Benzodiazepinni olib tashlash sindromi - Benzodiazepine withdrawal syndrome
| Benzodiazepinni olib tashlash sindromi | |
|---|---|
| Boshqa ismlar | Benzo chekinishi |
 | |
| Diazepam ba'zan benzodiazepinni olib tashlashni davolashda ishlatiladi.[1] | |
| Mutaxassisligi | Psixiatriya |
| Benzodiazepinlar |
|---|
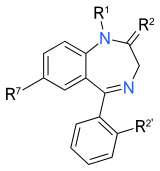 Benzodiazepinlarning yadro tuzilishi. "R" yorliqlari umumiy joylarni bildiradi yon zanjirlar, bu turli xil benzodiazepinlarga o'ziga xos xususiyatlarini beradi. |
Benzodiazepinni olib tashlash sindromi- qisqartirilgan benzo olib qo'yish yoki BZDni olib qo'yish - bu klaster belgilar va alomatlar qabul qilgan odam paydo bo'lganda paydo bo'ladi benzodiazepinlar, tibbiy yoki rekreatsion jihatdan va jismoniy rivojlangan qaramlik, dozani kamaytirish yoki bekor qilishni boshdan kechiradi. Jismoniy qaramlikning rivojlanishi va natijada ularning ba'zilari yillar davomida davom etishi mumkin bo'lgan olib tashlash alomatlari, buyurilgan dori-darmonlarni qabul qilish natijasida kelib chiqishi mumkin. Benzodiazepinning olib tashlanishi uyquni buzilishi, asabiylashish, kuchaygan kuchlanish va tashvish, vahima hujumlari, qo'llarning titrashi, titraganlik, terlash, konsentratsiyadagi qiyinchilik, chalkashlik va kognitiv qiyinchiliklar, xotira muammolari, quruq tortishish va ko'ngil aynish, vazn yo'qotish, yurak urishi, bosh og'rig'i, mushaklarning og'rig'i va qattiqligi, sezgi o'zgarishi, gallyutsinatsiyalar, soqchilik, psixoz,[2] va o'z joniga qasd qilish xavfi ortdi[3][4] (to'liq ro'yxat uchun quyidagi "alomatlar va alomatlar" bo'limiga qarang). Bundan tashqari, ushbu alomatlar mum va susayish uslubi bilan ajralib turadi va zo'ravonlik darajasi to'g'ridan-to'g'ri monotonik tarzda doimiy ravishda pasayish o'rniga kundan-kunga yoki haftadan-haftaga o'zgarib turadi.[5] Ushbu hodisa ko'pincha "to'lqinlar" va "derazalar" deb nomlanadi.
Bu potentsial jiddiy holat bo'lib, murakkab va ko'pincha o'z vaqtida cho'zilib ketadi.[6][7] Kamida uch oy davomida kunlik foydalanish deb ta'riflangan benzodiazepinni uzoq muddatli qo'llash,[8] bog'liqlik xavfining ortishi sababli istalmagan,[9] dozani oshirishi, samaradorligini yo'qotishi, baxtsiz hodisalar va tushish xavfining oshishi, ayniqsa qariyalar uchun,[10] shuningdek, kognitiv,[11] nevrologik va intellektual buzilishlar.[12] Qisqa muddatli foydalanish hipnotiklar, uyquni boshlashda samarali bo'lish bilan birga, uyqusizlik ta'siri tufayli uyquning ikkinchi yarmi yomonlashadi.[13]
Benzodiazepinni olib tashlash og'ir bo'lishi mumkin va hayotni xavf ostiga qo'yadigan alomatlarni keltirib chiqarishi mumkin, masalan, soqchilik,[14] ayniqsa, yuqori dozalarda yoki uzoq muddatli foydalanuvchilarda dozani keskin yoki juda tez pasayishi bilan.[6] Shunga qaramay, dozani bosqichma-bosqich kamaytirilishiga yoki qisqa vaqt ichida foydalanuvchilarga nisbatan past dozalarda bo'lishiga qaramay, pulni olib tashlashga jiddiy javob bo'lishi mumkin,[15] hayvon modellarida bitta katta dozadan keyin ham.[16][17] Shaxslarning ozchilik qismi a uzoq davom etadigan sindrom sindromi alomatlari benzodiazepinlar to'xtaganidan keyin bir necha oy yoki bir necha yil davomida sub-o'tkir darajada saqlanib qolishi mumkin. Uzoq muddatli tortishish sindromini rivojlanish ehtimoli dozani asta-sekin kamaytirish orqali kamaytirilishi mumkin.[18]
Surunkali benzodiazepinlarga ta'sir qilish asab ta'siriga ta'sir qiladi, bu esa preparatning ta'siriga ta'sir qiladi, natijada bag'rikenglik va qaramlik.[19] Doimiy terapevtik dozani qabul qilishiga qaramay, benzodiazepinlarni uzoq muddat iste'mol qilish, ayniqsa dozalar o'rtasida, tortilishga o'xshash alomatlarning paydo bo'lishiga olib kelishi mumkin.[20] Preparat bekor qilinganda yoki dozasi kamaytirilganda, olib tashlash belgilari tana fiziologik moslashuvlarni qaytarguncha paydo bo'lishi va qolishi mumkin.[21] Bular qaytish alomatlari preparat dastlab qabul qilingan alomatlar bilan bir xil bo'lishi mumkin yoki bekor qilish belgilarining bir qismi bo'lishi mumkin.[22] Og'ir holatlarda, tortib olish reaktsiyasi jiddiy psixiatrik va tibbiy holatlarni kuchaytirishi yoki shunga o'xshash bo'lishi mumkin, masalan mani, shizofreniya va, ayniqsa yuqori dozalarda, soqchilik buzilishlar.[23] Ishni to'xtatish alomatlarini tan olmaslik benzodiazepinlarni qabul qilish zarurligi to'g'risida soxta dalillarga olib kelishi mumkin, bu esa o'z navbatida olib tashlash etishmovchiligiga va benzodiazepinlarni qayta tiklanishiga, ko'pincha yuqori dozalarga olib keladi.[23]
Chiqib ketish reaktsiyalari to'g'risida xabardor bo'lish, tortib olish zo'ravonligiga qarab individual konus strategiyalari, ishontirish va benzodiazepinni olib tashlashni qo'llab-quvvatlash guruhlariga murojaat qilish kabi muqobil strategiyalarning qo'shilishi bularning barchasi pulni olib chiqishning muvaffaqiyat darajasini oshiradi.[24][25]
Belgilari va alomatlari
Benzodiazepinlar, barbituratlar yoki spirtli ichimliklar, jiddiy tibbiy asoratlarni keltirib chiqarishi mumkin. Ulardan chiqish xavfliroq ekanligi aytilgan opioidlar.[26] Foydalanuvchilar odatda to'xtatish uchun ozgina maslahat va yordam olishadi.[27] Ba'zi olib tashlash alomatlari dastlab dori buyurilgan alomatlar bilan bir xil,[22] va o'tkir yoki uzoq davom etishi mumkin. Uzoq vaqtdan beri simptomlarning paydo bo'lishi yarim hayot benzodiazepinlar uch haftagacha kechiktirilishi mumkin, ammo qisqa muddatli ta'sirchanlardan ajralish alomatlari ko'pincha erta, odatda 24-48 soat ichida namoyon bo'ladi.[28] Semptomlarda yuqori yoki past dozani to'xtatish bilan bog'liq bo'lgan asosiy farqlar bo'lmasligi mumkin, ammo yuqori dozalardan semptomlar og'irroq bo'ladi.[29]
Kunduzgi qayta tiklanish va tiklanishni bekor qilish alomatlari, ba'zida dozani qabul qilish bilan aralashtirib yuborilishi, qaramlik o'rnatilgandan so'ng paydo bo'lishi mumkin. 'Reergentsiya' - bu preparat dastlab buyurilgan alomatlarning qaytishi, aksincha, 'tiklanish' belgilari simptomlarning qaytishi. u uchun dastlab benzodiazepin qabul qilingan, ammo oldingisiga qaraganda ancha kuchli darajada; "dozani olib tashlash" - bu preparatning oldingi dozasi tugashi va butunlay olib tashlashning yangi tsiklining boshlanishi, bu alomatlar keyingi dozani qabul qilishda tarqalib ketadi, ammo bu dozadan keyin yana bir yangi olib tashlash tsikli boshlanadi. tugaydi, shuning uchun har bir dozani bekor qilishning yangi boshlanishi 'dozani oshirib yuborish chekinish 'va agar kerakli davolanish bo'lmasa, aylanada abadiy takrorlanishi mumkin (buning uchun yarim umr ko'rgan benzo, masalan. diazepam, almashtirish mumkin, shuning uchun preparat dozalar orasida eskirmaydi).[30]
Dozani kamaytirish paytida pulni olib tashlash alomatlari birinchi marta paydo bo'lishi mumkin va ular orasida uyqusizlik, xavotirlik, bezovtalik, vazn yo'qotish, bosh aylanishi, tunda terlash, titroq, mushaklarning qisilishi, afazi, vahima qo'zg'ashlari, depressiya, derealizatsiya, paranoya, oshqozon buzilishi, diareya, fotobobi mavjud. va boshqalar, va odatda triazolam singari qisqa muddatli benzodiazepinlarni to'xtatish bilan bog'liq.[23][31] Kunduzgi alomatlar bir necha kundan bir necha haftagacha tunda benzodiazepindan foydalanishni boshlaganidan keyin paydo bo'lishi mumkin[32][33] yoki zopiklon kabi z-dorilar;[34] tortib olish bilan bog'liq bo'lgan uyqusizlik rebound dastlabki darajadan ham yomonroq,[35][36] va tezda yo'q qilingan benzodiazepinlar uchun, shu jumladan triazolam va temazepam, bu 1991 yilgi kichik tadqiqotga ko'ra (n = 18) qisqacha va vaqti-vaqti bilan ishlatilganda ham yuz berishi mumkin.[37]
Dozani asta-sekin yoki keskin qisqartirish paytida quyidagi alomatlar paydo bo'lishi mumkin:
- Akathisia
- Ajitatsiya va tashvish,[1] mumkin bo'lgan terror va vahima hujumlari[2][38]
- Loyqa ko'rish[38]
- Ko'krak og'rig'i[38]
- Depersonalizatsiya[39] va derealizatsiya (real bo'lmagan tuyg'ular)[40]
- Depressiya (og'ir bo'lishi mumkin),[41] mumkin o'z joniga qasd qilish g'oya
- Kengaygan o'quvchilar[23]
- Bosh aylanishi[38]
- Quruq og'iz[38]
- Dissoriya[42][43]
- Balandligi qon bosimi[44]
- Charchoq va zaiflik[38]
- Oshqozon-ichak traktining buzilishi (ko'ngil aynish, diareya, qusish bilan birga)[45][46][47]
- Eshitish buzilishi[38]
- Bosh og'rig'i[2]
- Issiq va sovuqlar[38]
- Giperosmiya[48]
- Gipertenziya[49]
- Gipnagogik gallyutsinatsiyalar[18]
- Gipoxondriaz[38]
- Tegishga sezgirlikni oshirish[40]
- Kattalashtirilgan siydik chastotasi[38]
- Uyqusizlik[45]
- Nogiron xotira va diqqat[2][38]
- Ishtahani yo'qotish va Ozish[50]
- Engil va o'rtacha afazi[48]
- Kayfiyat o'zgaradi[38]
- Muskulli spazmlar, kramplar, noqulaylik yoki hayratga soladigan narsalar[51]
- Kabuslar[45]
- Obsesif kompulsiv kasallik[52][53]
- Paresteziya[38][40][48][6][54]
- Paranoya[48]
- Terlash[2]
- Fotofobi[48]
- Postural gipotenziya[45]
- REM uyqusida tiklanish[55]
- Bezovta qilinadigan oyoq sindromi[25]
- Qattiqlik[38]
- Taste va hidi buzilishi[38]
- Taxikardiya[56]
- Tinnitus[57]
- Tremor[58][59]
- Vizual buzilishlar[40]
Tez to'xtatish yanada jiddiy sindromga olib kelishi mumkin
- Katatoniya o'limga olib kelishi mumkin[60][61][62]
- Chalkashlik[1]
- Konvulsiyalar,[1] o'limga olib kelishi mumkin[63][64]
- Koma[65] (kamdan-kam)
- Deliryum titraydi[66][67]
- Gipertermiya[45]
- Mania[68][69]
- Neyroleptik malign sindrom o'xshash voqea[70][71] (kamdan-kam)
- Organik miya sindromi[72]
- Shikastlanishdan keyingi stress[25]
- Psixoz[73][74]
- O'z joniga qasd qilish g'oyasi[75] yoki o'z joniga qasd qilish[3][4]
- Zo'ravonlik va tajovuz[38][76]
Chiqib ketish davom etar ekan, bemorlar tez-tez jismoniy va ruhiy sog'lig'ini yaxshilangan kayfiyat va bilimni yaxshilash bilan yaxshilaydi.
