan toza suv bilan teriga tushganda paydo bo'ladi. Shistosomozning belgilari qurtlardan emas, balki organizmning tuxumlarga bo'lgan reaktsiyasidan kelib chiqadi. Tanadan tashqariga chiqmagan tuxumlar ichak yoki siydik pufagiga joylashib, yallig'lanish yoki chandiqlarni keltirib chiqarishi mumkin. Bir necha marta yuqtirgan bolalarda kamqonlik, to'yib ovqatlanmaslik va o'qishda qiyinchiliklar paydo bo'lishi mumkin.[59] Alomatlar odatda gematuriya, qovuq obstruktsiyasi, buyrak etishmovchiligi, qovuq saratoni, periportal fibroz, siydik pufagi, jigar fibrozi, portal gipertenziya, bachadon bo'yni shikastlanishi, astsitlar va qizilo'ngach tomirlari.[15][16]
Arzon praziquantel shistosomiyoz bilan kasallangan odamlarni davolash uchun ishlatilishi mumkin, ammo reinfektsiyani oldini olmaydi. Profilaktika qiymati har bir bola uchun yiliga 0,32 AQSh dollarini tashkil etadi.[16] Ommaviy degelmintizatsiya schistosomiasisning oldini olish uchun prazikvantel bilan davolash, xavfsiz suvdan yaxshiroq foydalanish, sanitariya, sog'liqni saqlash bo'yicha ma'lumotlardan foydalanish mumkin.[15] Vaktsinalar ishlab chiqilmoqda. Bunga serologik tekshiruv orqali tashxis qo'yish mumkin, ammo u ko'pincha yolg'on salbiy narsalarni keltirib chiqaradi.[16]
Tuproq bilan yuqadigan gelmintoz

Uchta asosiy qurt turlari tuproqdan yuqadigan gelmintoz bor Ascaris (yumaloq qurtlar ), Trichuris (qamchi qurti ), ankilomaterlar Nekator amerikan va Ankilostoma o'n ikki barmoqli ichak va Strongyloides stercoralis.[60] Ayni paytda bu kasallikka chalingan 1,5 milliard kishi bor.[60] Tuproq bilan yuqadigan gemintioz Afrikaning Sahroi janubida, Amerika qit'asida, Xitoy va Sharqiy Osiyoda uchraydi.[60] O'lim xavfi juda past.[15] Eng keng tarqalgan alomatlar anemiya, o'sishni to'xtatish, ichak muammolari, energiya etishmasligi va jismoniy va kognitiv rivojlanish buzilgan.[15][60] Yuqtirilgan bolalar ko'pincha maktabdan orqada qoladilar.[15] Semptomlarning og'irligi tanadagi qurtlar soniga bog'liq.[60]
Parazit qurtlar, odatda, yuqtirgan odamning axlati va tuproqqa ta'sir qilish yo'li bilan atrof muhitga tarqaladi, masalan, ochiq axlat.[60] Eng keng tarqalgan davolash usuli tibbiyotdir.[60] Gigienik jihatdan tayyorlangan oziq-ovqat va toza suv yordamida uning oldini olish mumkin sanitariya, davriy degelmintizatsiya va sog'liqni saqlash bo'yicha ta'lim.[60] Jahon sog'liqni saqlash tashkiloti tavsiya qiladi ommaviy degelmintizatsiya qilish oldindan tashxis qo'ymasdan.[60]
Taeniaz / sistitserkoz
Sistitserkoz lenta qurtlari lichinkalari infektsiyasidir, shu bilan birga taeniaz kattalar bilan kasallanish lenta qurtlari .[61] Ikkalasi ham Osiyo, Afrika va Lotin Amerikasida, xususan, cho'chqalar inson najasiga uchragan fermalarda uchraydi.[62]
Sistitserkozning oldini olishning eng keng tarqalgan sababi hisoblanadi epilepsiya rivojlanayotgan dunyoda.[62] Sistitserkoz ifloslangan oziq-ovqat, suv yoki tuproqni yutgandan keyin paydo bo'ladi.[61] Kistalar va jarohatlar sabab bo'lishi mumkin bosh og'rig'i, ko'rlik, soqchilik, gidrosefali, meningit va dementia.[63] Neyrosistoserkoz yoki asab tizimining parazitar infektsiyasi o'limga olib kelishi mumkin. Taeniasis o'limga olib kelmaydi.[62][63] Odatda, pishmagan ifloslangan cho'chqa go'shtini iste'mol qilgandan keyin yuqadi. Taeniasis engil alomatlarga ega, jumladan qorin og'rig'i, ko'ngil aynish, diareya yoki ich qotishi.
Giyohvand moddalar ikkala kasallikni davolash uchun ishlatiladi.[63] Infektsiyani oldini olish uchun go'shtni tekshirish standartlarini kuchaytirish, chorva mollarini saqlash, gigiena va sanitariya holatini yaxshilash, sog'liqni saqlash bo'yicha ta'lim, go'shtni xavfsiz tayyorlash, odam va cho'chqa tashuvchilarni aniqlash va davolash mumkin.[64]
Traxoma
21,4 million odam yuqtirgan traxoma, ulardan 2,2 millioni qisman ko'r va 1,2 millioni ko'rlar. U Afrika, Osiyo, Markaziy va Janubiy Amerika, Yaqin Sharq va Avstraliyada joylashgan.[65] Kasallik nomutanosib ravishda ayollar va bolalarga ta'sir qiladi.[65] O'lim xavfi juda past, garchi ko'plab qayta infektsiyalar oxir oqibat ko'rlikka olib keladi.[15][65] Alomatlar ichki chandiqli ko'z qovoqlari, so'ngra ko'z qovoqlari ichkariga buriladi.[65] Traxoma, ko'z oqishi (qo'l, mato va boshqalarda) orqali tarqaladigan mikroorganizm va "ko'zni qidiradigan chivinlar" tufayli yuzaga keladi.[65]
Antibiotiklar bilan davolanadi. Faqat ma'lum bo'lgan profilaktika usuli - bu shaxslararo gigiena.
Xromoblastomikoz va boshqa chuqur mikozlar
Qo‘tir
Kiruvchi ilon chaqishi
Snakebite ro'yxatga 2017 yilda, faollar tomonidan JSSTni ko'p yillik tanqidlaridan so'ng, ushbu ustuvor vazifaga aylanmagani uchun qo'shilgan.[66] The ilon chaqishi kasalligining eng katta yuki Hindiston va Janubi-Sharqiy Osiyoda joylashgan. Jahon miqyosida har yili taxminan 421000 ta envenomiya (taxminan 4 ta ilonning bittasi) va 20000 ta o'lim mavjud, ammo ilon chaqishi haqida ko'pincha xabar berilmaydi.[67]
Sog'liqni saqlash ta'siri
Degelmintlarni davolash
Degelmintizatsiya yuqtirgan bolalarda davolanish ozgina ozuqaviy foyda keltirishi mumkin, chunki qurtlar ko'pincha to'yib ovqatlanmaslik uchun qisman javobgar bo'ladi.[16][68] Biroq, ushbu yuqumli kasalliklar tez-tez uchraydigan joylarda bunga kuchli dalillar mavjud ommaviy degelmintizatsiya qilish aktsiyalar bolalarning o'rtacha ovqatlanish darajasiga, qon darajasiga ijobiy ta'sir ko'rsatmaydi gemoglobin, bilim qobiliyatlari, maktabdagi ishlash yoki omon qolish.[68] Keyinchalik sog'liqni saqlash sohasidagi yutuqlarga erishish uchun yaxshilanishlar sanitariya degelmintizatsiya qilish muolajalari bilan birgalikda gigiena qoidalari ham talab qilinadi.[iqtibos kerak ]
Koinfektsiya
Koinfektsiya e'tiborsiz qoldirilgan tropik kasalliklar bilan bog'liq asosiy muammo bo'lib, NTDlarni ularga nisbatan ko'proq zarar etkazadi o'lim stavkalar tasvirlanishi mumkin. E'tiborsiz qoldirilgan tropik kasalliklarni qo'llab-quvvatlovchi omillar (qashshoqlik, sog'liqni saqlashning etarli darajada ta'minlanmaganligi, sanitariya talablarining etarli emasligi va boshqalar) barcha NTDlarni qo'llab-quvvatlaganligi sababli, ular ko'pincha taqsimotlarda uchraydi. Gelmint infektsiyalari, odamlarning eng keng tarqalgan infektsiyasi sifatida, ko'pincha ko'p infektsion tizimlarda topilgan. Masalan, Braziliyada past ijtimoiy-iqtisodiy ahvol uy-joylarning haddan tashqari ko'p bo'lishiga yordam beradi. Xuddi shu sohalarda ulanish Nekator amerikan va Shistosoma mansoni keng tarqalgan. Har bir qurtning ta'siri immunitet tizimi yuqtirganlarning infektsiyasini boshqasidan osonroq va og'irroq qilish. Shu sababli koinfektsiya o'lim xavfini oshiradi. NTDlar, masalan, boshqa kasalliklar bilan yuqtirishda ham rol o'ynashi mumkin bezgak, OIV / OITS va sil kasalligi. Gelmintlarning immunitet tizimini boshqarish qobiliyati fiziologik muhitni yaratishi mumkin, bu esa rivojlanishni kuchaytirishi mumkin. OIV / OITS.[69] Dan ba'zi dalillar Senegal, Malavi va Tailand gelmint infektsiyalari bezgak yuqtirish xavfini oshirishini ko'rsatdi.[70]
Davolashning integratsiyasi
NTDlarni tashabbuslarga kiritish bezgak, OIV / OITS va sil kasalligi, shuningdek, NTD davolash dasturlarini birlashtirish, ushbu kasalliklar va NTDlar o'rtasidagi bog'liqlikni hisobga olgan holda afzalliklarga ega bo'lishi mumkin.[2][70][71] Ba'zi e'tibordan chetda qolgan tropik kasalliklar umumiy vektorlarga ega (pashshalar, qora chivinlar va chivinlar).[70] Ham tibbiy, ham vektor nazorati bo'yicha harakatlar birlashtirilishi mumkin.[72]
Keng tarqalishi uchun to'rtta dorivor tez ta'sir etuvchi paket taklif qilingan. Davolashni ajratish va jamoat ishchilariga ish qo'shish o'rniga, birdaniga bir nechta kasalliklarga qarshi kurashish orqali ma'muriyat yanada samarali bo'lishi mumkin. Ushbu paket har bir bemor uchun 0,40 AQSh dollarini tashkil qilishi taxmin qilinmoqda. Mustaqil davolash bilan taqqoslaganda, jamg'arma 26-47% ni tashkil qiladi. NTD va boshqa kasalliklarning ham vektorda, ham inson bosqichida o'zaro ta'sirini tushunish uchun ko'proq tadqiqotlar o'tkazish kerak bo'lsa-da, xavfsizlikni baholash hozirgacha ijobiy natijalarga erishdi.[70]
