Psixoz - Psychosis
| Psixoz | |
|---|---|
| Boshqa ismlar | Psixotik tanaffus |
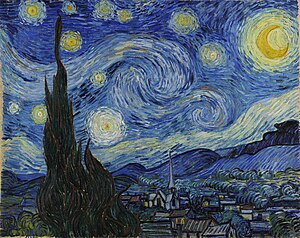 | |
| Van Gog "s Yulduzli tun, 1889 yildan boshlab, psixoz bilan paydo bo'lishi mumkin bo'lgan yorug'lik va rangdagi o'zgarishlarni ko'rsatadi.[1][2][3] | |
| Mutaxassisligi | Psixiatriya, klinik psixologiya |
| Alomatlar | Soxta e'tiqodlar, boshqalar ko'rmaydigan yoki eshitmaydigan narsalarni ko'rish yoki eshitish, nomuvofiq nutq[4] |
| Murakkabliklar | O'z-o'ziga ziyon, o'z joniga qasd qilish[5] |
| Sabablari | Ruhiy kasallik (shizofreniya, bipolyar buzilish ), uyqusizlik, ba'zi tibbiy sharoitlar, aniq dorilar, giyohvand moddalar (shu jumladan spirtli ichimliklar va nasha )[4] |
| Davolash | Antipsikotiklar, maslahat, ijtimoiy qo'llab-quvvatlash[5] |
| Prognoz | Sababga bog'liq[5] |
| Chastotani | Bir vaqtning o'zida odamlarning 3% (AQSh)[4] |
Psixoz ning anormal holatidir aql bu nima ekanligini aniqlashda qiyinchiliklarga olib keladi haqiqiy va nima haqiqiy emas.[4] Alomatlar o'z ichiga olishi mumkin xayollar va gallyutsinatsiyalar.[4] Boshqa alomatlar o'z ichiga olishi mumkin nomuvofiq nutq va vaziyatga mos bo'lmagan xatti-harakatlar.[4] Shuningdek, bo'lishi mumkin uyqu muammolari, ijtimoiy chekinish, motivatsiya etishmasligi va qiyinchiliklarni amalga oshirish kundalik faoliyat.[4] Psixoz jiddiy oqibatlarga olib kelishi mumkin.[6]
Psixoz turli xil sabablarga ega.[4] Bunga quyidagilar kiradi ruhiy kasallik, kabi shizofreniya yoki bipolyar buzilish, uyqusizlik, ba'zi tibbiy sharoitlar, aniq dorilar va shunga o'xshash dorilar spirtli ichimliklar yoki nasha.[4] Sifatida tanilgan bir turi tug'ruqdan keyingi psixoz, tug'ilgandan keyin paydo bo'lishi mumkin.[7] The neyrotransmitter dopamin rol o'ynaydi deb ishoniladi.[8] O'tkir psixoz psixiatrik holatdan kelib chiqsa, birlamchi, tibbiy holat tufayli kelib chiqsa, ikkinchi darajali hisoblanadi.[9] Ruhiy kasallik diagnostikasi boshqa mumkin bo'lgan sabablarni istisno qilishni talab qiladi.[10] Tekshirish uchun sinov o'tkazilishi mumkin markaziy asab tizimi kasalliklar, toksinlar yoki boshqa sog'liq muammolari sabab bo'ladi.[11]
Davolashni o'z ichiga olishi mumkin antipsikotik dori, maslahat va ijtimoiy qo'llab-quvvatlash.[4][5] Erta davolanish natijalarni yaxshilaydi.[4] Dori-darmonlar o'rtacha darajada ta'sir qiladi.[12][13] Natijalar asosiy sababga bog'liq.[5] Qo'shma Shtatlarda odamlarning taxminan 3% hayotining bir qismida psixozni rivojlantiradi.[4] Vaziyat miloddan avvalgi kamida 4-asrdan boshlab tasvirlangan Gippokrat va ehtimol miloddan avvalgi 1500 yilda Misrda Ebers Papirus.[14][15]
Belgilari va alomatlari
Gallyutsinatsiyalar
A gallyutsinatsiya tashqi stimullar bo'lmagan taqdirda hissiy idrok sifatida aniqlanadi. Halüsinasyonlar farq qiladi xayollar va tashqi ogohlantirishlarni noto'g'ri qabul qilish bo'lgan pertseptiv buzilishlar. Gallyutsinatsiyalar har qanday hissiyotlarda paydo bo'lishi va deyarli har qanday shaklda bo'lishi mumkin. Ular oddiy tuyg'ulardan (yorug'lik, ranglar, tovushlar, ta'mlar yoki hidlar kabi) yoki batafsil tajribalardan (masalan, hayvonlar va odamlarni ko'rish va ular bilan muloqot qilishdan) iborat bo'lishi mumkin. ovozlarni eshitish va murakkab teginish hissiyotlariga ega bo'lish). Halüsinasyonlar odatda jonli va boshqarib bo'lmaydigan sifatida tavsiflanadi.[16] Eshitish gallyutsinatsiyalari, xususan, ovozlarni eshitish tajribalari - bu psixozning eng keng tarqalgan va ko'pincha ko'zga tashlanadigan xususiyati.