Mexanizm
Tolerantlik, qaramlik va tushkunlik mexanizmlari bilan bog'liq neyroadaptiv jarayonlar GABAerjik va glutamaterjik tizimlarga ta'sir qiladi.[19] Gamma-aminobutirik kislota (GABA ) markaziy asab tizimining asosiy inhibitör nörotransmitteridir; taxminan GABA dan sinapslarning to'rtdan uchdan bir qismigacha foydalaniladi.[77] GABA xlorid ionlarining kirib kelishida vositachilik qiladi ligandli xlorli kanallar deb nomlangan GABAA retseptorlari. Xlorid asab hujayrasiga kirganda hujayra membranasi potentsiali giperpolyarizatsiyalanadi va shu bilan depolarizatsiyani inhibe qiladi yoki post-sinaptik asab hujayrasining otish tezligini pasaytiradi.[78] Benzodiazepinlar GABA ta'sirini kuchaytiradi,[79] 5-bo'linma retseptorining a va b subbirliklari orasidagi joyni bog'lash orqali[80] shu bilan GABA borligida xlorli kanal ochilish chastotasini oshiradi.[81]
Potensializatsiya uzoq muddatli foydalanish bilan ta'minlanganda, neyroadaptatsiyalar paydo bo'ladi, natijada GABAergik reaktsiya pasayadi. GABA sirtining aniqligiA retseptorlari oqsil darajasi retseptorlarning aylanish darajasi kabi benzodiazepin ta'siriga javoban o'zgartiriladi.[82] Javobgarlikni kamaytirishning aniq sababi aniqlanmagan, ammo retseptorlar sonining past regulyatsiyasi faqat ba'zi retseptorlarning joylashgan joylarida, shu jumladan, nigraning pars reticulata; retseptorlari sonini pastga tartibga solish yoki ichki holatga keltirish boshqa joylarda asosiy mexanizm bo'lib ko'rinmaydi.[83] Qabul qiluvchilar konformatsiyasining o'zgarishi, aylanishning o'zgarishi, qayta ishlash yoki ishlab chiqarish stavkalari, fosforillanish darajasi va retseptorlari genlarining ekspressioni, subbirlik tarkibi, GABA va benzodiazepin uchastkalari orasidagi bog'lanish mexanizmlarining pasayishi, GABA ishlab chiqarishning pasayishi va kompensator kabi boshqa farazlar uchun dalillar mavjud. glutamaterjik faollikni kuchayishi.[19][82] Birlashtirilgan model gipotezasi retseptorlarning ichki joylashuvining kombinatsiyasini o'z ichiga oladi, so'ngra retseptorlarning gen transkripsiyasidagi o'zgarishlar uchun yadro faolligini ta'minlaydigan ba'zi retseptorlarning kichik bo'linmalarining imtiyozli degradatsiyasi.[82]
Benzodiazepinlar miyadan tozalanganida, bu neyroadaptatsiyalar "niqobsiz" bo'lib, neyronning beg'araz qo'zg'alishiga olib keladi deb taxmin qilingan.[84][tekshirib bo'lmadi ]Glutamat eng keng tarqalgan qo'zg'atuvchidir neyrotransmitter umurtqali hayvonlarda asab tizimi.[85] Chiqib ketish paytida glutamat qo'zg'atuvchi faolligining oshishiga olib kelishi mumkin sezgirlik yoki yonish CNS, ehtimol bilish va simptomatologiyaning yomonlashishiga olib keladi va har bir keyingi olib tashlash davrini yomonlashtiradi.[86][87][88] Oldindan benzodiazepinlardan voz kechish tarixiga ega bo'lganlar keyingi safar muvaffaqiyatga erishish ehtimoli kamligi aniqlandi.[89]
Tashxis
Og'ir holatlarda, tortib olish reaktsiyasi yoki uzoq davom etishi mani, shizofreniya, kabi jiddiy psixiatrik va tibbiy holatlarni kuchaytirishi yoki o'xshash bo'lishi mumkin. qo'zg'atilgan depressiya, vahima buzilishi, umumiy tashvish buzilishi va murakkab qisman tutilishlar va, ayniqsa yuqori dozalarda, soqchilik kasalliklari.[23] Ishni to'xtatish alomatlarini tan olmaslik benzodiazepinlarni qabul qilish zarurligi to'g'risida yolg'on dalillarga olib kelishi mumkin, bu esa o'z navbatida olib tashlash etishmovchiligiga va benzodiazepinlarni qayta tiklanishiga, ko'pincha yuqori dozalarga olib keladi. Oldindan mavjud bo'lgan buzilish yoki boshqa sabablar odatda yaxshilanmaydi, ammo uzoq davom etadigan alomatlar keyingi oylarda asta-sekin yaxshilanadi.[23]
Semptomlar psixologik sabablarga ega bo'lmasligi mumkin va yaxshi va yomon kunlar bilan intensivlikda o'zgarib, oxir-oqibat tiklanishigacha o'zgarishi mumkin.[90][91]
Oldini olish
Ga ko'ra Britaniya milliy formulasi, benzodiazepinlardan tezroq emas, balki juda sekin chiqib ketish yaxshiroqdir.[28] Dozani kamaytirish tezligi simptomlarning intensivligi va zo'ravonligini minimallashtirish uchun eng yaxshi tarzda amalga oshiriladi. Anekdotal ravishda sekin pasayish darajasi uzoq davom etadigan sindromni rivojlanish xavfini kamaytirishi mumkin.
Uzoq yarim umr benzodiazepinlar kabi diazepam[1] yoki xlordiazepoksid rebound ta'sirini minimallashtirish uchun afzaldir va past dozali shakllarda mavjud. Ba'zi odamlar dozani kamaytirish o'rtasida to'liq barqarorlashmasligi mumkin, hatto pasayish darajasi sekinlashganda ham. Bunday odamlar ba'zida shunchaki davom etishlari kerak, chunki ular bir muncha vaqtgacha ulardan butunlay voz kechmaguncha o'zlarini yaxshi his qilmasliklari mumkin.[92]
Menejment

Benzodiazepinga qaramlikni boshqarish odamning yoshi, komorbidligi va benzodiazepinlarning farmakologik yo'llarini hisobga olishni o'z ichiga oladi.[94] Psixologik aralashuvlar faqat to'xtatilgandan keyin va kuzatuv paytida dozani bosqichma-bosqich kamaytirish orqali kichik, ammo sezilarli qo'shimcha foyda keltirishi mumkin.[95] O'rganilgan psixologik tadbirlar gevşeme mashg'ulotlari, uyqusizlikni kognitiv-xulq-atvorli davolash va iste'mol va alomatlarni o'z-o'zini nazorat qilish, maqsadni belgilash, tashlab ketishni boshqarish va tashvish bilan kurashish edi.[95]
Benzodiazepinni olib tashlashni boshqarishda standart yondashuv mavjud emas.[96]Etarli motivatsiya va to'g'ri yondashuv bilan deyarli har bir kishi benzodiazepinlardan muvaffaqiyatli chiqib ketishi mumkin. Ammo uzoq davom etgan va og'ir sindrom nikohlarning buzilishiga, biznesdagi muvaffaqiyatsizlikka, bankrotlikka, kasalxonaga yotqizilishga va eng jiddiy salbiy ta'sir o'z joniga qasd qilishga olib kelishi mumkin.[3] Shunday qilib, uzoq muddatli foydalanuvchilar o'zlarining xohishlariga qarshi to'xtashga majbur qilinmasligi kerak.[6]
Haddan tashqari tez chiqib ketish, tushuntirishning etishmasligi va odamlarni vaqtincha olib tashlash alomatlarini boshdan kechirayotganiga ishontirmaslik, ba'zi odamlarda vahima va aqldan ozishdan qo'rqishlarini kuchayishiga olib keldi, ba'zi odamlar travmadan keyingi stress buzilishlariga o'xshash holatni rivojlantirdilar. natija. Sekin-asta chiqib ketish rejimi, oilangiz, do'stlaringiz va tengdoshlaringizning ishonchi bilan natijani yaxshilaydi.[6][18] 2015 yilgi Cochrane sharhiga ko'ra, kognitiv xulq-atvor terapiyasi plyus konus qisqa muddatda to'xtashga erishishda samarali bo'ldi, ammo olti oydan keyin ta'siri aniq emas edi.[97]
Dori vositalari
Ba'zi bir o'rnini bosuvchi farmakoterapiya va'da qilgan bo'lsa-da, ulardan foydalanishni ta'minlash uchun mavjud dalillar etarli emas.[95] Ba'zi tadkikotlar shuni ko'rsatdiki, o'rnini bosuvchi farmakoterapiyani birdaniga almashtirish faqat dozani bosqichma-bosqich kamaytirishga qaraganda unchalik samarasiz edi va faqat uchta tadqiqot melatonin qo'shishning afzalliklarini topdi,[98] paroksetin,[99] trazodon,[100] yoki valproat[100] dozani bosqichma-bosqich kamaytirish bilan birgalikda.[95]
- Antipsikotiklar odatda benzodiazepinni olib tashlash bilan bog'liq psixoz uchun samarasizdir.[54][101] Benzodiazepinni olib tashlash paytida antipsikotiklardan saqlanish kerak, chunki ular olib tashlash alomatlarini kuchaytiradi, shu jumladan konvulsiyalar.[28][102][103][104] Biroz antipsikotik moddalar pul olish paytida boshqalardan ko'ra xavfli bo'lishi mumkin, ayniqsa klozapin, olanzapin yoki past kuch fenotiyazinlar (masalan, xlorpromazin ), ular pastga tushganda soqchilik chegarasi va pulni olib tashlash oqibatlarini yomonlashtirishi mumkin; agar ishlatilsa, juda ehtiyot bo'lish kerak.[105]
- Barbituratlar benzodiazepinlarga o'zaro chidamli va odatda ulardan qochish kerak; ammo fenobarbital foydalanish mumkin, chunki u nisbatan xavfsiz,[106] pastga qarang.
- Benzodiazepinlar yoki to'xtatilgandan keyin, hatto vaqti-vaqti bilan o'zaro ta'sirga chidamli dori-darmonlardan saqlanish kerak. Ular orasida benzodiazepinlar Z-dorilar, shunga o'xshash harakat mexanizmiga ega. Buning sababi shundaki, benzodiazepinlarga nisbatan bag'rikenglik shaxsiy biokimyoga bog'liq holda olib tashlanganidan keyin to'rt oydan ikki yilgacha davom etadi. Benzodiazepinlarga qayta ta'sir qilish odatda tolerantlik va benzodiazepinni olib tashlash sindromini qayta faollashishiga olib keldi.[107][108]
- Bupropion, asosan antidepressant va chekishni to'xtatish vositasi sifatida ishlatiladigan benzodiazepinlardan yoki boshqa sedativ-gipnozlardan (masalan, alkogoldan) to'satdan chiqib ketishni boshdan kechirayotgan odamlarda, soqchilik xavfi ortishi sababli kontrendikedir.[109]
- Buspirone ko'payish to'xtatilishning muvaffaqiyat darajasini oshirishi aniqlanmadi.[8]
- Kofein uning ogohlantiruvchi xususiyati tufayli olib tashlash alomatlarini yomonlashtirishi mumkin.[6] Kamida bitta hayvonlarni o'rganish ba'zi birlarini ko'rsatdi benzodiazepin saytining modulyatsiyasi soqchilik chegarasini pasayishiga olib keladigan kofein bilan.[110]
- Karbamazepin, an antikonvulsant, benzodiazepinni olib tashlashni davolash va davolashda ba'zi foydali ta'sirlarga ega ekanligi ko'rinadi; ammo tadqiqotlar cheklangan va shu sababli mutaxassislarning benzodiazepinni olib tashlash uchun foydalanish bo'yicha tavsiyalar berish qobiliyati hozircha mumkin emas.[107]
- Etanol, asosiy spirt spirtli ichimliklar, hatto engil va mo''tadil foydalanish ham, ehtimol, shuning uchun olib tashlash etishmovchiligining muhim bashoratchisi ekanligi aniqlandi o'zaro faoliyat bag'rikenglik benzodiazepinlar bilan.[6][107][111]
- Flumazenil bag'rikenglikni qaytarishni va retseptorlarning ishini normallashtirishni rag'batlantirishi aniqlandi. Shu bilan birga, benzodiazepinni olib tashlashni davolashda uning rolini namoyish qilish uchun randomizatsiyalangan sinovlar shaklida qo'shimcha tadqiqotlar o'tkazish kerak.[112] Flumazenil regulyatsiyani rag'batlantiradi va aksini qaytaradi ajratish ning benzodiazepin retseptorlari uchun GABAA retseptorlari, shu bilan bag'rikenglikni qaytarish va olib tashlash alomatlari va relaps stavkalarini kamaytirish.[113][114] Mumkin bo'lgan xavf bilan taqqoslaganda cheklangan tadqiqotlar va tajriba tufayli flumazenilni zararsizlantirish usuli munozarali bo'lib, faqat tibbiy nazorat ostida statsionar tartibda amalga oshirilishi mumkin.