Ko'plab e'tibordan chetda qolgan tropik kasalliklar va boshqa keng tarqalgan kasalliklar umumiy vektorlarga ega bo'lib, davolanish va boshqarish uchun integratsiyani boshqarish uchun yana bir imkoniyat yaratadi. Bunday misollardan biri bezgak va limfatik filariazdir. Ikkala kasallik ham bir xil yoki tegishli chivin vektorlari orqali yuqadi. Vektorli nazorat insektitsid bilan ishlangan to'rlarni tarqatish orqali odamning turli xil kasallik vektorlari bilan aloqasini kamaytiradi. Integratsiyalashgan vektor nazorati, shuningdek, giyohvand moddalarni ommaviy qabul qilish bosimini, ayniqsa tez rivojlanayotgan dori-darmonlarga nisbatan bosimni kamaytirishi mumkin. Vektorli nazoratni va dori-darmonlarni ommaviy administratsiyasini birlashtirish ikkalasini ham ta'kidlaydi va ularning har biri qarshilik evolyutsiyasiga kam ta'sir qiladi.[72]
Iqtisodiy samara
NTDlar uchun davolanishning arzonligi dasturlarning keng ko'lami, farmatsevtika kompaniyalari tomonidan dori-darmonlarni bepul etkazib berish, dori-darmonlarni etkazib berish usullari va dori-darmonlarni tarqatadigan pullik ko'ngillilar bilan bog'liq. NTDlarning iqtisodiy yuki yetarlicha baholanmagan va shuning uchun NTDlarning kamaygan tarqalishining tegishli iqtisodiy samarasi va iqtisodiy samaradorligi baholanmagan.[73] E'tiborsiz qoldirilgan tropik kasalliklarni nazorat qilish choralari bo'yicha investitsiya rentabelligi kasallik va mintaqaga qarab 14-30 foizni tashkil etadi.[74] Degelmintizatsiya qilishning uzoq muddatli foydalari qatoriga maktabga kelmaslik 25 foizga, kattalar daromadining 20 foizga o'sishi kiradi.[75]
Shu bilan birga, Buruli yarasi kabi ba'zi bir kasalliklarni davolash qiymati o'rtacha daromadga ega kvartilda o'rtacha bir xonadonning yillik daromadidan ikki baravar ko'p bo'lishi mumkin, eng yuqori daromadli kvartil uchun esa bu o'rtacha o'rtacha ko'rsatkichdan biroz pastroq. uy daromadlari. Ushbu ulkan moliyaviy xarajatlar ko'pincha davolanishni kechiktirishga va moliyaviy halokatga olib keladi, ammo iqtisodiy yuk jihatidan boy va kambag'allar o'rtasida tengsizlik mavjud. Ushbu kasalliklar, shuningdek, sog'liqni saqlash nuqtai nazaridan hukumatga qimmatga tushadi va kasallanish va umr ko'rishning qisqarishi tufayli ishchilarning mahsuldorligini yo'qotadi. Masalan, Keniyada degelmintizatsiya qilish kattalar o'rtacha daromadini 40 foizga oshirishi taxmin qilinmoqda, bu foyda-xarajat nisbati 100 ga teng. Har bir davolanmagan traxoma kasalligi yo'qolgan mahsuldorlik uchun 118 AQSh dollarini tashkil etadi. Shistosomozning har bir holati yiliga 45,4 kunlik ish yo'qotishiga olib keladi. Kasalliklarning aksariyati turli rivojlanayotgan mamlakatlar iqtisodiyotiga millionlab dollar zarar etkazmoqda. Keng miqyosli profilaktika kampaniyalari qishloq xo'jaligi mahsuloti va ta'lim darajasini oshirishi taxmin qilinmoqda.[73]
Ijtimoiy ta'sir
Ijtimoiy tamg'a
Kabi bir nechta NTDlar moxov, ijtimoiy isnodga olib keladigan og'ir deformatsiyalarni keltirib chiqaradi. Stigma beparvo qilingan tropik kasalliklarning "yashirin yuki" deb hisoblanadi va bu kabi choralar hisobga olinmaydi. nogironlik bo'yicha tuzatilgan hayot yillari (DALY). Og'ir ijtimoiy isnodga ega bo'lgan boshqa NTDlar kiradi onhocerciasis, limfatik filariaz, vabo, Buruli yarasi, leyshmanioz va Chagas kasalligi.[76] Lenfatik filariaz Masalan, og'ir deformatsiyalarni keltirib chiqaradi, natijada nikohdan voz kechish va mehnatga layoqatsizlik.[16] Gana va Shri-Lankada o'tkazilgan tadqiqotlar shuni ko'rsatdiki, limfatik filariaz bilan og'rigan bemorlarni qo'llab-quvvatlash guruhlari ijtimoiy qo'llab-quvvatlash va ularning kasalliklarini boshqarish bo'yicha amaliy maslahatlar berish orqali ishtirokchilarning o'z qadr-qimmatini, hayot sifatini va ijtimoiy munosabatlarini oshirishi mumkin. E'tiborsiz qoldirilgan tropik kasalliklarning ijtimoiy ta'siri erkaklar va ayollarga har xil ta'sir ko'rsatishi ko'rsatilgan. Erkaklar o'zlarining iqtisodiy istiqbollariga zararli ta'sir ko'rsatadigan tarzda ijtimoiy tahqirlanadi. Ayollar nikoh va oila sohasida ko'proq ta'sirlanishadi.[76]
Ruhiy salomatlikka ta'siri
2012 yilgi tadqiqotlar shuni ko'rsatdiki, e'tibordan chetda qolgan tropik kasallik bilan yuqtirish odamlarning ruhiy salomatligini yomonlashtiradi. Bu qisman NTDlarni o'rab turgan ijtimoiy stigma bilan bog'liq, ammo keyinchalik sog'liqni saqlash va ijtimoiy xizmatlardan foydalanish imkoniyatining etishmasligi sabab bo'lishi mumkin. Umuman olganda, yuqtirgan hamjamiyat a'zosi bo'lish fuqarolarni fuqarolik huquqlari, ta'lim olish imkoniyatlari va ish bilan ta'minlash orqali jamiyatning ko'p qirralaridan uzib qo'yishi aniqlandi. Mualliflar beparvo qilingan tropik kasalliklarning psixologik jihatlari, ularning birgalikdagi ta'sirini to'liq echish uchun ko'proq tadqiqotlar o'tkazishni taklif qilishadi.[77]
Jins
NTDlar nomutanosib ravishda ayollar va bolalarga ta'sir qiladi.[78] Bundan tashqari, homiladorlik paytida ankilomateriya yuqtirish xavfi va homiladorlik paytida Chagas kabi kasalliklarni yuqtirish imkoniyati mavjud. Ugandada o'tkazilgan tadqiqotlar shuni ko'rsatdiki, ayollar davolanishga osonroq erishdilar, chunki ular erkaklarnikiga qaraganda kasbiy majburiyatlari kam bo'lgan va davolanishga ko'proq ishonganlar, ammo homilador ayollarga dori vositalarining ta'sirini bilmaslik etarli darajada parvarish qilishni oldini olgan. Ugandada davolash dasturlarini ishlab chiqishda jinsi e'tiborga olinishi kerak degan xulosaga keladi.[79] Bundan tashqari, ayollar tez-tez turmushga chiqish bosimiga nisbatan og'ir ijtimoiy isnodga duchor bo'lishadi.[16][shubhali ][tekshirib bo'lmadi ]
Maktabga borish
Ommaviy degelmintizatsiya maktabga borishga ta'siri ziddiyatli. Ommaviy degelmintizatsiya maktabga borishga ijobiy ta'sir ko'rsatishi ta'kidlandi.[16] Ammo muntazam ravishda olib borilgan tadqiqotlar shuni ko'rsatdiki, ommaviy degelmintizatsiya olib boradigan bolalarda davomatning yo'qligi yoki farqi yo'q.[80] Bir tadqiqot shuni ko'rsatdiki, o'g'il bolalar boshlang'ich maktabda bunday dasturlarni taklif qilmaydigan maktablarda o'qiyotgan bolalarga qaraganda ko'proq yillar davomida o'qishgan. Xuddi shu tadqiqotda qatnashgan qizlar, agar ular davolanadigan bo'lsa, o'rta maktabda tahminan to'rtdan bir qismi ko'proq edi. Ikkala guruh ham mehnat bozorining malakali sohalarida ishtirok etishdi. Maktab dasturlaridan kelib chiqadigan iqtisodiy o'sish dasturning haqiqiy xarajatlarini muvozanatlashtirishi mumkin.[81] Ammo ushbu tadqiqot natijalari bahsli (masalan, tadqiqotda tarafkashlik xavfi yuqori bo'lganligi sababli) va ommaviy gelmintizatsiya qilishning uzoq muddatli ijobiy natijalari noma'lum bo'lib qolmoqda.[80]
E'tiborsizlik sabablari
Ushbu kasalliklar e'tibordan chetda qoldi, chunki ular asosan eng qashshoq mamlakatlarga ta'sir qiladi rivojlanayotgan dunyo va so'nggi paytlarda tarqalish darajasini pasaytirishga urg'u berganligi sababli OIV / OITS, sil kasalligi va bezgak.[15] "Katta uchlik" kasalliklariga ko'proq resurslar berilgan (OIV / OITS, bezgak va sil kasalligi ) o'lim darajasi va aholining xabardorlik darajasi yuqori bo'lganligi sababli. E'tiborsiz qoldirilgan tropik kasalliklar sababni qo'llab-quvvatlovchi taniqli madaniyat arbobiga ega emas.[82][83]
E'tiborsiz qoldirilgan tropik kasalliklarning ahamiyati past baholangan, chunki ko'pchilik asemptomatik bo'lib, uzoq vaqtdan beri mavjud inkubatsiya davrlari. Uzoq vaqt davomida yashirin bo'lgan o'lim va e'tiborsiz qoldirilgan tropik kasallik o'rtasidagi bog'liqlik tez-tez amalga oshirilmaydi.[16] Yuqori darajadagi yuqumli hududlar ko'pincha geografik jihatdan ajratilgan hududlarda joylashgan bo'lib, davolash va oldini olish ancha qiyinlashadi.[82]
Stigma
Bundan tashqari, e'tiborsiz qoldirilgan tropik kasalliklar ko'pincha ijtimoiy stigma bilan bog'liq bo'lib, ularni davolash yanada murakkablashadi. Sog'liqni saqlash sohasidagi tadqiqotlar yaqinda ushbu masalaning tarkibiy qismi sifatida stigmaga e'tibor berishni boshladi. 1960-yillardan boshlab, ijtimoiy stigma bilan bog'liq har yili taxminan bir marta keltiriladi. 2006 yilda ularning soni 458 edi.[76] Kasalliklarni nazorat qilish ushbu tamg'adan katta ta'sir ko'rsatadi, chunki u yordam izlash va davolanishga rioya qilishni kamaytiradi.[84] Kasalliklarni nazorat qilish dasturlari, 1980-yillarning boshidan boshlab, stigma yumshatishni o'zlarining takliflariga qo'shishni boshladilar. Hindistonda moxov dasturi juda ta'sirlangan jamoalarda optimizmni kuchaytirish uchun "moxov irsiy emas, davolanishi mumkin" degan xabarni birinchi o'ringa qo'ydi. Maqsad moxovni "boshqalar singari" kasallikka aylantirish edi, shunda isnodni kamaytirish. Shu bilan birga, berilgan davolanadigan va'dani bajarish uchun hududda mavjud bo'lgan tibbiy resurslar optimallashtirildi.[76]