Umumiy aholining 15 foizigacha eshitish gallyutsinatsiyasini boshdan kechirishi mumkin (ammo barchasi hammasi psixozga bog'liq emas). Shizofreniya bilan og'rigan bemorlarda eshitish gallyutsinatsiyalarining tarqalishi odatda 70% ni tashkil qiladi, ammo 98% gacha ko'tarilishi mumkin. Bipolyar buzilishning tarqalishi 11% dan 68% gacha.[17] 20-asrning boshlarida eshitish gallyutsinatsiyalari chastotasi bo'yicha vizual gallyutsinatsiyalardan keyin ikkinchi o'rinda turardi, ammo hozirgi vaqtda ular shizofreniya kasalligining eng keng tarqalgan ko'rinishidir, garchi bu ko'rsatkichlar madaniyatlar va mintaqalar o'rtasida farq qilsa. Eshitish gallyutsinatsiyalari odatda tushunarli ovozlardir. Ovozlar mavjud bo'lganda, o'rtacha raqam uchga baholandi. Tarkib, chastota kabi, ayniqsa madaniyatlar va demografiya bo'yicha sezilarli darajada farq qiladi. Eshitish gallyutsinatsiyasini boshdan kechirgan odamlar ovoz balandligini, kelib chiqadigan joyni tez-tez aniqlay olishadi va ovozlar uchun shaxsiyatlarga qarab turishlari mumkin. G'arb madaniyati ko'pincha gunoh bilan bog'liq diniy tarkibga oid eshitish tajribalari bilan bog'liq. Gallyutsinatsiyalar odamni aldanishlar bilan birlashganda potentsial xavfli ishni qilishni buyurishi mumkin.[18]
Ekstrakampin gallyutsinatsiyalari bu hissiy apparatdan tashqaridagi hislar, masalan, tovush tizza orqali seziladi,[18] yoki vizual ekstrakampin gallyutsinatsiyasi, kimdir sizga yaqin ekanligini sezadi, u erda yo'q.[19]
Vizual gallyutsinatsiyalar shizofreniya bilan kasallangan odamlarning taxminan uchdan birida uchraydi, ammo 55% gacha bo'lgan ko'rsatkichlar qayd etilgan. Bipolyar buzilishning tarqalishi 15% atrofida. Tarkib tez-tez jonlantiruvchi narsalarni o'z ichiga oladi, ammo yorug'lik, soyalash, chiziqlar yoki chiziqlar o'zgarishi kabi sezuvchanlik anormalliklari kuzatilishi mumkin. Vizual anormalliklarga zid bo'lishi mumkin proprioseptiv ma'lumot va vizyonlarda erni egish kabi tajribalar bo'lishi mumkin. Liliput gallyutsinatsiyalari shizofreniyada kamroq uchraydi va turli xillarda tez-tez uchraydi ensefalopatiya kabi pedunkulyar gallyutsinoz.[18]
Ventseral gallyutsinatsiya, shuningdek, sintetik gallyutsinatsiya deb ataladi, stimul bo'lmaganida visseral hislar bilan tavsiflanadi. Senestetik gallyutsinatsiyalar yonish hissi yoki ichki organlarning qayta joylashishini o'z ichiga olishi mumkin.[18]
Xayollar
Psixoz o'z ichiga olishi mumkin xayoliy e'tiqodlar. Odatda, aldanish kuchli ziddiyatli dalillarga qaramay saqlanib kelinayotgan aniqlik hissi sifatida ta'riflanadi. Xayollar kontekst va madaniyatga bog'liqdir: tanqidiy faoliyatni inhibe qiladigan va bir populyatsiyada keng tarqalgan deb hisoblanadigan e'tiqod boshqasida yoki keyinchalik o'sha populyatsiyada keng tarqalgan (va hatto moslashuvchan) bo'lishi mumkin. Beri normativ qarashlarning o'zlari mavjud dalillarga zid bo'lishi mumkin, e'tiqod aldangan deb hisoblash uchun madaniy me'yorlarga zid bo'lmasligi kerak.