- Flumazenil 4-266 hafta davomida benzodiazepinlardan xoli bo'lgan bemorlarda dushmanlik va tajovuzkorlik tuyg'ularini kamaytirishda platsebodan ko'ra samaraliroq ekanligi aniqlandi.[115] Bu flumazenilning benzodiazepinning uzaygan semptomlarini davolashda rolini taklif qilishi mumkin.
- Lader va Morton tomonidan benzodiazepin retseptorlari antagonisti - flumazenilning benzodiazepinni olib tashlash alomatlariga ta'sirini o'rganish bo'yicha tadqiqot olib borildi. Tadqiqot sub'ektlari bir oydan besh yilgacha benzodiazepinsiz edi, ammo ularning barchasi doimiy ravishda olib tashlanish ta'sirini turli darajalarda qayd etishdi. Doimiy alomatlar orasida bulutli fikrlash, charchoq, bo'yin tarangligi, depersonalizatsiya, kramplar va tebranish va xarakteristikasi sezgir benzodiazepinni olib tashlash alomatlari, ya'ni pinalar va ignalarni his qilish, terining yonishi, og'riq va tanadagi buzilish sub'ektiv hissiyotlari. 0,2-2 mg flumazenil bilan davolash vena ichiga a-da ushbu alomatlarni kamaytirishi aniqlandi platsebo - nazorat ostida o'rganish. Bu benzodiazepin retseptorlari antagonistlari neytral va klinik ta'sirga ega bo'lmaganligi sababli qiziqish uyg'otadi. Tadqiqot muallifi, ehtimol, benzodiazepinni ilgari ishlatilganligi va keyinchalik bag'rikenglik GABA-BZD retseptorlari majmuasining konformatsiyasini teskari agonist konformatsiya va antagonist flumazenil benzodiazepin retseptorlarini asl sezgirligiga qaytaradi. Ushbu tadqiqotda Flumazenil uzoq davom etgan benzodiazepinni olib tashlash sindromi uchun muvaffaqiyatli davo ekanligi aniqlandi, ammo qo'shimcha tadqiqotlar talab etiladi.[116] Shvetsiyadagi professor Borg tomonidan olib borilgan tadqiqotlar uzoq davom etadigan kasallikdan aziyat chekadigan bemorlarda ham xuddi shunday natijalarni keltirib chiqardi.[38] 2007 yilda, Hoffmann – La-Rosh flumazenil ishlab chiqaruvchilari uzoq davom etadigan benzodiazepinni olib tashlash sindromi mavjudligini tan oldilar, ammo bu holatni davolash uchun flumazenilni tavsiya qilmadilar.[117]
- Ftorxinolon antibiotiklar[118][119][120] CNS toksikligi bilan kasallanishni umumiy populyatsiyada 1% dan, benzodiazepinga qaram populyatsiyada yoki ulardan voz kechayotganlarda 4% gacha oshirishi qayd etilgan. Ehtimol, bu ularning GABA antagonistik ta'sirining natijasidir, chunki ular benzodiazepin retseptorlari joylaridan benzodiazepinlarni raqobatdosh ravishda siqib chiqarishi aniqlangan. Ushbu antagonizm susayishdan oldin bir necha hafta yoki bir necha oy davom etishi mumkin bo'lgan o'tkir siqilish belgilarini kuchaytirishi mumkin. Semptomlarga depressiya, tashvish, psixoz, paranoya, og'ir uyqusizlik, parateziya, tinnitus, yorug'lik va tovushga yuqori sezuvchanlik, titroq, holat epileptikus, o'z joniga qasd qilish fikrlari va o'z joniga qasd qilish harakati. Ftorxinolon antibiotiklari benzodiazepinni olib tashlashga bog'liq yoki unga bog'liq bemorlarda kontrendikedir.[6][121][122][123][124] NSAID ba'zi yumshoq GABA antagonistik xususiyatlariga ega va hayvonlarni tadqiq qilish shuni ko'rsatadiki, ba'zilari benzodiazepinlarni bog'lanish joyidan siqib chiqarishi mumkin. Shu bilan birga, ftorxinolonlar bilan birgalikda qabul qilingan NSAIDlar GABA antagonizmini, GABA toksikligini, tutilishlarni va boshqa jiddiy salbiy ta'sirlarni sezilarli darajada ko'payishiga olib keladi.[125][126][127]
- Imidazenil benzodiazepinni olib tashlashni boshqarish bo'yicha bir qator tadqiqotlar olib borgan, ammo hozirda uni olib tashlashda foydalanilmaydi.[128]
- Imipramin to'xtatilishning muvaffaqiyat darajasini statistik ravishda oshirishi aniqlandi.[8]
- Melatonin kattalashtirish uyqusizlikka chalingan odamlar uchun to'xtatish muvaffaqiyat darajasini statistik ravishda oshirishi aniqlandi.[8]
- Fenobarbital, (a barbiturat ), "detoks" yoki boshqa statsionar muassasalarda tez chiqib ketish paytida tutilishlarning oldini olish uchun ishlatiladi sovuq kurka. Fenobarbitaldan keyin bir-ikki haftalik konus keladi, ammo fenobarbitaldan sekin konusga afzallik beriladi.[23] Taqqoslash ishida benzodiazepinlardan foydalangan holda tezkor konus fenobarbital tezkor konusdan ustun ekanligi aniqlandi.[129][130]
- Pregabalin benzodiazepinni olib tashlash simptomlarining og'irligini kamaytirishga yordam berishi mumkin,[131] va qayt qilish xavfini kamaytiradi.[132]
- Progesteron benzodiazepinning chiqarilishini boshqarish uchun samarasiz deb topildi.[112]
- Propranolol to'xtatilishning muvaffaqiyat darajasini oshirishi aniqlanmadi.[8]
- SSRI antidepressantlarning benzodiazepinni olib tashlashni davolashda ahamiyati kamligi aniqlandi.[133]
- Trazodone to'xtatilishning muvaffaqiyat darajasini oshirishi aniqlanmadi.[8]
Statsionar davolanish
Statsionar giyohvand moddalarni zararsizlantirish yoki reabilitatsiya qilish rekreatsion foydalanishdan farqli o'laroq, dori-darmonlarni qabul qilish paytida bardoshli yoki qaram bo'lib qolganlar uchun moslamalar mos kelmasligi mumkin. Bunday statsionar yo'llanmalar suiiste'mol qilmaydiganlar uchun shikast etkazishi mumkin.[23]
Prognoz
2006 yil meta-tahlil bosqichma-bosqich parvarishlash samaradorligi uchun dalillarni topdi: minimal aralashuv (masalan, maslahat xati yuboring yoki to'xtatish to'g'risida maslahat berish uchun ko'plab bemorlar bilan uchrashing), so'ngra birinchi urinish muvaffaqiyatsiz bo'lsa, faqatgina ko'paytirmasdan tizimli qisqartirilgan to'xtatish.[8] Kognitiv xulq-atvor terapiyasi vahima buzilishi, melatonin uyqusizlik va umumiy uzoq muddatli benzodiazepindan foydalanish uchun flumazenil yoki natriy valproat uchun to'xtatish muvaffaqiyat ko'rsatkichlarini yaxshiladi.[8] O'n yillik kuzatuv shuni ko'rsatdiki, uzoq muddatli foydalanishdan muvaffaqiyatli chiqib ketganlarning yarmidan ko'pi ikki yildan keyin ham betaraf bo'lgan va agar ular ushbu holatni ikki yil ichida saqlab qolishsa, ular buni saqlab qolishgan o'n yillik kuzatuvda davlat.[10] Bir tadqiqot shuni ko'rsatdiki, benzodiazepinlarni uzoq muddatli ishlatishdan bir yil voz kechgandan so'ng, kognitiv, nevrologik va intellektual buzilishlar normal holatga qaytgan.[134]
Oldindan psixiatrik tashxis qo'yganlar, ikki yillik kuzatuvda asta-sekin konusdan shunga o'xshash muvaffaqiyat ko'rsatkichlariga ega edilar.[92][135] Benzodiazepinlardan foydalanish antidepressantlardan ko'proq foydalanishga olib kelmadi.[136]
Pulni qaytarib olish jarayoni
Qisqa yoki oraliq ta'sir etuvchi benzodiazepinlardan intensivligi tufayli chiqib ketish juda qiyin bo'lishi mumkin tiklanish dozalar o'rtasida sezilgan alomatlar.[6][137][138][139] Bundan tashqari, qisqa muddatli benzodiazepinlar kuchli intensiv sindromni keltirib chiqaradi.[140] Shu sababli, to'xtatish ba'zida avval an o'rnini bosish bilan amalga oshiriladi ekvivalent dozasi shunga o'xshash uzoqroq ta'sirga ega qisqa ta'sirli benzodiazepinning diazepam yoki xlordiazepoksid. To'g'ri ishlatmaslik ekvivalent miqdor jiddiy tortib olish reaktsiyasini keltirib chiqarishi mumkin.[141] A bilan benzodiazepinlar yarim hayot 24 soatdan ortiq xlordiazepoksid, diazepam, clobazam, klonazepam, xlorazepin kislotasi, ketazolam, medazepam, nordazepam va prazepam. Yarim ishlash muddati 24 soatdan kam bo'lgan benzodiazepinlar alprazolam, bromazepam, brotizolam, flunitrazepam, loprazolam, lorazepam, lormetazepam, midazolam, nitrazepam, oksazepam va temazepam.[10] Natijada ekvivalent dozani asta-sekin kamaytiradi.
Konsensus bir necha hafta davomida dozani asta-sekin kamaytirishdir, masalan. Diazepamning kuniga 30 mg dan ortiq dozalari uchun 4 yoki undan ko'p hafta,[1]odamning alomatlarga toqat qilish qobiliyati bilan belgilanadigan tezlik bilan.[142]Tavsiya etilgan pasayish stavkalari har hafta yoki undan ko'proq vaqt davomida boshlang'ich dozaning 50% gacha o'zgarib turadi,[143]har 2 haftada sutkalik dozaning 10-25% gacha.[142]Masalan, Xezer Eshton protokolida qo'llanilgan pasayish darajasi diazepamning 0,5 mg yoki 2,5 mg dozasida yakuniy doza bilan kamayishiga zo'ravonligi va ta'siriga qarab, har ikki-to'rt haftada qolgan dozaning 10% ni yo'q qilishni talab qiladi. xlordiazepoksid.[6]Ko'pgina odamlar uchun 4-6 hafta yoki 4-8 hafta davomida to'xtatish mos keladi.[144]Chiqib ketish jarayoni odam uchun "kasal markazida" bo'lishiga yo'l qo'ymaslik uchun ko'p oylar davomida uzoq muddatli pasayishdan saqlanish kerak.[107]
Muddati
Oxirgi dozani qabul qilgandan so'ng, pulni olib tashlashning o'tkir bosqichi, odatda, taxminan ikki oy davom etadi, ammo chekish belgilari, hatto past dozani qo'llagan taqdirda ham, ushbu davrda asta-sekin yaxshilanadigan olti oydan o'n ikki oygacha davom etishi mumkin,[29][92] ammo, klinik jihatdan ahamiyatli chekinish alomatlari yillar davomida davom etishi mumkin, garchi asta-sekin pasayib ketsa.