Iqtisodiy rag'batlantirish
Ushbu kasalliklarni e'tiborsiz qoldirishining bir sababi shundaki, ular tijorat emas, natijada patentlar va foyda innovatsiyalarni rag'batlantirishda hech qanday rol o'ynamaydi. Barcha notijorat sohalar singari, bu kasalliklar ham hukumatlar va xayriya ishlari (shu jumladan sanoat xayriya) uchun javobgardir.[85] Hozirgi kunda farmatsevtika sanoatining qarashlari tadqiqot va rivojlantirish juda xavfli. Shu sababli, resurslar ko'pincha NTDlar sohasiga kiritilmaydi (kambag'allarning kasalliklari kabi) va yangi kimyoviy mahsulotlar ko'pincha qimmatga tushadi. Davlat va xususiy tashabbuslarni o'rganish natijasida 1975 va 1999 yillarda sotilgan 1393 ta yangi kimyoviy mahsulotlarning atigi 16 tasi tropik kasalliklar va silga tegishli ekanligi aniqlandi. Xuddi shu tekshiruv qo'shimcha ravishda, NTDga qaraganda, markazga asab tizimining buzilishi va saraton kasalligiga chalingan preparatning bozorga kirish ehtimoli 13 baravar katta ekanligini aniqladi.[86]
Farmatsevtika sanoatida rag'bat yo'qligi sababli, NTDni muvaffaqiyatli davolash dasturlari ko'pincha xayr-ehson formatiga tayanadi. Mectizan donorlik dasturi 1,8 milliarddan ziyod ivermektin tabletkalarini xayriya qildi.[87] Ko'pincha rivojlangan davlatlar bunday loyihalarni moliyalashtirishda hukumat va xususiy sheriklik aloqalariga tayanadigan bo'lishsa, rivojlanayotgan davlatlar ushbu kasalliklarga sarflanadigan mablag'larning yiliga boshiga sezilarli darajada past bo'lishadi.[86]
2006 yilgi hisobotda Geyts Jamg'armasi ushbu kasalliklarga qarshi kurashish uchun qo'shimcha tadbirlarni moliyalashtirganligi aniqlandi.[88][89]
Rivojlangan xalqlar
2008 yildan beri beparvo qilingan qashshoqlik kasalliklari ishlab chiqilgan va o'rganilgan.[90] Ushbu guruh e'tiborga olinmagan tropik kasalliklar bilan bir-birini qoplaydi, ular rivojlangan mamlakatlarda ham inson salomatligiga xavf tug'diradi. In Qo'shma Shtatlar faqatgina parazitar yuqumli kasalliklarga chalingan kamida 12 million odam bor.[90] Ular eng kambag'al boy jamiyatlar orasida yashirin kasallik yukini tashkil qiladi.[8] Rivojlangan mamlakatlarda sog'liqni saqlash sohasidagi bilimlarning etishmasligi va yakuniy diagnostika testlarining yo'qligi ushbu kasallik guruhini e'tiborsiz qoldiradi.[91]
Qo'shma Shtatlarda parazitar yuqtirishning yuqori darajasi geografik, irqiy va ijtimoiy-iqtisodiy yo'nalishlar bo'yicha taqsimlanishi mumkin. Afro-amerikaliklar jamoasida 2,8 milliongacha holatlar bo'lishi mumkin toksokaroz. Toksokaroz kasalligi, trichomoniasis, va boshqa beparvo qilingan infektsiyalar Qo'shma Shtatlarda Nigeriyada bo'lgani kabi sodir bo'ladi. Ispan hamjamiyati tarkibida beparvo qilingan yuqumli kasalliklar AQSh-Meksika chegarasi yaqinida joylashgan. Vektor orqali yuqadigan kasalliklar, ayniqsa, Lotin Amerikasidagi kasalliklarga yaqinlashadi. Chagas kasalligi AQShda 1970-yillarda topilgan.[92] Biroq, rivojlangan mamlakatlarda qashshoqlik bilan bog'liq bo'lgan kasalliklar ko'pincha kompleks ravishda ko'rib chiqilmaydi. This may be due to lack of economic incentives and public policy failings. Here, a lack of awareness prevents effective policy generation and leaves health care services unequipped to address the issue. Additionally, there is little effort put into taking and maintaining large data sets on neglected disease in the United States and other developed nations. The first summit on the issue was held by the Adler Institute on Social Exclusion in the United States in 2009.[8]
In Europe, a similar trend is seen. Neglected tropical diseases are concentrated in eastern and southern Europe, where poverty levels are the highest. The most prevalent diseases in this region are ascariasis, trikuriyaz, zoonotik gelmint infektsiyalari, and visceral leyshmanioz. Migration paths to Europe, most notably to Spain, have brought diseases to Europe as well. As many as 6,000 cases of Chagas disease have been introduced via this method. In response to a growing awareness to the burden on these populations, the Evropa kasalliklarini oldini olish va nazorat qilish markazi has laid out ten public health guidelines. They cover a variety of topics, from health education and promotion to community partnerships and the development of a minority healthcare workforce.[8]
Oldini olish

Prevention and eradication are important because "of the appalling stigma, disfigurement, blindness and disabilities caused by NTDs."[16] The possibility of eliminating or eradicating drakunkulyaz, moxov, lymphatic filariasis, onchocerciasis, traxoma, uyqu kasalligi, visseral leyshmanioz, and canine quturish within the next ten years was the principal aim of the E'tiborsiz qoldirilgan tropik kasalliklar to'g'risida London deklaratsiyasi, which is a collaborative effort involving the WHO, the Jahon banki, the Bill & Melinda Gates Foundation, the world's 13 leading pharmaceutical companies, and government representatives from US, UK, United Arab Emirates, Bangladesh, Brazil, Mozambique and Tanzania. It was launched in January 2012.[2]
While the current era has had a noticeable uptick in biological research into neglected tropical diseases, prevention may be supplemented by social and development outreach. Spiegal and his coauthors advocated for this to take the form of "social offset." Social offset entails the delegation of some of the funding for biotechnological research to social programs. The attempts to alleviate some of the surrounding factors (such as poverty, poor sanitation, overcrowding, poor healthcare etc.) that greatly exacerbate the conditions brought on by neglected tropical diseases. Projects such as these also strengthen the goal of sustained eliminations, rather than quickly addressing symptoms.[93]
Siyosiy tashabbuslar
There are many prevention and eradication campaigns funded for example by the World Health Organization, US Agency for International Development, Bill va Melinda Geyts fondi, Buyuk Britaniya Xalqaro rivojlanish bo'limi.[16]
WHO Roadmap of 2012
WHO published in 2012 the NTD "roadmap" which contains milestones for 2015 and 2020 and which specifies targets for eradication, elimination, and intensified control of the different NTDs.[94] Masalan:
- NTDs planned to be eradicated: dracunculiasis (by the year 2015), endemic treponematoses (yaws) (by 2020)
- NTDs planned to be eliminated globally by 2020: blinding trachoma, moxov, human African trypanosomiasis, lymphatic filariasis
- NTDs planned to be eliminated in certain regions: rabies (by 2015 in Latin America, by 2020 in Southeast Asia and western Pacific regions), Chagas kasalligi (transmission through blood transfusion by 2015, intra-domiciliary transmission by 2020 in the region of the Americas), visceral leishmaniasis (by 2020 in the Indian subcontinent), oncocerciasis (by 2015 in Latin America), schistosomiasis (by 2015 in eastern Mediterranean region, Caribbean, Indonesia and the Mekong River basin, by 2020 in the region of the Americas and western Pacific region)
- NTDs planned to be eliminated in certain countries: human African trypanosomiasis (by 2015 in 80 percent of areas in which it occurs), oncocerciasis (by 2015 in Yemen, by 2020 in selected countries in Africa), schistosomiasis (by 2020 in selected countries in Africa)
- Intensified control with specific targets for the years 2015 and 2020 are provided for these NTDs: dengue, buruli yarasi, cutaneous leishmaniasis, taeniaz /sistiserkoz va echinococcosis /hydatidosis, foodborne tremadode infections, soil-transmitted helmintheases
Boshqalar