Shizofreniya tarqalishi odatda kamida 90%, bipolyar buzuqlikda esa 50% atrofida hisoblanadi.
DSM-5 ba'zi bir xayollarni "g'alati" deb ta'riflaydi, agar ular aniq ishonib bo'lmaydigan bo'lsa yoki atrofdagi madaniy kontekst bilan mos kelmasa. G'alati xayolparastlik tushunchasi ko'plab tanqidlarga ega, eng taniqli, uning mavjudligini baholash, hatto o'qitilgan odamlar orasida ham juda ishonchli emas.[18]
Yolg'onchilik turli xil tematik tarkibni o'z ichiga olishi mumkin. Eng keng tarqalgan turi a ta'qib qiluvchi aldanish, unda biron bir shaxs ularga zarar etkazishga urinayotganiga ishonadi. Boshqalar kiradi ma'lumotnomaning xayoliyligi (biron bir tajribaning ba'zi bir elementlari qasddan va aniq bir harakat yoki boshqa biron bir tashkilotning xabarini anglatadi degan ishonch), ulug'vorlikning xayollari (inson o'ziga xos kuchga yoki ta'sir doirasiga ega ekanligiga ishonish) efirga uzatish (kishining fikrlari eshitilishi mumkinligiga ishonch) va fikrni kiritish (birovning fikri o'ziniki emasligiga ishonch).
Xayollarning mavzusi ma'lum bir vaqt va joyda mavjud madaniyatni aks ettiradi. Masalan, AQShda, 1900-yillarning boshlarida sifilis keng tarqalgan mavzu edi, Ikkinchi jahon urushi paytida Germaniya, sovuq urush paytida kommunistlar va so'nggi yillarda texnologiya diqqat markazida bo'ldi. [20] Ba'zi psixologlar, masalan, amaliyot bilan shug'ullanadiganlar Dialogni oching usuli psixozning mazmuni qisman psixoz uchun javobgar bo'lishi mumkin bo'lgan asosiy fikrlash jarayonini anglatadi, [21] Garchi qabul qilingan tibbiy pozitsiya psixoz miya buzilishi tufayli yuzaga keladi.
Tarixiy jihatdan, Karl Yaspers tasniflangan psixotik aldanishlar birlamchi va ikkilamchi turlari. Birlamchi xayollarga to'satdan kelib chiqadigan va odatdagi aqliy jarayonlar nuqtai nazaridan tushunib bo'lmaydigan deb ta'rif berilgan bo'lsa, ikkilamchi xayollarga odatda odamning kelib chiqishi yoki hozirgi holati (masalan, etnik kelib chiqishi; shuningdek, diniy, xurofot yoki siyosiy e'tiqod) ta'sirida tushuniladi.[22]
Organizatsiya
Disorganizatsiya uyushmagan nutq yoki fikrlash va qo'pol ravishda tartibsiz harakatga bo'linadi. Uyushmagan nutq yoki fikrlash, shuningdek chaqiriladi rasmiy fikr buzilishi, nutqdan kelib chiqadigan fikrlashning disorganizatsiyasi. Noto'g'ri nutqning xususiyatlariga relsdan chiqish yoki bo'shashgan assotsiatsiya deb ataladigan tez o'zgaruvchan mavzular kiradi; tangensial fikrlash deb ataladigan, bog'liq bo'lmagan mavzularga o'tish; chaqirilgan tushunarsiz nutq salat so'zi yoki nomuvofiqlik. Tartibsiz vosita harakati takrorlanadigan, g'alati yoki ba'zan maqsadsiz harakatni o'z ichiga oladi. Disorganizatsiyalangan motorli xatti-harakatlar kamdan-kam hollarda katatoniyani o'z ichiga oladi va bu tarixiy jihatdan taniqli alomat bo'lsa-da, bugungi kunda u kamdan-kam uchraydi. Bu tarixan qo'llanilgan muolajalar bilan bog'liqmi yoki yo'qligi noma'lum.[18][16]
Katatoniya haqiqat tajribasi umuman buzilgan deb hisoblanadigan chuqur hayajonlangan holatni tavsiflaydi. Katatonik xulq-atvorning ikkita asosiy ko'rinishi mavjud. Klassik taqdimot - bu uyg'otganda hech qanday harakat qilmaydigan yoki dunyo bilan aloqa qilmaydigan odam. Ushbu turdagi katatoniya bilan birga keladi mumi moslashuvchanligi. Mumli moslashuvchanlik - bu katatonik odam tanasining bir qismini jismonan harakatga keltirishi va u g'alati va boshqa funktsiyalarga ega bo'lmagan taqdirda ham odam o'z holatida qolishi (masalan, odamning qo'lini havoda tekis ko'tarish va qo'l shu erda qolishi).