Sakkiz hafta davomida benzodiazepin alprazolamni qabul qilgan bemorlarning klinik tekshiruvi alprazolam to'xtaganidan sakkiz hafta o'tgach ham davom etgan xotira etishmovchiligining uzaygan alomatlarini keltirib chiqardi.[145]
Uzoq muddatli sindrom sindromi
Uzoq muddatli sindirish sindromi bir necha oy yoki hatto yillar davomida saqlanib turadigan alomatlarga ishora qiladi. Benzodiazepinlardan voz kechadigan odamlarning ozchilik qismi, ehtimol 10% dan 15% gacha, a uzoq davom etadigan sindrom sindromi ba'zida bu og'ir bo'lishi mumkin. Alomatlar tinnitusni o'z ichiga olishi mumkin,[57][146] psixoz, kognitiv nuqsonlar, oshqozon-ichak traktining shikoyati, uyqusizlik, paresteziya (karıncalanma va karaxtlik), og'riq (odatda oyoq-qo'llarda va ekstremitalarda), mushaklarda og'riq, zaiflik, kuchlanish, og'riqli titroq, titroq xurujlari, jirkanchliklar, bosh aylanishi va blefarospazm[18] va ushbu alomatlar oldindan mavjud bo'lmagan tarixsiz ham paydo bo'lishi mumkin. Dozani kamaytirish yoki benzodiazepinlarni qabul qilishni to'xtatish paytida paydo bo'ladigan tinnitus benzodiazepinlarni tavsiya etish bilan yumshatiladi. Bosh aylanishi ko'pincha eng uzoq davom etadigan tortishish belgisi sifatida qayd etiladi.
Nöropsikologik omillarni sinab ko'rgan tadqiqotda psixofiziologik belgilar normal holatdan farq qiladi va uzoq muddatli sindirish sindromi uzoq muddatli foydalanish natijasida kelib chiqqan asl yatrogenik holat degan xulosaga keldi.[147] Doimiy simptomlarning sabablari - bu doimiy ta'sir ko'rsatadigan retseptorlarning o'zgarishi, giyohvandlik vositasi tomonidan kelib chiqadigan va preparatdan ajralib turadigan psixologik omillar, ehtimol ba'zi hollarda, ayniqsa yuqori dozada foydalanuvchilar, miyaning strukturaviy shikastlanishi yoki tizimli neyronlarning shikastlanishi kabi farmakologik omillarning kombinatsiyasi.[18][148] Semptomlar vaqt o'tishi bilan yaxshilanishda davom etmoqda, ko'pincha odamlar hatto yillar davomida qobiliyatsiz bo'lganidan keyin ham o'zlarining normal hayotlarini tiklaydilar.[6]
Sekin olib chiqish darajasi uzoq muddatli yoki og'ir tortib olish holati xavfini sezilarli darajada kamaytiradi. Uzoq muddatli olib tashlash alomatlari yaxshi kunlar va yomon kunlar bilan belgilanishi mumkin. Uzoq muddatli tortishish paytida alomatlar vaqti-vaqti bilan ko'payganda, fiziologik o'zgarishlar, shu jumladan bo'lishi mumkin kengaygan o'quvchilar shuningdek qon bosimi va yurak urish tezligining oshishi.[23] Semptomlarning o'zgarishi tolerantlikni qaytarish jarayonida GABA uchun retseptorlari sezgirligining o'zgarishi tufayli taklif qilingan.[6] A meta-tahlil benzodiazepindan foydalanish tufayli ko'plab sohalarda kognitiv buzilishlar olti oylik bekor qilinganidan keyin yaxshilanishlarni ko'rsatdi, ammo aksariyat sohalarda sezilarli darajada buzilishlar doimiy bo'lishi mumkin yoki ularni qaytarish uchun olti oydan ko'proq vaqt talab qilinishi mumkin.[149]
Uzoq muddatli alomatlar ko'p oylar yoki bir necha yil davomida susayib boraveradi. Uzoq muddatli benzodiazepinni olib tashlash sindromi uchun vaqtdan tashqari ma'lum davo yo'q,[18] ammo, flumazenil preparati 4-26 hafta davomida benzodiazepinlardan xoli bo'lgan bemorlarda dushmanlik va tajovuzkorlik tuyg'ularini kamaytirishda platsebodan ko'ra samaraliroq ekanligi aniqlandi.[115] Bu flumazenilning benzodiazepinning uzaygan semptomlarini davolashda rolini taklif qilishi mumkin.
Epidemiologiya
Chiqib ketish sindromining og'irligi va davomiyligi turli xil omillar, jumladan, torayish tezligi, foydalanish muddati va dozalari hajmi va mumkin bo'lgan genetik omillar bilan belgilanadi.[6][150] Oldingi benzodiazepinlardan voz kechish tarixiga ega bo'lganlar a sezgir yoki yondi markaziy asab tizimi kognitiv va simptomatologiyaning yomonlashishiga olib keladi va har bir keyingi tortishish davrini yomonlashtiradi.[86][87][88][151]
Maxsus populyatsiyalar
Pediatriya
Onadan benzodiazepinlarni qabul qilganida, ba'zida og'ir bo'lgan neonatal tortishish sindromi paydo bo'lishi mumkin, ayniqsa uchinchi trimestr. Alomatlar kiradi gipotoniya, apnoe afsunlar, siyanoz, nogiron metabolik sovuq stressga javoblar va soqchilik. Neonatal benzodiazepinni olib tashlash sindromi tug'ilgandan keyin bir necha oydan keyin davom etishi haqida xabar berilgan.[152]
Chiqib ketish sindromi taxminan 20% da kuzatiladi pediatrik intensiv terapiya bo'limi bolalari benzodiazepinlar yoki opioidlar bilan infuziya qilinganidan keyin.[153] Sindromga ega bo'lish ehtimoli infuziyaning umumiy davomiyligi va dozasi bilan bog'liq, ammo davomiyligi muhimroq deb hisoblanmoqda.[154] Chiqib ketishni davolash odatda infuziya bir haftadan ko'proq davom etgan bo'lsa, 3- dan 21 kungacha bo'lgan davrda sutdan ajratishni o'z ichiga oladi.[155] Semptomlar orasida titroq, qo'zg'alish, uyqusizlik, aql bovar qilmaydigan yig'lash, diareya va terlash mavjud. Hammasi bo'lib, ellikdan ortiq pulni olib tashlash alomatlari ushbu sharh maqolasida keltirilgan.[153][156] Kuchli abstinentsiya sindromi bo'lgan yangi tug'ilgan chaqaloqlarning alomatlarini yumshatishga qaratilgan atrof-muhit choralari juda oz ta'sir ko'rsatdi, ammo engil holatlarda tinch uyqu muhitini ta'minlash yordam berdi.[153]
Homiladorlik
Xavotirlari tufayli benzodiazepinlarni yoki antidepressantlarni to'satdan to'xtatish teratogen dorilarning ta'siri jiddiy asoratlarni keltirib chiqarish xavfi yuqori, shuning uchun tavsiya etilmaydi. Masalan, benzodiazepinlarni yoki antidepressantlarni keskin chiqarib yuborish ekstremal alomatlarni keltirib chiqarish xavfi yuqori, shu jumladan o'z joniga qasd qilish g'oyasi va agar mavjud bo'lsa, asosiy buzilishning qaytishi. Bu kasalxonaga yotqizilishiga va potentsial ravishda o'z joniga qasd qilishga olib kelishi mumkin. Bir tadqiqotga ko'ra, o'z dori-darmonlarini to'satdan to'xtatgan yoki juda tez toraytirgan onalarning uchdan bir qismi «chidab bo'lmas alomatlar» tufayli o'z joniga qasd qilishgan. Bitta ayolda tibbiy abort, endi u dosh berolmasligini sezganligi sababli va yana bir ayol benzodiazepinlardan ajralish alomatlari bilan kurashish uchun spirtli ichimliklarni ishlatgan. O'z-o'zidan abort qilish shuningdek, psixotrop dori-darmonlarni, shu jumladan benzodiazepinlarni keskin olib tashlash natijasida paydo bo'lishi mumkin. Tadqiqot natijalariga ko'ra, shifokorlar odatda to'satdan og'ir oqibatlarga olib kelishini bilishmaydi chekinish ning psixotrop benzodiazepinlar yoki antidepressantlar kabi dorilar.[75]
Qariyalar
Benzodiazepinga qaram bo'lgan keksa yoshdagi odamlarni olib tashlashni o'rganish juda kam asoratlar bilan amalga oshirilishi mumkin va uxlash va bilim qobiliyatlarini yaxshilashga olib kelishi mumkin. Muvaffaqiyatli ishdan bo'shatilgandan 52 hafta o'tgach, kognitiv holatning 22% yaxshilanishi va ijtimoiy faoliyat yaxshilanganligi aniqlandi. Benzodiazepinlarda qolganlar kognitiv qobiliyatlarning 5% pasayishiga duch kelishdi, bu odatdagi qarishda kuzatilganidan tezroq bo'lib tuyuldi, demak benzodiazepinlarni qabul qilish qancha ko'p bo'lsa, bilish effektlari shunchalik yomonlashadi. Semptomlarning ba'zi bir yomonlashishi benzodiazepinni iste'mol qilishni to'xtatishning birinchi oylarida kuzatilgan, ammo 24 haftalik kuzatuvda benzodiazepinlarda qolganlarga nisbatan keksa yoshdagi odamlar aniq yaxshilandi. 24 va 52 haftalik kuzatuvlarda uyquning yaxshilanishi kuzatildi. Mualliflarning fikriga ko'ra, benzodiazepinlar uzoq vaqt davomida uyqudagi muammolar uchun samarali emas edi, faqat olib tashlash bilan bog'liq bo'lganlarni bostirishdan tashqari uyqusizlikni tiklash. Ishdan bo'shatilgandan keyin 24 va 52 xafta orasida yaxshilanishlar ko'plab omillar, jumladan, uyquni yaxshilash va bir nechta bilim va ishlash qobiliyatlarini yaxshilagan. Benzodiazepinlarga sezgir bo'lgan ba'zi bilim qobiliyatlari, shuningdek yoshi, masalan epizodik xotira yaxshilanmadi. Biroq, mualliflar, 3,5 yillik kuzatuvida hech qanday xotira buzilishini ko'rsatmagan va ba'zi xotira funktsiyalari surunkali benzodiazepinni qayta tiklashdan uzoqroq vaqt talab qilishi va keksa odamlarning kognitiv funktsiyalarini yanada takomillashtirish 52 haftadan keyin sodir bo'lishi mumkinligi haqida taxmin qilgan yosh bemorlarda o'tkazilgan tadqiqotni keltirdilar. chekinish. Benzodiazepindan foydalanishni to'xtatgandan so'ng yaxshilanishlarni ko'rish uchun 24 hafta davom etganining sababi, miyaning benzodiazepinsiz muhitga moslashishi uchun zarur bo'lgan vaqt bilan bog'liq edi.[157]
24-haftada sezilarli yaxshilanishlar aniqlandi, shu jumladan ma'lumotni qayta ishlash aniqligi yaxshilandi, ammo benzodiazepinlarda qolganlarda pasayish kuzatildi. 52 haftalik kuzatuvda keyingi yaxshilanishlar qayd etildi, bu benzodiazepinning abstinentsiyasi bilan davom etayotgan yaxshilanishlarni ko'rsatmoqda. Benzodiazepinlar bilan shug'ullanadigan yoshroq odamlar vizual fazoviy xotirada kognitiv yomonlashuvni boshdan kechirmoqdalar, ammo kognitiv ta'sirga qariyalar kabi zaif emaslar.[157] Benzodiazepinlardan xoli keksa bemorlarda reaktsiyaning yaxshilangan vaqtlari 52 xaftada qayd etildi. Bu keksa yoshdagi odamlarda, ayniqsa benzodiazepin iste'molchilarida yo'l-transport hodisalari xavfi ortishi sababli avtomashinani boshqarishda muhim ahamiyatga ega.[157] 24 haftalik kuzatuvda odamlarning 80% benzodiazepinlardan muvaffaqiyatli chiqib ketishdi. Muvaffaqiyatning bir qismi platsebo buzilgan sud jarayoni uchun ishlatiladigan usul psixologik qaramlik keksa bemorlar bir necha hafta oldin asta-sekin kamayishini tugatganligini va faqat platsebo tabletkalarini iste'mol qilishganini anglaganlarida, benzodiazepinlarda. Bu ularni tabletkasiz uxlashlariga ishontirishga yordam berdi.[157]
Mualliflar, shuningdek, farmakologiyaning o'xshashligi va yangisini ta'sir qilish mexanizmi haqida ogohlantirdilar benzodiazepin Z dorilar.[157]
The yarim umrni yo'q qilish diazepam va xlordiazepoksid, shuningdek boshqa yarim umr ko'rish benzodiazepinlari yoshi kattalarga qaraganda qariyalarda ikki baravar ko'p. Ko'pgina shifokorlar benzodiazepin dozasini keksa bemorlarda yoshga qarab sozlamaydilar.[158]
Shuningdek qarang
Adabiyotlar
- ^ a b v d e f Soyka M (2017). "Treatment of Benzodiazepine Dependence". Nyu-England tibbiyot jurnali. 376 (12): 1147–1157. doi:10.1056/NEJMra1611832. PMID 28328330. S2CID 205117734.CS1 maint: ref = harv (havola)
- ^ a b v d e Petursson, H. (1994). "The benzodiazepine withdrawal syndrome". Giyohvandlik. 89 (11): 1455–9. doi:10.1111/j.1360-0443.1994.tb03743.x. PMID 7841856.