AQSh Oziq-ovqat va dori-darmonlarni boshqarish ustuvor ko'rib chiqish voucher is an incentive for companies to invest in new drugs and vaccines for tropical diseases. A provision of the Food and Drug Administration Amendments Act (HR 3580) awards a transferable "priority review voucher" to any company that obtains approval for a treatment for one of the listed diseases. The voucher can later be used to accelerate review of an unrelated drug. This program is for all tropical diseases and includes medicines for malaria and tuberculosis. The first voucher given was for Koartem, a malaria treatment.[95] It does not use or define the term "neglected" though most of the diseases listed are often included on lists of neglected diseases.
The prize was proposed by Dyuk universiteti faculty Henry Grabowski, Jeffrey Moe, and David Ridley in their 2006 Sog'liqni saqlash ishlari paper: "Developing Drugs for Developing Countries."[96] In 2007 United States Senators Sem Braunbek (R-KS) and Sherrod Braun (D-OH) sponsored an amendment to the Oziq-ovqat va dori-darmonlarni boshqarish Amendments Act of 2007. President Jorj V.Bush signed the bill in September 2007.
Integration with WASH programs
Water, sanitation, and hygiene (YUVISH ) interventions are essential in preventing many NTDs, for example tuproqdan yuqadigan gelmintoz.[97] Mass drug administrations alone will not protect people from re-infection. A more holistic and integrated approach to NTDs and WASH efforts will benefit both sectors along with the communities they are aiming to serve. This is especially true in areas that are endemic with more than one NTD.[97]
In August 2015 the World Health Organization unveiled a global strategy and action plan to integrate WASH with other xalq salomatligi interventions in order to accelerate elimination of NTDs.[98] The plan aims to intensify control or eliminate certain NTDs in specific regions by 2020 and refers to the NTD "roadmap" milestones from 2012 that include for example eradication of dracunculiasis by 2015 and of yaws by 2020, elimination of trachoma and lymphatic filariasis as public health problems by 2020, intensified control of dengue, schistosomiasis and soil-transmitted helminthiases.[91]
A closer collaboration between WASH and NTD programmes can lead to synergies. They can be achieved through collaborative planning, delivery and evaluation of programmes, strengthening and sharing of evidence, and using monitoring tools to improve the equity of health services.[99]
Reasons why WASH plays an important role in NTD prevention and patient care include:[91]
- NTDs affect more than one billion people in 149 countries. They occur mainly in regions with a lack of basic sanitation. About 2.4 billion people worldwide do not have adequate sanitation facilities. 663 million do not have access to improved drinking water sources.[100]
- One leading cause of preventable blindness is traxoma. The bacterial infection is transmitted through contact with eye-seeking flies, fingers, and fomites. Prevention components are facial cleanliness, which requires water for face washing, and environmental improvement, which includes safe disposal of excreta to reduce fly populations.[101]
- Sanitariya holati yaxshilandi prevents soil-transmitted helminthiases. It impedes fecal pathogens such as intestinal worm eggs from contaminating the environment and infecting people through contaminated food, water, dirty hands, and direct skin contact with the soil.[102]
- Sanitariya holati yaxshilandi and water management can contribute to reduce proliferation of mosquitoes that transmit diseases, such as lymphatic filariasis, denge va chikungunya. Breeding of the Culex mosquito which transmits filarial parasites is facilitated through poorly constructed latrines. Breeding of the Aedes aegypti va Aedes albopictus mosquitoes which transmit dengue and chikungunya can be prevented through safe storage of water.[103]
- Najas va siydik that contain worm eggs can contaminate surface water and lead to transmission of shistozomiya. This can be prevented through improved sanitation. Not only human but also animal (cow, buffalo) urine or feces can transmit some schistosome species. Therefore, it is important to protect freshwater from animals and animal waste.[104]
- Treatment of many NTDs require clean water and hygienic conditions for healthcare facilities and households. Uchun Gvineya qurti, Buruli yarasi, yoki cutaneous leishmaniasis, wound management is needed to speed up healing and reduce disability. Lenfatik filariaz causes chronic disabilities. People who suffer from this disease need to maintain rigorous personal hygiene with water and soap to prevent secondary infections.[105]
- NTDs that lead to permanent nogironlik make tasks such as carrying water long distances or accessing toilets difficult. However, people affected by these diseases often face isnod and can be excluded from accessing water and sanitation facilities. This increases their risk of poverty and severe illness. Clean water and soap are essential for these groups to maintain personal hygiene and dignity. Therefore, additional efforts to reduce stigma and exclusion are needed. In this manner, WASH can improve quality of life of people affected by NTDs.[106]
- A meta-tahlil safe water was associated with significantly reduced odds of Shistosoma infection, and adequate sanitation was associated with significantly lower odds of infection with both S. mansoni va S. haematobium.[107]
- A systematic ko'rib chiqish and meta-analysis showed that better hygiene in children is associated with lower odds of trachoma. Access to sanitation was associated with 15 percent lower odds of active traxoma and 33 percent lower odds of C. trachomatis infection of the eyes.[108]
- Another systematic review and meta-analysis found a correlation between WASH access and practices and lower odds of tuproqdan yuqadigan gelmintoz infections by 33 to 77 percent. Shaxslar washed their hands keyin defekatsiya were less than half as likely to be infected as those who did not.[109] An'anaga ko'ra, preventive chemotherapy is used as a measure of control, although this measure does not stop the transmission cycle and cannot prevent reinfection. In contrast, improved sanitation can.[110]
Pharmaceutical market
Biotexnologiya companies in the developing world have targeted neglected tropical diseases due to need to improve global health.[111]
Dori vositalarini ommaviy boshqarish is considered a possible method for eradication, especially for lymphatic filariasis, onchocerciasis, and trachoma, although drug resistance is a potential problem.[112] According to Fenwick, Pfizer donated 70 million doses of drugs in 2011 to eliminate trachoma through the International Trachoma Initiative.[16] Merck has helped The African Programme for the Control of Onchocerciasis (APOC) and Oncho Elimination Programme for the Americas to greatly diminished the effect of onchocerciasis by donating ivermektin.[16] Merck KGaA pledged to give 200 million tablets of praziquantel over 10 years, the only cure for shistozomiya.[113] GlaxoSmithKline has donated two billion tablets of medicine for lymphatic filariasis and pledged 400 million deworming tablets per year for five years in 2010. Jonson va Jonson has pledged 200 million deworming tablets per year.[16] Novartis has pledged leprosy treatment, EISAI pledged two billion tablets to help treat lymphatic filariasis.[16]
NGO initiatives
There are currently only two donor-funded nodavlat tashkilotlar that focus exclusively on NTDs:[114] The Schistosomiasis Control Initiative and Deworm the World. Despite under-funding, many neglected diseases are cost-effective to treat and prevent. The cost of treating a child for infection of soil transmitted helminths and schistosomes (some of the main causes of neglected diseases), is less than US$0.50 per year, when administered as part of school-based mass deworming by Deworm the World. This programme is recommended by Biz qo'limizdan kelganini berish va Copenhagen Consensus Centre as one of the most efficient and cost-effective solutions. Sa'y-harakatlari Schistosomiasis Control Initiative to combat neglected diseases include the use of rapid-impact packages: supplying schools with packages including four or five drugs, and training teachers in how to administer them.