Katatoniyaning boshqa turi - yuqorida tavsiflangan chuqur hayajonlangan holatning tashqi ko'rinishidir. Bu haddan tashqari va maqsadsiz motorli xatti-harakatlarni, shuningdek haqiqatning buzilmagan tajribasini oldini oladigan haddan tashqari aqliy mashg'ulotni o'z ichiga oladi. Masalan, alomatlar paydo bo'lishidan oldin odamga xos bo'lmagan, ruhiy mashg'ulot darajasiga ega bo'lgan boshqa narsalarni istisno qilish uchun aylanada juda tez yuradigan kishi (vaziyatga bog'liq bo'lgan narsaga e'tibor bermaslik kerak). Katatoniyaning har ikkala turida, odatda, ularning tashqarisida sodir bo'ladigan narsalarga munosabat yo'q. Katatonik ajitatsiyani qattiq bipolyar maniyadan ajratish muhimdir, garchi kimdir ikkalasida ham bo'lishi mumkin.
Salbiy alomatlar
Salbiy alomatlar orasida emotsional ifodaning pasayishi, motivatsiyaning pasayishi va o'z-o'zidan nutqni qisqartirish. Jabrlangan odamlarda qiziqish va o'z-o'zidan paydo bo'ladigan narsa yo'q zavqni his qila olmaslik.[23]
O'smirlarda psixoz
O'smirlarda psixoz kam uchraydi.[6] Psixozga chalingan yoshlar atrofdagi dunyo bilan aloqa qilishda muammolarga duch kelishlari va gallyutsinatsiyalar va / yoki xayollarga duch kelishlari mumkin.[6] Psixoz bilan og'rigan o'spirinlarda bilim etishmovchiligi ham bo'lishi mumkin, bu esa yoshlarning ijtimoiylashuvi va ishlashini qiyinlashtirishi mumkin.[6] Mumkin bo'lgan buzilishlarga aqliy ishlov berish tezligi, diqqatni chalg'itmasdan yo'naltirish qobiliyati kiradi (diqqat oralig'i ) va ular bilan bog'liq muammolar og'zaki xotira.[6]
Sabablari
Psixoz belgilari jiddiy sabab bo'lishi mumkin psixiatrik kasalliklar kabi shizofreniya, bir qator tibbiy kasalliklar va travma. Psixoz ham vaqtinchalik yoki vaqtinchalik bo'lishi mumkin va dori vositalari yoki giyohvand moddalarni suiiste'mol qilish (moddaning ta'sirida bo'lgan psixoz ).