- ^ a b v Colvin, Rod (26 August 2008). Overcoming Prescription Drug Addiction: A Guide to Coping and Understanding (3 nashr). United States of America: Addicus Books. 74-76 betlar. ISBN 978-1-886039-88-9.
I have treated ten thousand patients for alcohol and drug problems and have detoxed approximately 1,500 patients for benzodiazepines – the detox for the benzodiazepines is one of the hardest detoxes we do. It can take an extremely long time, about half the length of time they have been addicted – the ongoing relentless withdrawals can be so incapacitating it can cause total destruction to one’s life – marriages break up, businesses are lost, bankruptcy, hospitalization, and of course suicide is probably the most single serious side effect.
- ^ a b Dodds TJ (2017). "Belgilangan benzodiazepinlar va o'z joniga qasd qilish xavfi: adabiyotga sharh". Primary Care Companion for CNS Disorders. 19 (2). doi:10.4088 / PCC.16r02037. PMID 28257172.
- ^ C. Heather Ashton DM. "Chapter III: Benzodiazepine withdrawal symptoms, acute & protracted". Institute of Neuroscience, Newcastle University. Olingan 29 aprel 2013.
Benzodiazepines : How they work and how to withdraw
- ^ a b v d e f g h men j k l m n Professor Xizer Eshton (2002). "Benzodiazepinlar: ular qanday ishlaydi va qanday qilib tortib olinadi". Arxivlandi from the original on 15 September 2011.
- ^ O'Konnor, RD (1993). "Benzodiazepine dependence—a treatment perspective and an advocacy for control". NIDA tadqiqotlari monografiyasi. 131: 266–9. PMID 8105385.
- ^ a b v d e f g h Voshaar, R. C. O.; Couvée, JE; Van Balkom, AJ; Mulder, PG; Zitman, FG (2006). "Strategies for discontinuing long-term benzodiazepine use: Meta-analysis". Britaniya psixiatriya jurnali. 189 (3): 213–20. doi:10.1192/bjp.189.3.213. PMID 16946355.
- ^ Nutt, David (1986). "Benzodiazepine dependence in the clinic: Reason for anxiety?". Farmakologiya fanlari tendentsiyalari. 7: 457–60. doi:10.1016/0165-6147(86)90420-7.
- ^ a b v De Gier, N.; Gorgels, W.; Lucassen, P.; Oude Voshaar, R.; Mulder, J.; Zitman, F. (2010). "Discontinuation of long-term benzodiazepine use: 10-year follow-up". Oilaviy amaliyot. 28 (3): 253–9. doi:10.1093/fampra/cmq113. PMID 21193495.
- ^ Authier, Nicolas; Boucher, Alexandra; Lamaison, Dominique; Llorca, Pierre-Michel; Descotes, Jacques; Eschalier, Alain (2009). "Second Meeting of the French CEIP (Centres d'Évaluation et d'Information sur la Pharmacodépendance). Part II: Benzodiazepine Withdrawal". Terapiya. 64 (6): 365–70. doi:10.2515/therapie/2009051. PMID 20025839.
- ^ Xeberlein, A .; Bleyx, S .; Kornxuber, J .; Hillemacher, T. (2008). "Benzodiazepin-Abhängigkeit: Ursachen und Behandlungsmöglichkeiten" [Benzodiazepine Dependence: Causalities and Treatment Options]. Fortschritte der Neurologie · Psixiatriya (nemis tilida). 77 (1): 7–15. doi:10.1055/s-0028-1100831. PMID 19101875.
- ^ Lee-chiong, Teofilo (24 April 2008). Sleep Medicine: Essentials and Review. Oksford universiteti matbuoti, AQSh. p. 468. ISBN 978-0-19-530659-0.
- ^ Evans, Katie; Sullivan, Michael J. (2001). "Withdrawal and Medical Issues". Dual Diagnosis: Counseling the Mentally Ill Substance Abuser (2-nashr). Guilford Press. 52-3 betlar. ISBN 978-1-57230-446-8. Arxivlandi asl nusxasidan 2018 yil 3 mayda.
- ^ Lader, M (1987). "Long-term anxiolytic therapy: The issue of drug withdrawal". Klinik psixiatriya jurnali. 48 Suppl: 12–6. PMID 2891684.
- ^ Boisse, NR; Periana, RM; Guarino, JJ; Kruger, HS; Samoriski, GM (1986). "Pharmacologic characterization of acute chlordiazepoxide dependence in the rat". Farmakologiya va eksperimental terapiya jurnali. 239 (3): 775–83. PMID 3098961.
- ^ Boisse, NR; Periana, RM; Guarino, JJ; Kruger, HS (1986). "Acute chlordiazepoxide dependence in the rat: Comparisons to chronic". NIDA tadqiqotlari monografiyasi. 67: 197–201. PMID 3092067.
- ^ a b v d e f Professor Heather Ashton (2004). "Protracted Withdrawal Symptoms From Benzodiazepines". Comprehensive Handbook of Drug & Alcohol Addiction.
- ^ a b v Allison, C; Pratt, J.A (2003). "Neuroadaptive processes in GABAergic and glutamatergic systems in benzodiazepine dependence". Farmakologiya va terapiya. 98 (2): 171–95. doi:10.1016/S0163-7258(03)00029-9. PMID 12725868.
- ^ Herman, JB; Brotman, AW; Rosenbaum, JF (1987). "Rebound anxiety in panic disorder patients treated with shorter-acting benzodiazepines". Klinik psixiatriya jurnali. 48 Suppl: 22–8. PMID 2889722.
- ^ Allgulander, C; Bandelou, B; Hollander, E; Montgomery, SA; Nutt, DJ; Okasha, A; Pollack, MH; Shteyn, DJ; Swinson, RP; World Council Of, Anxiety (2003). "WCA recommendations for the long-term treatment of generalized anxiety disorder". CNS spektrlari. 8 (8 Suppl 1): 53–61. doi:10.1017/S1092852900006945. PMID 14767398.
- ^ a b Salzman, Carl (1993). "Benzodiazepine treatment of panic and agoraphobic symptoms: Use, dependence, toxicity, abuse". Psixiatriya tadqiqotlari jurnali. 27: 97–110. doi:10.1016/0022-3956(93)90021-S. PMID 7908335.
- ^ a b v d e f g h men Gabbard, Glen O. (15 May 2007). Gabbard's Treatments of Psychiatric Disorders, Fourth Edition (Treatments of Psychiatric Disorders). Amerika psixiatriya nashriyoti. 209–211 betlar. ISBN 978-1-58562-216-0.
- ^ Onyett, SR (1989). "The benzodiazepine withdrawal syndrome and its management". Qirollik umumiy amaliyot shifokorlari kolleji jurnali. 39 (321): 160–3. PMC 1711840. PMID 2576073.
- ^ a b v Ashton, Heather (1991). "Protracted withdrawal syndromes from benzodiazepines". Moddani suiiste'mol qilishni davolash jurnali. 8 (1–2): 19–28. doi:10.1016/0740-5472(91)90023-4. PMID 1675688.
- ^ Lindsay, S.J.E.; Powell, Graham E., eds. (1999). The Handbook of Clinical Adult Psychology (2-nashr). Yo'nalish. p. 363. ISBN 978-0-415-07215-1.
- ^ Authier, N .; Balayssak, D .; Sautereau, M .; Zangarelli, A .; Korti, P .; Somogyi, A.A.; Vennat, B .; Llorka, P.-M .; Eschalier, A. (2009). "Benzodiazepinga qaramlik: to'xtatish sindromiga e'tibor". Annales Pharmaceuticaliques Françaises. 67 (6): 408–13. doi:10.1016 / j.pharma.2009.07.001. PMID 19900604.
- ^ a b v Committee on Safety of Medicines (2007). "Gipnoz va anksiyolitiklar". Britaniya milliy formulasi. Olingan 17 sentyabr 2007.(ro'yxatdan o'tish talab qilinadi)
- ^ a b Murphy, S. M.; Tyrer, P. (1991). "A double-blind comparison of the effects of gradual withdrawal of lorazepam, diazepam and bromazepam in benzodiazepine dependence". Britaniya psixiatriya jurnali. 158 (4): 511–6. doi:10.1192/bjp.158.4.511. PMID 1675901.
- ^ Heather, Ashton. "BENZODIAZEPINES: HOW THEY WORK AND HOW TO WITHDRAW". The Ashton Manual. New Castle University Institute of Neuroscience. Olingan 28 dekabr 2017.
- ^ Adam, Kirstine; Oswald, I. (2008). "Can a Rapidly-eliminated Hypnotic Cause Daytime Anxiety?". Farmakopsixiatriya. 22 (3): 115–9. doi:10.1055/s-2007-1014592. PMID 2748714.
- ^ Scharf, Martin B; Kales, Judith A; Bixler, EO; Jacoby, JA; Schweitzer, PK (1982). "Lorazepam—Efficacy, side effects, and rebound phenomena". Klinik farmakologiya va terapiya. 31 (2): 175–9. doi:10.1038/clpt.1982.27. PMID 6120058. S2CID 464310.
- ^ Walsh, James K; Schweitzer, Paula K; Parwatikar, Sadashiv (1983). "Effects of lorazepam and its withdrawal on sleep, performance, and subjective state". Klinik farmakologiya va terapiya. 34 (4): 496–500. doi:10.1038/clpt.1983.203. PMID 6617072. S2CID 29955775.
- ^ Fontaine, Réjean; Beaudry, Paul; Le Morvan, Patrick LE; Beauclair, Linda; Chouinard, GUY (1990). "Zopiclone and Triazolam in Insomnia Associated with Generalized Anxiety Disorder". Xalqaro klinik psixofarmakologiya. 5 (3): 173–83. doi:10.1097/00004850-199007000-00002. PMID 2230061.
- ^ Kales, Entoni; Bixler, Edward O.; Soldatos, Constantin R.; Jacoby, Judith A.; Kales, Joyce D. (1986). "Lorazepam: Effects on Sleep and Withdrawal Phenomena". Farmakologiya. 32 (3): 121–30. doi:10.1159/000138160. PMID 3960963.
- ^ Bonnet, M H; Arand, D L (1999). "The use of lorazepam TID for chronic insomnia". Xalqaro klinik psixofarmakologiya. 14 (2): 81–9. doi:10.1097/00004850-199903000-00004. PMID 10220122.
- ^ Kales, Entoni; Manfredi, Rocco L; Vgontzas, Alexandras N; Bixler, Edward O; Vela-Bueno, Antonio; Fee, Eric C (1991). "Rebound insomnia after only brief and intermittent use of rapidly eliminated benzodiazepines". Klinik farmakologiya va terapiya. 49 (4): 468–76. doi:10.1038/clpt.1991.55. PMID 2015735. S2CID 185909.