Health Action International based in Amsterdam worked with the WHO to get snakebite envenoming on the list of neglected tropical diseases.[115]
Public-private initiatives
An alternative model to the profit-driven drug development emerged in the years 2000 to provide an answer to the needs of these neglected patients. Product development partnerships (PDPs) aim at implementing and accelerating the research and development (R&D) of safe and effective health tools (diagnostics, vaccines, drugs) to notably combat diseases that are neglected.[116] Drugs for Neglected Disease initiative (DNDi) is one of these PDPs that has already developed new treatments for NTDs[117]
The Sabin Vaccine Institute, founded in 1993, works to address the issues of vaccine-preventable diseases as well as NTDs. They run three main programs, Sabin Vaccine Development, E'tiborsiz qolgan tropik kasalliklar uchun global tarmoq, and Vaccine Advocacy and Education.[118] Their product development partnership affiliates them with the Texas bolalar kasalxonasi shuningdek Baylor Tibbiyot kolleji. Their major campaign, End7, aims to end seven of the most common NTDs (fil, river blindness, salyangoz isitmasi, traxoma, yumaloq qurt, qamchi qurti va ankilomit ) by 2020. Through End7, college campuses undertake fundraising and educational initiatives for the broader goals of the campaign.[119]
WIPO Re:Search was established in 2011 by the Jahon intellektual mulk tashkiloti in collaboration with BIO Ventures for Global Health (BVGH) and with the active participation of leading pharmaceutical companies and other private and public sector research organizations. It allows organizations to share their intellectual property, compounds, expertise, facilities and know-how royalty-free with qualified researchers worldwide working on new solutions for NTDs, malaria and tuberculosis.[120][121]
In 2013, the Government of Japan, five Japanese pharmaceutical companies, the Bill and Melinda Gates Foundation, and the UNDP established a new public-private partnership, Global Health Innovative Technology Fund. They pledged over US$100 million to the fund over five years, to be awarded as grants to R&D partnerships across sectors in Japan and elsewhere, working to develop new drugs and vaccines for 17 neglected diseases, in addition to HIV, malaria and tuberculosis.[122][123][124] Affordability of the resulting drugs and vaccines is one of the key criteria for grant awards.[122]
Boshqalar
An ochiq jurnal dedicated to neglected tropical diseases called PLoS Neglected Tropical Diseases first began publication in 2007.
One of the first large-scale initiatives to address NTDs came from a collaboration between Kenneth Warren and the Rokfeller jamg'armasi. Ken Warren is regarded as one of the founding figures in neglected tropical disease research. The Great Neglected Tropical Diseases Network was a consortium of scientists from all over the world, hand picked by Ken Warren, working to expand the research base in neglected diseases. Many of the scientists that he recruited had not been involved in NTD research before. The network ran from 1978 to 1988. Warren's vision was to establish units within biological labs across the world, dedicated to Ilmiy-tadqiqot ishlari. By forming a critical mass of scientists in NTD research, he hoped to attract new students into the field. The interdisciplinary group met annually to update the community on research progress. Much of the work done by this group focused on the understanding of the mechanisms behind infection. At these informally structured meetings, research partnerships were formed. Warren himself encouraged these partnerships, especially if they bridged the divide between developed and developing nations. Through the Great Neglected Tropical Disease Network, a great number of scientists were brought into the field of parazitologiya.[125]
Epidemiologiya
The distribution of neglected tropical disease disproportionally affects about one billion of the world's poorest populations[126] causing mortality, disability, and morbidity.[127] Lack of funding, resources, and attention can result in treatable and preventable diseases causing death.[128] Factors like political dynamics, poverty, and geographical conditions can make the delivery of NTD control programs difficult.[126] Intersectional collaboration of poverty reduction policies and neglected tropical diseases creates cross-sector approaches to simultaneously address these issues.[126]
The six most common NTDs include tuproqdan yuqadigan gelmintlar (STHs)—specifically roundworm (Ascaris lumbricoides), qamchi (Trichuris trichiura) and hookworms (Nekator amerikan va Ankilostoma o'n ikki barmoqli ichak)—schistosomiasis, trachoma, and lymphatic filariasis (LF).[97] These diseases affect one-sixth of the world's population with 90 percent of the disease burden occurring in sub-Saharan Africa.[97]
Information on the frequency of neglected tropical diseases is of low quality. It is currently difficult to summarize all of the information on this family of diseases. One effort to do so is the Global Burden of Disease framework. It aims to create a standardized method of measurement. The principle components of the approach involve 1) the measuring of premature mortality as well as disability, 2) the standardized usage of DALYs (nogironlik bo'yicha tuzatilgan hayot yillari ), and 3) wide spread inclusion of diseases and injury causes with the estimation of missing data.[129] However, the DALY has been criticized as a 'systematic undervaluation' of disease burden. Qirol [130] asserts that the DALY emphasizes the individual too much, while ignoring the effects of the ecology of the disease. In order for the measure to become more valid, it may have to take the context of poverty more into account. King also emphasizes that DALYs may not capture the non-linear effects of poverty on cost-utility analysis of disease control. The Socio-Demographic Index (SDI) and Healthy Life Expectancy (HALE) are other summary measures that can be used to take into account other factors.[131] HALE is a metric that weights years lived and health loss before death to provides a summary of population health.[132] SDI is a measurement that includes lag-distributed income per capita, average education, and fertility rate.[133] Socioeconomic factors greatly influence the distribution of neglected tropical diseases, and not addressing these factors in models and measurements can lead to ineffective public health policy.[128]
Tarix
In 1977 an American research invented the concept of what is now "neglected tropical diseases".[134]
Shuningdek qarang
- Yuqumli kasallik
- Najas-og'iz orqali yuborish
- Neglected Tropical Disease Research and Development
- Drugs for Neglected Diseases Initiative
- Yuqumli kasalliklarni yo'q qilish
- E'tiborsiz qolgan tropik kasalliklar uchun global tarmoq
- Etim kasalliklari
Adabiyotlar
- ^ Hotez PJ, Aksoy S, Brindley PJ, Kamhawi S (January 2020). "What constitutes a neglected tropical disease?". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 14 (1): e0008001. doi:10.1371/journal.pntd.0008001. PMC 6991948. PMID 31999732.
- ^ a b v Hotez PJ (November 2013). "NTDs V.2.0: "blue marble health"--neglected tropical disease control and elimination in a shifting health policy landscape". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 7 (11): e2570. doi:10.1371/journal.pntd.0002570. PMC 3836998. PMID 24278496.

- ^ Hotez PJ, Kamath A (August 2009). Cappello M (ed.). "Neglected tropical diseases in sub-saharan Africa: review of their prevalence, distribution, and disease burden". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 3 (8): e412. doi:10.1371 / journal.pntd.0000412. PMC 2727001. PMID 19707588.

- ^ Mike Shanahan (31 January 2006). "Beat neglected diseases to fight HIV, TB and malaria". SciDev.Net. Arxivlandi from the original on 19 May 2006.
- ^ "Making the Case to Fight Schistosomiasis". Milliy jamoat radiosi. Arxivlandi from the original on 10 October 2008. Olingan 1 dekabr 2008.
- ^ Hotez PJ (January 2010). "A plan to defeat neglected tropical diseases". Ilmiy Amerika. 302 (1): 90–4, 96. Bibcode:2010SciAm.302a..90H. doi:10.1038/scientificamerican0110-90. PMID 20063641. Arxivlandi from the original on 6 August 2014.
- ^ Reddy M, Gill SS, Kalkar SR, Vu V, Anderson PJ, Rochon PA (oktyabr 2007). "Ko'plab e'tibordan chetda qolgan tropik kasalliklar uchun og'iz dori terapiyasi: tizimli ko'rib chiqish". JAMA. 298 (16): 1911–24. doi:10.1001 / jama.298.16.1911. PMID 17954542.
- ^ a b v d Hotez P (1 November 2009). "Neglected diseases amid wealth in the United States and Europe". Sog'liqni saqlash ishlari. 28 (6): 1720–5. doi:10.1377/hlthaff.28.6.1720. PMID 19887412.
- ^ "Research Publications | Poverty Solutions at The University of Michigan". www.npc.umich.edu. Arxivlandi from the original on 23 July 2017. Olingan 16 yanvar 2018.
- ^ Hotez PJ (September 2012). "Fighting neglected tropical diseases in the southern United States" (PDF). BMJ. 345: e6112. doi:10.1136/bmj.e6112. PMID 22977143. S2CID 22530671. Arxivlandi (PDF) asl nusxasidan 2017 yil 10 mayda.
- ^ "Jahon Sog'liqni saqlash tashkiloti". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2014 yil 22 fevralda. Olingan 18 iyun 2017.
- ^ "DNDi – Best Science for the Most Neglected". www.dndi.org. Arxivlandi from the original on 13 March 2018. Olingan 5 may 2018.