Oddiy holatlar
Qisqa gallyutsinatsiyalar psixiatrik kasalligi bo'lmaganlarda kam uchraydi. Sabablari yoki qo'zg'atuvchilariga quyidagilar kiradi:[24]
- Uxlab qolish va uyg'onish: gipnagogik va gipnopompik gallyutsinatsiyalar, bu butunlay normaldir[25]
- Yordam, unda vafot etgan yaqin kishining gallyutsinatsiyalari keng tarqalgan[24]
- Og'ir uyqusizlik[26][27][28]
- Stress[29]
Travma
Shikastlangan hayotiy hodisalar psixotik simptomlarni rivojlanish xavfi bilan bog'liq.[30] Bolalik travması, ayniqsa, o'spirin va kattalar psixozining bashoratchisi ekanligi aniqlandi.[31] Psixotik alomatlari bo'lgan odamlarning taxminan 65% bolalik travmatizmini boshdan kechirgan (masalan, jismoniy yoki jinsiy zo'ravonlik, jismoniy yoki hissiy e'tiborsizlik).[32] Psixozga qarshi individual zaiflikning kuchayishi, ayniqsa, sezgir rivojlanish davrida, kelajakdagi psixotik alomatlarning paydo bo'lishiga yordam beradigan travmatik tajribalar bilan o'zaro ta'sir qilishi mumkin.[31] Muhimi, travmatik hayot hodisalari va psixotik alomatlar o'rtasidagi munosabatlar dozaga bog'liq bo'lib, unda ko'plab shikastlanishlar sodir bo'ladigan hayotiy hodisalar to'planib, simptomning namoyon bo'lishi va zo'ravonligini kuchaytiradi.[30][31] Bu travmanın oldini olish va erta aralashuv psixotik buzilishlarni kamaytirish va uning ta'sirini yaxshilash uchun muhim maqsad bo'lishi mumkinligini ko'rsatadi.[30]
Ruhiy kasallik
Tashxisiy nuqtai nazardan, organik buzilishlar miyaga ta'sir qiladigan jismoniy kasallik (ya'ni boshqa holatlarga bog'liq bo'lgan psixiatrik kasalliklar) tufayli yuzaga kelgan deb hisoblar edilar, funktsional buzilishlar esa jismoniy buzilishlar bo'lmagan taqdirda ong faoliyatining buzilishi deb hisoblanardi (ya'ni , asosiy psixologik yoki psixiatrik kasalliklar). An'anaviy ravishda funktsional deb hisoblangan kasalliklarda nozik jismoniy anormallik aniqlangan shizofreniya. The DSM-IV-TR funktsional / organik farqlanishdan qochadi va buning o'rniga an'anaviy psixotik kasalliklar, umumiy tibbiy holatlar sababli psixoz va moddaning ta'sirida bo'lgan psixozlarni ro'yxatlaydi.
Psixozning birlamchi psixiatrik sabablari quyidagilarni o'z ichiga oladi:[33][34][24]
- shizofreniya va shizofreniform buzilish
- affektiv (kayfiyat) buzilishlar, shu jumladan katta depressiya, va qattiq depressiya yoki mani bipolyar buzilish (manik depressiya). Depressiya sharoitida psixotik epizodni boshdan kechirayotgan odamlar quvg'inni boshdan kechirishlari mumkin o'zini ayblash aldanishlar yoki gallyutsinatsiyalar, maniya sharoitida psixotik epizodni boshdan kechirayotganlar esa ulkan xayolotlarni shakllantirishi mumkin.
- shizoaffektiv buzilish, shizofreniya va kayfiyat buzilishining alomatlarini o'z ichiga olgan
- qisqa psixotik buzilish yoki o'tkir / vaqtinchalik psixotik buzilish
- xayolparastlik buzilishi (doimiy xayolparastlik buzilishi)
- surunkali gallyutsinatsion psixoz
Psixotik alomatlar quyidagilarda ham kuzatilishi mumkin:[24]
- shizotipal shaxsiyat buzilishi
- aniq shaxsiyatning buzilishi stress paytida (shu jumladan paranoid shaxsiyat buzilishi, shizoid shaxsiyat buzilishi va chegara kishilik buzilishi )
- katta depressiv buzilish uning og'ir shaklida, garchi psixozisiz og'ir depressiya bo'lishi mumkin va ehtimol
- bipolyar buzilish ichida manik va aralash epizodlar ning bipolyar I buzilishi va ikkalasining ham depressiv epizodlari bipolyar I va bipolyar II; ammo, psixotik alomatlarsiz bunday holatlarni boshdan kechirish mumkin.
- travmatik stress buzilishi
- sabab bo'lgan delusional buzilish
- Ba'zan obsesif-kompulsiv buzilish
- Voyaga etmaganlarda boshlangan affektiv buzilish[6]
- Dissociativ kasalliklar Ko'plab alomatlar tufayli ehtiyotkorlik bilan differentsial diagnostika, ayniqsa, o'z ichiga oladi dissotsiativ identifikatsiyani buzilishi.[35]
Stress psixotik holatlarga hissa qo'shishi va qo'zg'atishi ma'lum. Psixologik travmatik voqealar tarixi va so'nggi paytlarda stressli hodisalar tajribasi ikkalasi ham psixoz rivojlanishiga hissa qo'shishi mumkin. Qisqa muddatli stress tufayli yuzaga keladigan psixoz ma'lum qisqa reaktiv psixoz, va bemorlar o'z-o'zidan ikki hafta ichida normal ishlashini tiklashlari mumkin.[36] Ba'zi kamdan-kam holatlarda, odamlar ko'p yillar davomida to'la-to'kis psixoz holatida qolishlari yoki aksariyat hollarda mavjud bo'lgan psixotik alomatlarni (masalan, past intensiv gallyutsinatsiyalar) susaytirishi mumkin.