- ^ a b v d e f g h men j k l m n o p q Sakson, L .; Hjemdahl, P.; Hiltunen, A. J.; Borg, S. (1997). "Effects of flumazenil in the treatment of benzodiazepine withdrawal - a double-blind pilot study". Psixofarmakologiya. 131 (2): 153–60. doi:10.1007/s002130050278. PMID 9201803. S2CID 19374966.
- ^ Terao, T; Yoshimura, R; Terao, M; Abe, K (1992). "Depersonalization following nitrazepam withdrawal". Biologik psixiatriya. 31 (2): 212–3. doi:10.1016/0006-3223(92)90209-I. PMID 1737083. S2CID 26522217.
- ^ a b v d Mintzer, M. Z.; Stoller, K. B.; Griffiths, R. R. (1999). "A controlled study of flumazenil-precipitated withdrawal in chronic low-dose benzodiazepine users". Psixofarmakologiya. 147 (2): 200–9. doi:10.1007/s002130051161. PMID 10591888. S2CID 35666163.
- ^ Lader, Malcolm (1994). "Anxiety or depression during withdrawal of hypnotic treatments". Psixosomatik tadqiqotlar jurnali. 38: 113–23, discussion 118–23. doi:10.1016/0022-3999(94)90142-2. PMID 7799243.
- ^ Mendelson, WB; Weingartner, H; Grinblatt, DJ; Garnett, D; Gillin, JC (1982). "A clinical study of flurazepam". Uyqu. 5 (4): 350–60. doi:10.1093/sleep/5.4.350. PMID 6761826.
- ^ Schöpf, J. (2008). "Withdrawal Phenomena after Long-term Administration of Benzodiazepines a Review of Recent Investigations". Farmakopsixiatriya. 16 (1): 1–8. doi:10.1055/s-2007-1017439. PMID 6131447.
- ^ Mintzer, Miriam Z.; Griffiths, Roland R. (2004). "Flumazenil-precipitated withdrawal in healthy volunteers following repeated diazepam exposure". Psixofarmakologiya. 178 (2–3): 259–67. doi:10.1007/s00213-004-2009-1. PMID 15452683. S2CID 22130710.
- ^ a b v d e Bismuth, C; Le Bellec, M; Dally, S; Lagier, G (1980). "Benzodiazepine physical dependence. 6 cases (author's transl)". La Nouvelle Presse Medicale. 9 (28): 1941–5. PMID 6106922.
- ^ Loeb, P; Adnet, P; Boittiaux, P; Forget, AP; Mille, FX (1997). "Sevrage en benzodiazépines révélé par un syndrome douloureux abdominal pseudochirurgical" [Benzodiazepine withdrawal masquerading as surgical abdominal syndrome]. Annales Françaises d'Anesthésie et de Reanimation (frantsuz tilida). 16 (5): 521–2. doi:10.1016/S0750-7658(97)83345-X. PMID 9750606.
- ^ http://www.benzo.org.uk/manual/bzcha03.htm#16[to'liq iqtibos kerak ]
- ^ a b v d e Pelissolo, A; Bisserbe, JC (1994). "Dependence on benzodiazepines. Clinical and biological aspects". L'Encefale. 20 (2): 147–57. PMID 7914165.
- ^ Biswas, AK; Feldman, BL; Davis, DH; Zintz, EA (2005). "Myocardial ischemia as a result of severe benzodiazepine and opioid withdrawal". Klinik toksikologiya. 43 (3): 207–9. doi:10.1081/clt-200053099. PMID 15902797.
- ^ Pecknold, J.C. (1993). "Discontinuation reactions to alprazolam in panic disorder". Psixiatriya tadqiqotlari jurnali. 27: 155–170. doi:10.1016/0022-3956(93)90025-W. PMID 8145176.
- ^ Kliniska Färdigheter: Mellan bemor Och Läkare, LINDGREN, STEFAN, ISBN 91-44-37271-X (Shved)[sahifa kerak ]
- ^ Drummond, Lynne M.; Matthews, Helen P. (1988). "SINGLE CASE STUDY Obsessive-Compulsive Disorder Occurring as a Complication in Benzodiazepine Withdrawal". Asab va ruhiy kasalliklar jurnali. 176 (11): 688–91. doi:10.1097/00005053-198811000-00008. PMID 3183654. S2CID 28340232.
- ^ Matthews, HP; Drummond, LM (1987). "Obsessive-compulsive disorder—a complication of benzodiazepine withdrawal". Britaniya psixiatriya jurnali. 150 (2): 272. doi:10.1192/s0007125000122810. PMID 3651695.
- ^ a b Shader, RI; Greenblatt, DJ (1981). "The use of benzodiazepines in clinical practice". Britaniya klinik farmakologiya jurnali. 11 Suppl 1 (Suppl 1): 5S–9S. doi:10.1111/j.1365-2125.1981.tb01832.x. PMC 1401641. PMID 6133535.
- ^ Pagel, J. F.; Parnes, Bennett L. (2001). "Medications for the Treatment of Sleep Disorders". Klinik psixiatriya jurnaliga birlamchi tibbiy yordam. 3 (3): 118–125. doi:10.4088/PCC.v03n0303. PMC 181172. PMID 15014609.
- ^ Van Engelen, BG; Gimbrere, JS; Booy, LH (1993). "Benzodiazepine withdrawal reaction in two children following discontinuation of sedation with midazolam". Farmakoterapiya yilnomalari. 27 (5): 579–81. doi:10.1177/106002809302700509. PMID 8347907. S2CID 38855049.
- ^ a b Beeley, L (1991). "Benzodiazepines and tinnitus". BMJ. 302 (6790): 1465. doi:10.1136/bmj.302.6790.1465. PMC 1670117. PMID 2070121.
- ^ Mellor, CS; Jain, VK (1982). "Diazepam withdrawal syndrome: Its prolonged and changing nature". Kanada tibbiyot birlashmasi jurnali. 127 (11): 1093–6. PMC 1862031. PMID 7139456.
- ^ Olajide, Dele; Lader, Malcolm (2009). "Depression following withdrawal from long-term benzodiazepine use: A report of four cases". Psixologik tibbiyot. 14 (4): 937–40. doi:10.1017/S0033291700019899. PMID 6152745.
- ^ Rosebush, Patricia I.; Mazurek, Michael F. (1996). "Catatonia After Benzodiazepine Withdrawal". Klinik psixofarmakologiya jurnali. 16 (4): 315–9. doi:10.1097/00004714-199608000-00007. PMID 8835707.
- ^ Deuschle, M.F.; Lederbogen, F (2001). "Benzodiazepine Withdrawal - Induced Catatonia". Farmakopsixiatriya. 34 (1): 41–2. doi:10.1055/s-2001-15188. PMID 11229621.
- ^ Kanemoto, Kousuke; Miyamoto, Toshio; Abe, Ryuji (1999). "Ictal catatonia as a manifestation of de novo absence status epilepticus following benzodiazepine withdrawal". Tutqanoq. 8 (6): 364–6. doi:10.1053/seiz.1999.0309. PMID 10512781. S2CID 17454162.
- ^ Metten, Pamela; Crabbe, John C (1999). "Genetic Determinants of Severity of Acute Withdrawal from Diazepam in Mice". Farmakologiya Biokimyo va o'zini tutish. 63 (3): 473–9. doi:10.1016/S0091-3057(99)00017-9. PMID 10418790. S2CID 21241791.
- ^ Haque, W; Watson, DJ; Bryant, SG (1990). "Death following suspected alprazolam withdrawal seizures: A case report". Texas tibbiyoti. Vol. 86 yo'q. 1. pp. 44–7. PMID 2300914.
- ^ De Bard, ML (1979). "Diazepam withdrawal syndrome: A case with psychosis, seizure, and coma". Amerika psixiatriya jurnali. 136 (1): 104–5. doi:10.1176/ajp.136.1.104. PMID 103443.
- ^ Provini, F.; Cortelli, P.; Montagna, P .; Gambetti, P .; Lugaresi, E. (2008). "Fatal insomnia and agrypnia excitata: Sleep and the limbic system". Revue Neurologique. 164 (8–9): 692–700. doi:10.1016/j.neurol.2007.11.003. PMID 18805303.
- ^ Berezak, A.; Weber, M .; Hansmann, J.; Tulasne, P.A.; Laporte, B.; Ould Ouali, A. (1984). "Dépendance physique aux benzodiazépines dans un contexte traumatologique" [Benzodiazepine physical dependence in traumatology]. Annales Françaises d'Anesthésie et de Reanimation (frantsuz tilida). 3 (5): 383–4. doi:10.1016/S0750-7658(84)80078-7. PMID 6149713.
- ^ Turkington, Douglas; Gill, Paul (1989). "Mania induced by lorazepam withdrawal: A report of two cases". Affektiv buzilishlar jurnali. 17 (1): 93–5. doi:10.1016/0165-0327(89)90028-1. PMID 2525581.
- ^ Lapierre, YD; Labelle, A (1987). "Manic-like reaction induced by lorazepam withdrawal". Kanada psixiatriya jurnali. 32 (8): 697–8. doi:10.1177/070674378703200812. PMID 3690487. S2CID 8932926.
- ^ Kawajiri, M; Ohyagi, Y; Furuya, H; Araki, T; Inoue, N; Esaki, S; Yamada, T; Kira, J (2002). "A patient with Parkinson's disease complicated by hypothyroidism who developed malignant syndrome after discontinuation of etizolam". Rinsho Shinkeigaku. 42 (2): 136–9. PMID 12424963.
- ^ Strawn, Jeffrey; Keck Jr, PE; Caroff, SN (2007). "Neuroleptic Malignant Syndrome". Amerika psixiatriya jurnali. 164 (6): 870–6. doi:10.1176/ajp.2007.164.6.870. PMID 17541044.
- ^ Khan, A; Joyce, P; Jones, AV (1980). "Benzodiazepine withdrawal syndromes". Yangi Zelandiya tibbiyot jurnali. 92 (665): 94–6. PMID 6107888.
- ^ Peh, LH; Mahendran, R (1989). "Psychiatric complications of Erimin abuse". Singapur tibbiy jurnali. 30 (1): 72–3. PMID 2595393.
- ^ Fruensgaard, K. (1976). "Withdrawal Psychosis: A Study of 30 Consecutive Cases". Acta Psychiatrica Scandinavica. 53 (2): 105–18. doi:10.1111/j.1600-0447.1976.tb00065.x. PMID 3091. S2CID 1741725.
- ^ a b Einarson, A; Selby, P; Koren, G (2001). "Abrupt discontinuation of psychotropic drugs during pregnancy: Fear of teratogenic risk and impact of counselling". Psixiatriya va nevrologiya jurnali. 26 (1): 44–8. PMC 1408034. PMID 11212593.
- ^ Citrome, Leslie; Volavka, Jan (1999). "Violent Patients in the Emergency Setting". Shimoliy Amerikaning psixiatriya klinikalari. 22 (4): 789–801. doi:10.1016/S0193-953X(05)70126-X. PMID 10623971.
- ^ Dubuc, Bruno. "Neurotransmitters". The Brain from Top to Bottom. Arxivlandi asl nusxasidan 2013 yil 29 iyunda. Olingan 29 aprel 2013.
- ^ Tallman, J F; Gallager, D W (1985). "The Gaba-Ergic System: A Locus of Benzodiazepine Action". Nevrologiyani yillik sharhi. 8: 21–44. doi:10.1146/annurev.ne.08.030185.000321. PMID 2858999.
- ^ Schoch, P.; Richards, J. G.; Häring, P.; Takacs, B.; Stähli, C.; Staehelin, T.; Haefely, W.; Möhler, H. (1985). "Co-localization of GABAA receptors and benzodiazepine receptors in the brain shown by monoclonal antibodies". Tabiat. 314 (6007): 168–71. Bibcode:1985Natur.314..168S. doi:10.1038/314168a0. PMID 2983231. S2CID 1381200.
- ^ Vinkers, Christiaan H.; Olivier, Berend (2012). "Mechanisms Underlying Tolerance after Long-Term Benzodiazepine Use: A Future for Subtype-Selective GABAA Receptor Modulators?". Advances in Pharmacological Sciences. 2012: 1–19. doi:10.1155/2012/416864. PMC 3321276. PMID 22536226.
- ^ Study, R. E.; Barker, JL (1981). "Diazepam and (–)-pentobarbital: fluctuation analysis reveals different mechanisms for potentiation of γ-aminobutyric acid responses in cultured central neurons". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 78 (11): 7180–4. Bibcode:1981PNAS...78.7180S. doi:10.1073/pnas.78.11.7180. JSTOR 11434. PMC 349220. PMID 6273918.