- ^ a b "Jahon Sog'liqni saqlash tashkiloti". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2017 yil 20 oktyabrda. Olingan 5 may 2018.
- ^ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lanset. 385 (9963): 117–71. doi:10.1016 / S0140-6736 (14) 61682-2. PMC 4340604. PMID 25530442.
- ^ a b v d e f g h men j k l m Feasey N, Wansbrough-Jones M, Mabey DC, Solomon AW (2010). "Neglected tropical diseases". Britaniya tibbiyot byulleteni. 93 (1): 179–200. doi:10.1093/bmb/ldp046. PMID 20007668. Arxivlandi from the original on 14 February 2016.
- ^ a b v d e f g h men j k l m n o p q r s Fenvik A (2012 yil mart). "The global burden of neglected tropical diseases". Xalq salomatligi. 126 (3): 233–236. doi:10.1016 / j.puhe.2011.11.015. PMID 22325616.
- ^ "Neglected tropical diseases". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2014 yil 22 fevralda. Olingan 24-noyabr 2015.
- ^ "Jahon Sog'liqni saqlash tashkiloti". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2014 yil 22 fevralda. Olingan 30 oktyabr 2016.
- ^ "CDC – Neglected Tropical Diseases – Diseases". www.cdc.gov. Arxivlandi asl nusxasidan 2014 yil 4 dekabrda. Olingan 30 oktyabr 2016.
- ^ "PLoS Neglected Tropical Diseases: A Peer-Reviewed Open-Access Journal". journals.plos.org. Arxivlandi from the original on 14 November 2020. Olingan 19 noyabr 2020.
- ^ a b "Buruli Ulcer". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2016 yil 11 mayda. Olingan 2 may 2016.
- ^ a b "Buruli Ulcer". Arxivlandi asl nusxasidan 2014 yil 13 aprelda. Olingan 12 mart 2014.
- ^ "Buruli Ulcer Endemic Countries". Arxivlandi asl nusxasidan 2014 yil 12 martda. Olingan 12 mart 2014.
- ^ a b v d e f g "Chagas disease (American trypanosomiasis)". Arxivlandi asl nusxasidan 2014 yil 13 martda. Olingan 12 mart 2014.
- ^ a b v d e "World Health Day 2014: small bite, big threat". Arxivlandi asl nusxasidan 2014 yil 27 fevralda. Olingan 12 mart 2014.
- ^ a b v d e f "Dengue Control". Arxivlandi asl nusxasidan 2014 yil 12 martda. Olingan 12 mart 2014.
- ^ a b v Pialoux G, Gaüzère BA, Jauréguiberry S, Strobel M (May 2007). "Chikungunya, an epidemic arbovirosis". Lanset. Yuqumli kasalliklar. 7 (5): 319–27. doi:10.1016/S1473-3099(07)70107-X. PMID 17448935.
- ^ "Symptoms, Diagnosis, & Treatment | Chikungunya virus | CDC". www.cdc.gov. 17 dekabr 2018 yil. Olingan 17 mart 2020.
- ^ Chikungunya, JSSV, arxivlandi asl nusxasidan 2016 yil 20 yanvarda, olingan 21 yanvar 2016
- ^ "Dunyo bo'ylab Gvineyada qurtlarni yuqtirish bo'yicha so'nggi holatlarni ko'rib chiqing". www.cartercenter.org. Olingan 28 fevral 2020.
- ^ "Dracunculiasis eradication - global surveillance summary, 2009" (PDF). Tegishli Épidémiologique Hebdomadaire. 85 (19): 166–76. 2010 yil may. PMID 20449943. Arxivlandi (PDF) asl nusxasidan 2016 yil 3 martda.
- ^ a b v d e f "Dracunculiasis". Arxivlandi from the original on 5 April 2014. Olingan 13 mart 2014.
- ^ "Echinococcosis". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ a b v "Signs, symptoms and treatment of echinococcosis". Arxivlandi asl nusxasi 2015 yil 24 mayda. Olingan 16 mart 2014.
- ^ a b "Transmission of echinococcosis". Arxivlandi asl nusxasi 2015 yil 5-iyunda. Olingan 16 mart 2014.
- ^ a b "Surveillance, prevention and control of echinococcosis". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ a b v d e f "Yaws". Arxivlandi from the original on 15 March 2014. Olingan 16 mart 2014.
- ^ "Foodborne trematode infections". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi from the original on 25 November 2015. Olingan 24-noyabr 2015.
- ^ "Human African Trypanosomiasis: number of new cases falls to historical low in 50 years". Arxivlandi asl nusxasidan 2013 yil 25 oktyabrda.
- ^ a b "Burden and Distribution". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ "Leishmaniasis". Arxivlandi from the original on 15 March 2014. Olingan 16 mart 2014.
- ^ "Diagnosis, detection and surveillance". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ "Access to essential antileishmanial medicines and treatment". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ "WHO | Leprosy: New data show steady decline in new cases".
- ^ a b "Leprosy Today". Arxivlandi asl nusxasidan 2014 yil 14 martda. Olingan 16 mart 2014.
- ^ a b "Leprosy: the disease". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ a b "Leprosy". Arxivlandi asl nusxasidan 2010 yil 9 fevralda.
- ^ a b "Epidemiologiya". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ a b "Forms of Lymphatic Filariasis and diagnosis". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ a b "Lenfatik filariaz". Arxivlandi asl nusxasidan 2014 yil 30 martda. Olingan 16 mart 2014.
- ^ Mohammed KA, Haji HJ, Gabrielli AF, Mubila L, Biswas G, Chitsulo L, et al. (2008 yil yanvar). Utzinger J (ed.). "Triple co-administration of ivermectin, albendazole and praziquantel in zanzibar: a safety study". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 2 (1): e171. doi:10.1371/journal.pntd.0000171. PMC 2217668. PMID 18235853.

- ^ "Clinical manifestations". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ "Onchocerciasis (River blindness)".
- ^ a b v d "Onchocerciasis". Arxivlandi from the original on 16 March 2014. Olingan 16 mart 2014.
- ^ a b v "Onchocerciasis". Arxivlandi asl nusxasidan 2014 yil 9 aprelda. Olingan 16 mart 2014.
- ^ a b "Quturganlar". Arxivlandi asl nusxasidan 2014 yil 24 fevralda. Olingan 16 mart 2014.
- ^ a b v d e "About rabies". Arxivlandi from the original on 30 January 2014. Olingan 16 mart 2014.
- ^ a b "Quturganlar". Arxivlandi asl nusxasidan 2014 yil 1 aprelda. Olingan 16 mart 2014.
- ^ "Schistosomiasis-Disease". CDC, Division of Parasitic Diseases. Arxivlandi asl nusxasidan 2016 yil 2 dekabrda. Olingan 17 oktyabr 2016.
- ^ a b v d e f g h men "Soil-transmitted helminth infections". Arxivlandi asl nusxasidan 2014 yil 21 fevralda. Olingan 16 mart 2014.
- ^ a b "Transmission of taeniasis/cysticercosis". Arxivlandi asl nusxasidan 2014 yil 14 martda. Olingan 13 mart 2014.
- ^ a b v "About Taeniasis/cysticercosis". Arxivlandi asl nusxasidan 2014 yil 14 martda. Olingan 13 mart 2014.
- ^ a b v "Signs, symptoms and treatment of taeniasis/cysticercosis". Arxivlandi asl nusxasidan 2014 yil 14 martda. Olingan 13 mart 2014.
- ^ "Surveillance, prevention and control of taeniasis/cysticercosis". Arxivlandi asl nusxasidan 2014 yil 14 martda. Olingan 13 mart 2014.
- ^ a b v d e "Priority eye diseases". Arxivlandi from the original on 26 July 2014. Olingan 16 mart 2014.
- ^ "Snakebite finally makes a WHO list of top global health priorities". STAT. 12 June 2017. Arxivlandi from the original on 13 June 2017. Olingan 18 iyun 2017.
- ^ Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. (2008 yil noyabr). "Ilon chaqishning global yuki: kelayotgan va o'lganlarning mintaqaviy taxminlariga asoslangan adabiyotni tahlil qilish va modellashtirish". PLOS tibbiyoti. 5 (11): e218. doi:10.1371 / journal.pmed.0050218. PMC 2577696. PMID 18986210.
- ^ a b Taylor-Robinson, David C.; Maayan, Nikola; Donegan, Sarah; Chaplin, Marty; Garner, Paul (11 September 2019). "Public health deworming programmes for soil-transmitted helminths in children living in endemic areas". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 9: CD000371. doi:10.1002/14651858.CD000371.pub7. ISSN 1469-493X. PMC 6737502. PMID 31508807.
- ^ Lindoso JA, Lima AC, Cunha MA, Gomes CM (23 August 2015). "Diagnosing Neglected Tropical Diseases in HIV Coinfection". Human Parasitic Diseases. 2015 (7): 11–18. doi:10.4137/HPD.S19569. Arxivlandi asl nusxasidan 2016 yil 17 noyabrda.
- ^ a b v d Singer M, Bulled N (November 2012). "Interlocked Infections: The Health Burdens of Syndemics of Neglected Tropical Diseases". Annals of Anthropological Practice. 36 (2): 328–345. doi:10.1111/napa.12007.
- ^ Brady MA, Hooper PJ, Ottesen EA (July 2006). "Projected benefits from integrating NTD programs in sub-Saharan Africa". Parazitologiya tendentsiyalari. 22 (7): 285–91. doi:10.1016/j.pt.2006.05.007. PMID 16730230.
- ^ a b van den Berg H, Kelly-Hope LA, Lindsay SW (January 2013). "Malaria and lymphatic filariasis: the case for integrated vector management". Lanset. Yuqumli kasalliklar. 13 (1): 89–94. doi:10.1016/S1473-3099(12)70148-2. PMID 23084831.
- ^ a b Conteh L, Engels T, Molyneux DH (January 2010). "Socioeconomic aspects of neglected tropical diseases". Lanset. 375 (9710): 239–47. doi:10.1016/S0140-6736(09)61422-7. PMID 20109925. S2CID 20630557.
- ^ Molyneux DH (2004). ""Neglected" diseases but unrecognised successes--challenges and opportunities for infectious disease control". Lanset. 364 (9431): 380–3. doi:10.1016/S0140-6736(04)16728-7. PMID 15276399. S2CID 42273787.
- ^ "Deworm the World: the evidence for school-based deworming". Arxivlandi 2013 yil 14 yanvarda asl nusxadan.
- ^ a b v d Weiss MG (May 2008). "Stigma and the social burden of neglected tropical diseases". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 2 (5): e237. doi:10.1371/journal.pntd.0000237. PMC 2359851. PMID 18478049.

- ^ Litt E, Baker MC, Molyneux D (May 2012). "Neglected tropical diseases and mental health: a perspective on comorbidity". Parazitologiya tendentsiyalari. 28 (5): 195–201. doi:10.1016/j.pt.2012.03.001. PMID 22475459.
- ^ Kealey A, Smith? R (February 2010). "Neglected tropical diseases: infection, modeling, and control". Journal of Health Care for the Poor and Underserved. 21 (1): 53–69. doi:10.1353/hpu.0.0270. PMID 20173255. S2CID 27293058.
- ^ Rilkoff H, Tukahebwa EM, Fleming FM, Leslie J, Cole DC (2013). "Exploring gender dimensions of treatment programmes for neglected tropical diseases in Uganda". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 7 (7): e2312. doi:10.1371/journal.pntd.0002312. PMC 3708858. PMID 23875047.

- ^ a b Welch VA, Ghogomu E, Hossain A, et al. (2016). "Deworming and Adjuvant Interventions for Improving the Developmental Health and Well-being of Children in Low- and Middle-income Countries: A Systematic Review and Network Meta-analysis" (PDF). Kempbellning muntazam sharhlari. 12: 1–383. doi:10.4073/csr.2016.7. Arxivlandi (PDF) from the original on 26 March 2017.
- ^ "Worms at Work: Long-Run Impacts of a Child Health investment". Arxivlandi asl nusxasidan 2016 yil 28 oktyabrda. Olingan 28 oktyabr 2016.
- ^ a b Hotez P, Ottesen E, Fenwick A, Molyneux D (1 January 2006). "The neglected tropical diseases: the ancient afflictions of stigma and poverty and the prospects for their control and elimination". Eksperimental tibbiyot va biologiyaning yutuqlari. 582: 23–33. doi:10.1007/0-387-33026-7_3. ISBN 978-0-387-31783-0. PMID 16802616.
- ^ Payne L, Fitchett JR (September 2010). "Bringing neglected tropical diseases into the spotlight". Parazitologiya tendentsiyalari. 26 (9): 421–3. doi:10.1016/j.pt.2010.06.002. PMID 20591739.
- ^ Weiss MG (May 2008). "Stigma and the social burden of neglected tropical diseases". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 2 (5): e237. doi:10.1371/journal.pntd.0000237. PMC 2359851. PMID 18478049.
- ^ "O'qish uchun obuna bo'ling". Financial Times. Olingan 5 may 2018.
- ^ a b Trouiller P, Olliaro P, Torreele E, Orbinski J, Laing R, Ford N (June 2002). "Drug development for neglected diseases: a deficient market and a public-health policy failure". Lanset. 359 (9324): 2188–94. doi:10.1016/S0140-6736(02)09096-7. hdl:10144/28441. PMID 12090998. S2CID 1616485.
- ^ Colatrella B (September 2008). "The Mectizan Donation Program: 20 years of successful collaboration - a retrospective". Tropik tibbiyot va parazitologiya yilnomalari. 102 Suppl 1: 7–11. doi:10.1179/136485908X337418. PMID 18718147. S2CID 32987420.
- ^ Gillis J (25 April 2006). "Cure for Neglected Diseases: Funding". Vashington Post.
- ^ Disease control priorities in developing countries (2-nashr). Oksford universiteti matbuoti. 2006 yil. ISBN 978-0-821-36179-5.
- ^ a b Hotez PJ (September 2014). "Neglected parasitic infections and poverty in the United States". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 8 (9): e3012. doi:10.1371/journal.pntd.0003012. PMC 4154650. PMID 25188455.
- ^ a b v World Health Organization (WHO) (2015): Water Sanitation and Hygiene for accelerating and sustaining progress on Neglected Tropical Diseases. A global strategy 2015 – 2020 Arxivlandi 2015 yil 25 sentyabr Orqaga qaytish mashinasi. Geneva, Switzerland, p. 26
- ^ Kirchhoff LV (August 1993). "American trypanosomiasis (Chagas' disease)--a tropical disease now in the United States". Nyu-England tibbiyot jurnali. 329 (9): 639–44. doi:10.1056/NEJM199308263290909. PMID 8341339.
- ^ Spiegel JM, Dharamsi S, Wasan KM, Yassi A, Singer B, Hotez PJ, et al. (2010 yil may). "Which new approaches to tackling neglected tropical diseases show promise?". PLOS tibbiyoti. 7 (5): e1000255. doi:10.1371/journal.pmed.1000255. PMC 2872649. PMID 20502599.
- ^ World Health Organization (WHO) (2012). Accelerating work to overcome the global impact of Neglected Tropical Diseases. A roadmap for implementation Arxivlandi 2015 yil 6-iyun kuni Orqaga qaytish mashinasi. Geneva, Switzerland.
- ^ "FDA Approves Coartem Tablets to Treat Malaria". USFDA. Arxivlandi asl nusxasidan 2009 yil 2 iyunda. Olingan 11 dekabr 2009.
- ^ Ridli DB, Grabovski HG, Moe JL (2006). "Rivojlanayotgan mamlakatlar uchun dori vositalarini yaratish". Sog'liqni saqlash ishlari. 25 (2): 313–24. doi:10.1377 / hlthaff.25.2.313. PMID 16522573.
- ^ a b v d Johnston EA, Teague J, Graham JP (June 2015). "Challenges and opportunities associated with neglected tropical disease and water, sanitation and hygiene intersectoral integration programs". BMC sog'liqni saqlash. 15 (1): 547. doi:10.1186/s12889-015-1838-7. PMC 4464235. PMID 26062691.
- ^ "WHO strengthens focus on water, sanitation, and hygiene to accelerate elimination of neglected tropical diseases". Jahon sog'liqni saqlash tashkiloti (JSST). 2015 yil 27-avgust. Arxivlandi asl nusxasidan 2015 yil 12 sentyabrda. Olingan 14 sentyabr 2015.
- ^ "Collaboration between WASH and NTD". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2016 yil 4 martda. Olingan 14 sentyabr 2015.
- ^ "NTDs and access to water and sanitation are major global challenges". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2015 yil 30 avgustda. Olingan 14 sentyabr 2015.
- ^ "Facial cleanliness and environmental improvement are key to eliminating trachoma". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2016 yil 2 aprelda. Olingan 14 sentyabr 2015.
- ^ "Sanitation prevents soil transmitted helminth infections". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2016 yil 2 aprelda. Olingan 14 sentyabr 2015.
- ^ "Breeding sites for mosquitoes are reduced through improved sanitation and water management". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi from the original on 16 June 2016. Olingan 14 sentyabr 2015.
- ^ "Protecting freshwater from contamination reduces schistosomiasis". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2016 yil 4 martda. Olingan 14 sentyabr 2015.
- ^ "Xavfsiz suv NTDlarni davolash va parvarish qilish uchun juda muhimdir". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2016 yil 4 martda. Olingan 14 sentyabr 2015.
- ^ "WASH NTDlardan zarar ko'rgan odamlarning hayot sifatini yaxshilaydi". Jahon sog'liqni saqlash tashkiloti (JSST). Arxivlandi asl nusxasidan 2016 yil 2 aprelda. Olingan 14 sentyabr 2015.
- ^ Grimes JE, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR (dekabr 2014). "Suv, sanitariya va shistosomioz o'rtasidagi o'zaro bog'liqlik: tizimli tahlil va meta-tahlil". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 8 (12): e3296. doi:10.1371 / journal.pntd.0003296. PMC 4256273. PMID 25474705.
- ^ Aktsiyalar ME, Ogden S, Haddad D, Addiss DG, McGuire C, Freeman MC (fevral 2014). "Suv, sanitariya va gigienaning traxomani oldini olishga ta'siri: tizimli tahlil va meta-tahlil". PLOS tibbiyoti. 11 (2): e1001605. doi:10.1371 / journal.pmed.1001605. PMC 3934994. PMID 24586120.
- ^ Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC (mart 2014). "Suv, sanitariya, gigiena va tuproqdan yuqadigan gelmint infektsiyasi: tizimli tahlil va meta-tahlil". PLOS tibbiyoti. 11 (3): e1001620. doi:10.1371 / journal.pmed.1001620. PMC 3965411. PMID 24667810.