- ^ a b v Bateson, A. (2002). "Basic Pharmacologic Mechanisms Involved in Benzodiazepine Tolerance and Withdrawal". Amaldagi farmatsevtika dizayni. 8 (1): 5–21. doi:10.2174/1381612023396681. PMID 11812247.
- ^ Tietz, EI; Rosenberg, HC; Chiu, TH (1986). "Autoradiographic localization of benzodiazepine receptor downregulation". Farmakologiya va eksperimental terapiya jurnali. 236 (1): 284–92. PMID 3001290.
- ^ Koob, G.; Bloom, F. (1988). "Cellular and molecular mechanisms of drug dependence". Ilm-fan. 242 (4879): 715–23. Bibcode:1988Sci...242..715K. doi:10.1126/science.2903550. PMID 2903550.
- ^ Meldrum, Brian S. (2000). "Glutamate as a Neurotransmitter in the Brain: Review of Physiology and Pathology". Oziqlanish jurnali. 130 (4): 1007S–15S. doi:10.1093 / jn / 130.4.1007s. PMID 10736372.
- ^ a b Stephens, D. N. (1995). "A glutamatergic hypothesis of drug dependence: extrapolations from benzodiazepine receptor ligands". Xulq-atvor farmakologiyasi. 6 (5): 425–46. doi:10.1097/00008877-199508000-00004. PMID 11224351.
- ^ a b Dunworth, Sarah J.; Mead, Andy N.; Stephens, David N. (2000). "Previous experience of withdrawal from chronic diazepam ameliorates the aversiveness of precipitated withdrawal and reduces withdrawal-induced c-fos expression in nucleus accumbens". Evropa nevrologiya jurnali. 12 (4): 1501–8. doi:10.1046/j.1460-9568.2000.00036.x. PMID 10762378. S2CID 42898466.
- ^ a b Rickels, Karl; Schweizer, E; Csanalosi, I; Case, WG; Chung, H (1988). "Long-term Treatment of Anxiety and Risk of Withdrawal: Prospective Comparison of Clorazepate and Buspirone". Umumiy psixiatriya arxivi. 45 (5): 444–50. doi:10.1001/archpsyc.1988.01800290060008. PMID 2895993.
- ^ Vorma, Helena; Naukkarinen, Hannu H.; Sarna, Seppo J.; Kuoppasalmi, Kimmo I. (2005). "Predictors of Benzodiazepine Discontinuation in Subjects Manifesting Complicated Dependence". Moddani ishlatish va uni noto'g'ri ishlatish. 40 (4): 499–510. doi:10.1081/JA-200052433. PMID 15830732. S2CID 1366333.
- ^ Smit, Devid E .; Wesson, Donald R. (1983). "Benzodiazepine Dependency Syndromes". Psixoaktiv dorilar jurnali. 15 (1–2): 85–95. doi:10.1080/02791072.1983.10472127. PMID 6136575.
- ^ Landry, MJ; Smith, DE; McDuff, DR; Baughman, OL (1992). "Benzodiazepine dependence and withdrawal: Identification and medical management". The Journal of the American Board of Family Practice. 5 (2): 167–75. PMID 1575069.
- ^ a b v Higgitt, A C; Lader, M H; Fonagy, P (1985). "Clinical management of benzodiazepine dependence". British Medical Journal. 291 (6497): 688–90. doi:10.1136/bmj.291.6497.688. PMC 1416639. PMID 2864096.
- ^ Lal R, Gupta S, Rao R, Kattimani S (2007). "Emergency management of substance overdose and withdrawal" (PDF). Substance Use Disorder. Jahon Sog'liqni saqlash tashkiloti (JSSV). p. 82. Arxivlangan asl nusxasi (PDF) 2010 yil 13 iyunda. Olingan 6 iyun 2009.
Generally, a longer-acting benzodiazepine such as chlordiazepoxide or diazepam is used and the initial dose titrated downward
- ^ Santos C, Olmedo RE (2017). "Sedative-Hypnotic Drug Withdrawal Syndrome: Recognition And Treatment". Shoshilinch tibbiy yordam amaliyoti. 19 (3): 1–20. PMID 28186869.
- ^ a b v d Parr, Jannette M.; Kavanagh, David J.; Cahill, Lareina; Mitchell, Geoffrey; Mcd Young, Ross McD. (2009). "Effectiveness of current treatment approaches for benzodiazepine discontinuation: A meta-analysis". Giyohvandlik. 104 (1): 13–24. doi:10.1111/j.1360-0443.2008.02364.x. PMID 18983627.
- ^ Fluyau, D; Revadigar, N; Manobianco, BE (May 2018). "Challenges of the pharmacological management of benzodiazepine withdrawal, dependence, and discontinuation". Psixofarmakologiyaning terapevtik yutuqlari. 8 (5): 147–168. doi:10.1177/2045125317753340. PMC 5896864. PMID 29713452.
- ^ Darker, Catherine D.; Sweeney, Brion P.; Barry, Joe M.; Farrell, Michael F.; Donnelly-Swift, Erica (2015). "Psychosocial interventions for benzodiazepine harmful use, abuse or dependence". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (5): CD009652. doi:10.1002/14651858.CD009652.pub2. hdl:2262/75957. ISSN 1469-493X. PMID 26106751.
- ^ Garfinkel, Doron; Zisapel, N; Wainstein, J; Laudon, M (1999). "Facilitation of Benzodiazepine Discontinuation by Melatonin: A New Clinical Approach". Ichki kasalliklar arxivi. 159 (20): 2456–60. doi:10.1001/archinte.159.20.2456. PMID 10665894.
- ^ Nakao, Mutsuhiro; Takeuchi, Takeaki; Nomura, Kyoko; Teramoto, Tamio; Yano, Eiji (2006). "Clinical application of paroxetine for tapering benzodiazepine use in non-major-depressive outpatients visiting an internal medicine clinic". Psixiatriya va klinik nevrologiya. 60 (5): 605–10. doi:10.1111/j.1440-1819.2006.01565.x. PMID 16958945. S2CID 44969935.
- ^ a b Rickels, K.; Schweizer, E.; Garcia España, F.; Case, G.; Demartinis, N.; Greenblatt, D. (1999). "Trazodone and valproate in patients discontinuing long-term benzodiazepine therapy: Effects on withdrawal symptoms and taper outcome". Psixofarmakologiya. 141 (1): 1–5. doi:10.1007/s002130050798. PMID 9952057. S2CID 12903042.
- ^ Fruensgaard, K (1977). "Withdrawal psychosis after drugs. Report of a consecutive material". Lger uchun Ugeskrift. 139 (29): 1719–22. PMID 898354.
- ^ Tagashira, Eijiro; Hiramori, Tameo; Urano, Tomoko; Nakao, Kenzo; Yanaura, Saizo (1981). "Enhancement of drug withdrawal convulsion by combinations of phenobarbital and antipsychotic agents". Yapon farmakologiya jurnali. 31 (5): 689–99. doi:10.1254 / jjp.31.689. PMID 6118452.
- ^ Bobolakis, Ioannis (2000). "Neuroleptic Malignant Syndrome After Antipsychotic Drug Administration During Benzodiazepine Withdrawal". Klinik psixofarmakologiya jurnali. 20 (2): 281–3. doi:10.1097/00004714-200004000-00033. PMID 10770479.
- ^ Randall, Michael D; Neil, Karen E (February 2004). "5". Kasalliklarni boshqarish (1 nashr). Farmatsevtika matbuoti. p. 62. ISBN 978-0-85369-523-3. Olingan 1 iyun 2009.
- ^ Ebadi, Manuchair (23 October 2007). "Alphabetical presentation of drugs". Desk Reference for Clinical Pharmacology (2-nashr). AQSh: CRC Press. p. 512. ISBN 978-1-4200-4743-1.
- ^ Clinical Guide to the Diagnosis and Treatment of Mental Disorders By Michael B. First, Allan Tasman, p. 242
- ^ a b v d Lader, Malcolm; Tylee, Andre; Donoghue, John (2009). "Withdrawing Benzodiazepines in Primary Care". CNS dorilar. 23 (1): 19–34. doi:10.2165/0023210-200923010-00002. PMID 19062773. S2CID 113206.
- ^ Higgitt, A.; Fonagi, P .; Lader, M. (2009). "Benzodiazepinlarga nisbatan bag'rikenglikning tabiiy tarixi". Psixologik tibbiyot. Monograph Supplement. 13: 1–55. doi:10.1017 / S0264180100000412. PMID 2908516.
- ^ "Wellbutrin XL Prescribing Information" (PDF). GlaxoSmithKline. Dekabr 2008. Arxivlangan asl nusxasi (PDF) 2009 yil 26 martda. Olingan 16 yanvar 2010.
- ^ Seale, Thomas W.; Carney, John M.; Rennert, Owen M.; Flux, Marinus; Skolnick, Phil (1987). "Coincidence of seizure susceptibility to caffeine and to the benzodiazepine inverse agonist, DMCM, in SWR and CBA inbred mice". Farmakologiya Biokimyo va o'zini tutish. 26 (2): 381–7. doi:10.1016/0091-3057(87)90133-X. PMID 3575358. S2CID 30168114.
- ^ Schweizer, Edward; Rickels, K; Case, WG; Greenblatt, DJ (1990). "Long-term Therapeutic Use of Benzodiazepines: II. Effects of Gradual Taper". Umumiy psixiatriya arxivi. 47 (10): 908–15. doi:10.1001/archpsyc.1990.01810220024003. PMID 2222130.
- ^ a b Denis, Cecile; Fatseas, Melina; Lavie, Estelle; Auriacombe, Marc (2006). Denis, Cecile (ed.). "Pharmacological interventions for benzodiazepine mono-dependence management in outpatient settings". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (3): CD005194. doi:10.1002/14651858.CD005194.pub2. PMID 16856084. (Orqaga tortildi, qarang doi:10.1002/14651858.cd005194.pub3. Agar bu tortib olingan qog'ozga qasddan keltirilgan bo'lsa, uni o'zgartiring
{{Orqaga olindi}}bilan{{Orqaga olindi| qasddan = ha}}.) - ^ Gerra, G.; Zaimovic, A.; Giusti, F .; Moi, G.; Brewer, C. (2002). "Intravenous flumazenil versus oxazepam tapering in the treatment of benzodiazepine withdrawal: A randomized, placebo-controlled study". Addiction Biology. 7 (4): 385–95. doi:10.1080/1355621021000005973. PMID 14578014. S2CID 21255719.
- ^ Little, H.J. (1991). "The benzodiazepines: Anxiolytic and withdrawal effects". Neyropeptidlar. 19: 11–4. doi:10.1016/0143-4179(91)90077-V. PMID 1679209. S2CID 13734753.
- ^ a b L. Saxon, S. Borg & A. J. Hiltunen (Avgust 2010). "Reduction of aggression during benzodiazepine withdrawal: effects of flumazenil". Farmakologiya Biokimyo va o'zini tutish. 96 (2): 148–151. doi:10.1016/j.pbb.2010.04.023. PMID 20451546. S2CID 41351863.
- ^ Lader, M. H.; Morton, S. V. (1992). "A pilot study of the effects of flumazenil on symptoms persisting after benzodiazepine withdrawal". Psixofarmakologiya jurnali. 6 (3): 357–63. doi:10.1177/026988119200600303. PMID 22291380. S2CID 23530701.
- ^ Roche USA (October 2007). "Romazicon" (PDF). Roche Pharmaceuticals USA. Arxivlandi asl nusxasi (PDF) 2008 yil 25 iyunda.
- ^ Unseld, E; G Ziegler; A Gemeinhardt; U Janssen; U Klotz (July 1990). "Possible interaction of fluoroquinolones with the benzodiazepine-GABAA-receptor complex (summary)". Britaniya klinik farmakologiya jurnali. 30 (1): 63–70. doi:10.1111/j.1365-2125.1990.tb03744.x. PMC 1368276. PMID 2167717.
- ^ Ashton, Heather (April 2011). "The Ashton Manual Supplement". Benzodiazepines: How They Work & How to Withdraw. benzo.org.uk.