- ^ Kempbell SJ, Savage GB, Grey DJ, Atkinson JA, Soares Magalhaes RJ, Neri SV va boshq. (2014 yil aprel). "Suv, sanitariya va gigiena (WASH): tuproq bilan yuqadigan barqaror gelmint va shistosomozni nazorat qilishning muhim tarkibiy qismi". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 8 (4): e2651. doi:10.1371 / journal.pntd.0002651. PMC 3983087. PMID 24722335.
- ^ Frew SE, Liu VY, Singer PA (2009). "Dunyo janubiga" beparvo qilingan kasalliklarga qarshi kurashda yordam berish uchun biznes-reja " (PDF). Sog'liqni saqlash ishlari. 28 (6): 1760–73. doi:10.1377 / hlthaff.28.6.1760. PMID 19887417. Arxivlandi (PDF) asl nusxasidan 2012 yil 20 oktyabrda.
- ^ Keenan JD, Hotez PJ, Amza A, Stoller NE, Gaynor BD, Porco TC, Lietman TM (2013). "Dori vositalarini ommaviy ravishda yuborish bilan unutilgan tropik kasalliklarni yo'q qilish va yo'q qilish: mutaxassislar so'rovi". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 7 (12): e2562. doi:10.1371 / journal.pntd.0002562. PMC 3855072. PMID 24340111.

- ^ Berns M (3 oktyabr 2010 yil). "Praziquantelni hayotdan qutqaradigan dori Afrika uchun juda qimmat". Tinch okeani standarti. Miller-Makkun tadqiqot, ommaviy axborot vositalari va jamoat siyosati markazi. Arxivlandi asl nusxasidan 2018 yil 3 fevralda. Olingan 8 dekabr 2015.
- ^ "Biz qo'limizdan kelganini berish; tavsiya etilgan tadbirlar". Arxivlandi asl nusxasidan 2014 yil 16 martda.
- ^ Cite error: Nomlangan ma'lumotnoma
2. avtomatik ishlab chiqarilganchaqirilgan, ammo hech qachon aniqlanmagan (qarang yordam sahifasi). - ^ Croft SL (oktyabr 2005). "Davlat-xususiy sheriklik: u erdan bu erga". Tropik tibbiyot va gigiena qirollik jamiyatining operatsiyalari. 99 Qo'shimcha 1: S9-14. doi:10.1016 / j.trstmh.2005.06.008. PMID 16087204.
- ^ "Qarovsiz qolgan bemorlar uchun ilmiy-tadqiqot ishlariga innovatsion yondashuv: o'n yillik tajriba va DNDi tomonidan o'rganilgan darslar". DNDi. 2014 yil yanvar
- ^ "Biz haqimizda | Sabin". www.sabin.org. Arxivlandi asl nusxasidan 2016 yil 30 oktyabrda. Olingan 28 oktyabr 2016.
- ^ "Nima uchun NTD'lar? | End7". www.end7.org. Arxivlandi asl nusxasidan 2016 yil 29 oktyabrda. Olingan 28 oktyabr 2016.
- ^ Ramamoorti R, Graef KM, Dent J (2014 yil dekabr). "BIMT Re: Izlash: sektorlararo sheriklik orqali anthelmintic rivojlanishini tezlashtirish". Xalqaro parazitologiya jurnali. Giyohvand moddalar va giyohvandlikka qarshilik. 4 (3): 220–5. doi:10.1016 / j.ijpddr.2014.09.002. PMC 4266808. PMID 25516832.
- ^ "WIPO Re: Izlash". Arxivlandi asl nusxasidan 2015 yil 28 martda. Olingan 16 mart 2015.
- ^ a b "Yaponiya sog'liqni saqlash bo'yicha global tadqiqotlarni moliyalashtirish bo'yicha kashshof hamkorlikda", Endryu Jek, Financial Times, 2013 yil 30-may
- ^ "Tachi Yamada bilan tomoshabin", Asher Mullard tomonidan, Tabiat jurnal, 2013 yil sentyabr, 12-jild, 658-bet
- ^ "Qarovsiz kasalliklarga qarshi kurashga qo'shilish", Ilm-fan jurnal, 2013 yil 7-iyun, 340-jild, p.1148
- ^ Keating C (2014 yil dekabr). "Ken Uorren va Rokfeller jamg'armasining katta e'tibordan chetda qolgan kasalliklar tarmog'i, 1978-1988 yillar: tropik va global tibbiyotning o'zgarishi". Molekulyar tibbiyot. 20 ta qo'shimcha 1 (qo'shimcha 1): S24-30. doi:10.2119 / molmed.2014.00221. PMC 4374516. PMID 25549230.
- ^ a b v Standley C, Boyce MR, Klineberg A, Essix G, Katz R (2018 yil noyabr). Remais QK (tahr.). "Sog'liqni saqlash vazirliklari tarkibida unutilgan tropik kasalliklarni kompleks nazoratini nazorat qilishni tashkil etish". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 12 (11): e0006929. doi:10.1371 / journal.pntd.0006929. PMC 6281257. PMID 30462639.
- ^ Martins-Melo FR, Karneiro M, Ramos AN, Heukelbach J, Ribeiro AL, Werneck GL (iyun 2018). Angheben A (tahrir). "Braziliyada e'tiborsiz qoldirilgan tropik kasalliklarning yuki, 1990-2016: 2016 yilgi global yuklarni o'rganish bo'yicha submilliy tahlil". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 12 (6): e0006559. doi:10.1371 / journal.pntd.0006559. PMC 6013251. PMID 29864133.
- ^ a b DebRoy S, Prosper O, Mishoe A, Mubayi A (dekabr 2017). "E'tiborsiz qoldirilgan tropik kasalliklarning murakkabligini modellashtirishdagi muammolar: resurslarning cheklangan sharoitida visseral leyshmaniozning dinamikasini ko'rib chiqish". Epidemiologiyada paydo bo'layotgan mavzular. 14 (1): 10. doi:10.1186 / s12982-017-0065-3. PMC 5604165. PMID 28936226.
- ^ Mathers CD, Ezzati M, Lopez AD (2007 yil noyabr). "Qarovsiz qoldirilgan tropik kasalliklar yukini o'lchash: kasallik doirasining global yuki". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 1 (2): e114. doi:10.1371 / journal.pntd.0000114. PMC 2100367. PMID 18060077.
- ^ King CH, Bertino AM (mart 2008). "Kambag'allikning nosimmetrikliklari: kasalliklarni baholashning global yuki nega e'tibordan chetda qolgan tropik kasalliklarning yukini kamaytiradi". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 2 (3): e209. doi:10.1371 / journal.pntd.0000209. PMC 2267491. PMID 18365036.
- ^ Pni unuting (2016 yil 14 oktyabr). "315 kasallik va shikastlanishlar va sog'lom hayot davomiyligi (HALE) uchun global, mintaqaviy va milliy nogironlikka moslashtirilgan hayot yillari (DALY) uchun 1000 baholash fakulteti, 1990-2015 yillar: kasalliklarni o'rganish global yukini 2015 yil uchun tizimli tahlil". doi:10.3410 / f.726827339.793524296. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ Pni unuting (2016 yil 14 oktyabr). "315 kasallik va shikastlanishlar va sog'lom hayot davomiyligi (HALE) uchun global, mintaqaviy va milliy nogironlikka moslashtirilgan hayot yillari (DALY) uchun 1000 baholash fakulteti, 1990-2015 yillar: kasalliklarni o'rganish global yukini 2015 yil uchun tizimli tahlil". doi:10.3410 / f.726827339.793524296. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ Martins-Melo FR, Karneiro M, Ramos AN, Heukelbach J, Ribeiro AL, Werneck GL (iyun 2018). Angheben A (tahrir). "Braziliyada e'tiborsiz qoldirilgan tropik kasalliklarning yuki, 1990-2016: 2016 yilgi global yuklarni o'rganish bo'yicha submilliy tahlil". PLOS tropik kasalliklarni e'tiborsiz qoldirdi. 12 (6): e0006559. doi:10.1371 / journal.pntd.0006559. PMC 6013251. PMID 29864133.
- ^ Keating C (2014 yil dekabr). "Ken Uorren va Rokfeller jamg'armasining katta e'tibordan chetda qolgan kasalliklar tarmog'i, 1978-1988 yillar: tropik va global tibbiyotning o'zgarishi". Molekulyar tibbiyot. 20 (Qo'shimcha 1): S24-30. doi:10.2119 / molmed.2014.00221. PMC 4374516. PMID 25549230.
Qo'shimcha o'qish
- Butunjahon sog'liqni saqlash tashkiloti beparvo qilingan tropik kasalliklar haqida xabar beradi
- E'tiborsiz qoldirilgan tropik kasalliklarning global ta'sirini engish uchun ish olib borish, 2010 yil oktyabr
- E'tiborsiz qoldirilgan tropik kasalliklarning global ta'sirini engish uchun harakatni davom ettirish, 2013 yil yanvar
- E'tiborsiz qoldirilgan tropik kasalliklarning global ta'sirini engish uchun sarmoyalar, 2015 yil fevral
- Jahon sog'lig'i va rivojlanishida beparvo qilingan tropik kasalliklarni birlashtirish, 2017 yil aprel
Tashqi havolalar
| Tasnifi |
|---|