- ^ Kamath, Ashwin (2013). "Fluoroquinolone Induced Neurotoxicity: A Review" (PDF). Journal of Advanced Pharmacy Education & Research. 3 (1): 16-19. Arxivlandi asl nusxasi (PDF) 2014 yil 11 fevralda. Olingan 17 oktyabr 2015.
- ^ McConnell, John Girvan (2008). "Benzodiazepine tolerance, dependency, and withdrawal syndromes and interactions with fluoroquinolone antimicrobials". Britaniya umumiy amaliyot jurnali. 58 (550): 365–6. doi:10.3399/bjgp08X280317. PMC 2435654. PMID 18482496.
- ^ Unseld, E; Ziegler, G; Gemeinhardt, A; Yanssen, U; Klotz, U (1990). "Possible interaction of fluoroquinolones with the benzodiazepine-GABAA- receptor complex". Britaniya klinik farmakologiya jurnali. 30 (1): 63–70. doi:10.1111/j.1365-2125.1990.tb03744.x. PMC 1368276. PMID 2167717.
- ^ Sternbach, Harvey; State, Rosanne (1997). "Antibiotics: Neuropsychiatric Effects and Psychotropic Interactions". Garvard psixiatriyasini ko'rib chiqish. 5 (4): 214–26. doi:10.3109/10673229709000304. PMID 9427014. S2CID 21259675.
- ^ Dori vositalari xavfsizligi qo'mitasi; Medicines and Healthcare products Regulatory Agency (2008). "Quinolones". Birlashgan Qirollik: Britaniya milliy formulasi. Arxivlandi asl nusxasi 2012 yil 30 iyunda. Olingan 16 fevral 2009.
- ^ Wong, PT (1993). "Interactions of indomethacin with central GABA systems". Archives Internationales de Pharmacodynamie et de Terapie. 324: 5–16. PMID 8297186.
- ^ Delanty, Norman (November 2001). "Medication associated seizures". Seizures: Medical Causes and Management. Humana Press. 152-153 betlar. ISBN 978-0-89603-827-1.
- ^ Green, M. A.; Halliwell, R. F. (1997). "Selective antagonism of the GABAAreceptor by ciprofloxacin and biphenylacetic acid". Britaniya farmakologiya jurnali. 122 (3): 584–90. doi:10.1038/sj.bjp.0701411. PMC 1564969. PMID 9351519.
- ^ Auta, J; Kosta, E; Devis, J; Guidotti, A (2005). "Imidazenil: An antagonist of the sedative but not the anticonvulsant action of diazepam". Neyrofarmakologiya. 49 (3): 425–9. doi:10.1016/j.neuropharm.2005.04.005. PMID 15964602. S2CID 44619421.
- ^ Sallivan, Mark; Toshima, Michelle; Lynn, Pamela; Roy-Byrne, Peter (1993). "Phenobarbital Versus Clonazepam for Sedative-Hypnotic Taper in Chronic Pain Patients: A Pilot Study". Klinik psixiatriya yilnomalari. 5 (2): 123–8. doi:10.3109/10401239309148974. PMID 8348204.
- ^ Ray Baker. "Dr Ray Baker's Article on Addiction: Benzodiazepines in Particular". Olingan 14 fevral 2009.
- ^ Oulis, P.; Konstantakopoulos, G. (2010). "Pregabalin in the treatment of alcohol and benzodiazepines dependence". CNS nevrologiya va terapiya. 16 (1): 45–50. doi:10.1111/j.1755-5949.2009.00120.x. PMC 6493856. PMID 20070788.
- ^ Oulis, P.; Konstantakopoulos, G. (July 2012). "Efficacy and safety of pregabalin in the treatment of alcohol and benzodiazepine dependence". Tergov narkotiklari bo'yicha mutaxassislarning fikri. 21 (7): 1019–29. doi:10.1517/13543784.2012.685651. PMID 22568872. S2CID 24354141.
- ^ Zitman, F. G.; Couvée, JE (2001). "Chronic benzodiazepine use in general practice patients with depression: An evaluation of controlled treatment and taper-off: Report on behalf of the Dutch Chronic Benzodiazepine Working Group". Britaniya psixiatriya jurnali. 178 (4): 317–24. doi:10.1192/bjp.178.4.317. PMID 11282810.
- ^ Tönne, U.; Hiltunen, A. J.; Vikander, B.; Engelbrektsson, K.; Bergman, H .; Bergman, I.; Leifman, H.; Borg, S. (1995). "Neuropsychological changes during steady-state drug use, withdrawal and abstinence in primary benzodiazepine-dependent patients". Acta Psychiatrica Scandinavica. 91 (5): 299–304. doi:10.1111/j.1600-0447.1995.tb09786.x. PMID 7639085. S2CID 9339677.
- ^ Kan, CC; Mickers, FC; Barnhoorn, D (2006). "Short- and long-term results of a systematic benzodiazepine discontinuation programme for psychiatric patients". Tijdschrift voor Psychiatrie. 48 (9): 683–93. PMID 17007474.
- ^ Jørgensen, VR (2009). "Benzodiazepine reduction does not imply an increased consumption of antidepressants. A survey of two medical practices". Lger uchun Ugeskrift. 171 (41): 2999–3003. PMID 19814928.
- ^ Lal R, Gupta S, Rao R, Kattimani S (2007). "Emergency management of substance overdose and withdrawal" (PDF). Substance Use Disorder. Jahon sog'liqni saqlash tashkiloti. p. 82. Arxivlangan asl nusxasi (PDF) 2010 yil 13 iyunda. Olingan 6 iyun 2009.
Generally, a longer-acting benzodiazepine such as chlordiazepoxide or diazepam is used and the initial dose titrated downward
- ^ Noyes, Russell; Perry, Paul J.; Crowe, Raymond R.; Coryell, William H.; Clancy, John; Yamada, Thoru; Gabel, Janelle (1986). "Seizures Following the Withdrawal of Alprazolam". Asab va ruhiy kasalliklar jurnali. 174 (1): 50–2. doi:10.1097/00005053-198601000-00009. PMID 2867122.
- ^ Noyes Jr, R; Clancy, J; Coryell, WH; Crowe, RR; Chaudhry, DR; Domingo, DV (1985). "A withdrawal syndrome after abrupt discontinuation of alprazolam". Amerika psixiatriya jurnali. 142 (1): 114–6. doi:10.1176/ajp.142.1.114. PMID 2857066.
- ^ Rickels, Karl; Schweizer, E; Case, WG; Greenblatt, DJ (1990). "Long-term Therapeutic Use of Benzodiazepines: I. Effects of Abrupt Discontinuation". Umumiy psixiatriya arxivi. 47 (10): 899–907. doi:10.1001/archpsyc.1990.01810220015002. PMID 2222129.
- ^ Neale, G; Smith, AJ (2007). "Self-harm and suicide associated with benzodiazepine usage". Britaniya umumiy amaliyot jurnali. 57 (538): 407–8. PMC 2047018. PMID 17504594.
- ^ a b Soyka (2017), Treatment of Withdrawal Symptoms, p. 1151 cited "Drug misuse and dependence: UK guidelines on clinical management" (PDF). London: Department of Health (England), Scottish Government, Welsh Assembly Government, Northern Ireland Executive. 2017 yil.
- ^ Soyka (2017), Treatment of Withdrawal Symptoms, p. 1151 cited Soyka, M (2015). Medikamentenabhängigkeit. Stuttgart, Germany: Schattauer.
- ^ Soyka (2017), Treatment of Withdrawal Symptoms, p. 1151
- ^ Curran, H. V.; Bond, A.; O'Sullivan, G.; Bryus, M.; Marks, I.; Lelliot, P.; Shine, P.; Lader, M. (2009). "Memory functions, alprazolam and exposure therapy: A controlled longitudinal study of agoraphobia with panic disorder". Psixologik tibbiyot. 24 (4): 969–76. doi:10.1017/S0033291700029056. PMID 7892364.
- ^ Busto, Usoa; Fornazzari, Luis; Naranjo, Claudio A. (1988). "Protracted Tinnitus after Discontinuation of Long-Term Therapeutic Use of Benzodiazepines". Klinik psixofarmakologiya jurnali. 8 (5): 359–362. doi:10.1097/00004714-198810000-00010. PMID 2903182.
- ^ Higgitt, A.; Fonagi, P .; Toone, B.; Shine, P. (1990). "The prolonged benzodiazepine withdrawal syndrome: Anxiety or hysteria?". Acta Psychiatrica Scandinavica. 82 (2): 165–8. doi:10.1111/j.1600-0447.1990.tb01375.x. PMID 1978465. S2CID 41458371.
- ^ Ashton CH (March 1995). "Protracted Withdrawal From Benzodiazepines: The Post-Withdrawal Syndrome". Psixiatrik yilnomalar. benzo.org.uk. 25 (3): 174–179. doi:10.3928/0048-5713-19950301-11.
- ^ Barker, M; Greenwood, KM; Jackson, M; Crowe, SF (2004). "Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: A meta-analysis". Klinik neyropsixologiya arxivi. 19 (3): 437–54. doi:10.1016/S0887-6177(03)00096-9. PMID 15033227.
- ^ Hood HM, Metten P, Crabbe JC, Buck KJ (February 2006). "Fine mapping of a sedative-hypnotic drug withdrawal locus on mouse chromosome 11". Genlar, miya va o'zini tutish. 5 (1): 1–10. doi:10.1111/j.1601-183X.2005.00122.x. PMID 16436183. S2CID 27844115.
- ^ Vorma, H; Naukkarinen, Hh; Sarna, Sj; Kuoppasalmi, Ki (2005). "Predictors of benzodiazepine discontinuation in subjects manifesting complicated dependence". Moddani ishlatish va uni noto'g'ri ishlatish. 40 (4): 499–510. doi:10.1081/JA-200052433. PMID 15830732. S2CID 1366333.
- ^ McElhatton, Patricia R. (1994). "Homiladorlik va laktatsiya davrida benzodiazepinni qo'llash ta'siri". Reproduktiv toksikologiya. 8 (6): 461–75. doi:10.1016/0890-6238(94)90029-9. PMID 7881198.
- ^ a b v Birchley, Giles (2009). "Opioid and benzodiazepine withdrawal syndromes in the paediatric intensive care unit: A review of recent literature". Nursing in Critical Care. 14 (1): 26–37. doi:10.1111/j.1478-5153.2008.00311.x. PMID 19154308.
- ^ Fontela, Patrícia Scolari; Fontela, Aline; Moraes, Fabrício; Da Silva, Ricardo Bernardi; Sober, Roberta B.; Noer, Francisco; Bruno, Paulo; Einloft, Ana; Garcia, Pedro Celiny Ramos; Piva, Jefferson P. (2003). "Sedation and analgesia in children submitted to mechanical ventilation could be overestimated?". Jornal de Pediatriya. 79 (4): 343–8. doi:10.2223/JPED.1046. PMID 14513134.
- ^ Playfor, Stephen; Jenkins, Ian; Boyles, Carolyne; Choonara, Imti; Davies, Gerald; Haywood, Tim; Hinson, Gillian; Mayer, Anton; Morton, Neil; Ralph, Tanya; Wolf, Andrew; United Kingdom Paediatric Intensive Care Society Sedation; Analgesia Neuromuscular Blockade Working Group (2006). "Consensus guidelines on sedation and analgesia in critically ill children". Reanimatsiya tibbiyoti. 32 (8): 1125–36. doi:10.1007/s00134-006-0190-x. PMID 16699772. S2CID 8518882.
- ^ Ista, Erwin; Van Dijk, Monique; Gamel, Claudia; Tibboel, Dick; De Hoog, Matthijs (2007). "Withdrawal symptoms in children after long-term administration of sedatives and/or analgesics: A literature review. 'Assessment remains troublesome'". Reanimatsiya tibbiyoti. 33 (8): 1396–406. doi:10.1007/s00134-007-0696-x. PMID 17541548.
- ^ a b v d e Curran, HV; Collins, R; Fletcher, S; Kee, SC; Woods, B; Iliffe, S (2003). "Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life" (PDF). Psixologik tibbiyot. 33 (7): 1223–37. doi:10.1017/S0033291703008213. PMID 14580077.
- ^ Salzman, Carl (15 May 2004). Clinical geriatric psychopharmacology (4-nashr). AQSh: Lippincott Uilyams va Uilkins. pp. 450–3. ISBN 978-0-7817-4380-8.
Tashqi havolalar
| Tasnifi |
|---|