Nörotizm - bu psixoz rivojlanishining mustaqil bashoratchisi.[37]
Subtiplar
Psixozning pastki turlariga quyidagilar kiradi:
- Menstrüel psixoz, shu bilan ritmik ravishda taxminan menual (taxminan oylik) davriylikni o'z ichiga oladi hayz tsikli.
- Tug'ilgandan keyingi psixoz, birozdan keyin sodir bo'lgan tug'ish
- Monotematik xayollar
- Miksedematoz psixoz
- Stimulyator psixoz
- Kechikadigan psixoz
- Umumiy psixoz
Sikloid psixoz
Sikloid psixoz - bu odatdagidan to to'lqinli holatga o'tadigan, odatda bir necha soatdan bir necha kungacha, giyohvand moddalarni iste'mol qilish bilan bog'liq bo'lmagan psixoz. miya shikastlanishi.[38] Sikloid psixoz Evropa psixiatriya diagnostikasida uzoq tarixga ega. "Sikloid psixoz" atamasi birinchi marta Karl Kleyst tomonidan 1926 yilda ishlatilgan. Klinik ahamiyatliligiga qaramay, ushbu tashxis adabiyotda ham, nozologiyada ham e'tiborsiz qoldirilgan. Sikloid psixozi so'nggi 50 yil ichida xalqaro adabiyotga katta qiziqish uyg'otdi, ammo so'nggi 15 yil ichida ilmiy tadqiqotlar soni sezilarli darajada kamaydi, ehtimol qisman tashxis joriy diagnostika tasniflash tizimiga kiritilgan degan noto'g'ri tushunchalar bilan izohlanadi. Shuning uchun sikloid psixoz ishlatilgan diagnostik tasniflash tizimlarida qisman tavsiflanadi. Sikloid psixoz baribir manik-depressiv buzilishdan va shizofreniyadan ajralib turadigan o'ziga xos o'ziga xos kasallik bo'lib, sikloid psixoz ikkala bipolyar (kayfiyatning asosiy siljishi) va shizofrenik alomatlarni ham o'z ichiga olishi mumkinligiga qaramay. Kasallik o'tkir, odatda o'zini o'zi cheklaydigan, funktsional psixotik holat bo'lib, juda xilma-xil klinik ko'rinishga ega bo'lib, deyarli izchil ravishda ma'lum darajada chalkashlik yoki bezovta qiluvchi hayratlanish borligi bilan ajralib turadi, lekin avvalambor kasallikning ko'p qirrali va xilma-xil ifodalari. oladi. Kasallikning asosiy xususiyatlari shundan iboratki, boshlanishi o'tkir, simptomlarning ko'p qirrali rasmini o'z ichiga oladi va odatda normal holatga qaytadi va uzoq muddatli prognoz yaxshi bo'ladi. Bunga qo'chimcha, diagnostika mezonlari quyidagi belgilarning kamida to'rttasini o'z ichiga oladi:[38]
- Chalkashlik
- Muvofiq bo'lmagan aldanishlar
- Gallyutsinatsiyalar
- Pan-tashvish, muayyan holatlar yoki holatlarga bog'liq bo'lmagan qattiq tashvish
- Baxt yoki yuqori darajadagi ekstaz
- Akinetik yoki giperkinetik tipdagi harakatchanlikning buzilishi
- O'limdan tashvishlaning
- Kayfiyat ma'lum darajada o'zgaradi, ammo tashxis qo'yish uchun zarur bo'lganidan kamroq affektiv buzilish
Sikloid psixoz odatda 15-50 yoshdagi odamlarda uchraydi.[38]
Tibbiy sharoit
Juda ko'p miqdordagi tibbiy sharoitlar ba'zan chaqirilgan psixozni keltirib chiqarishi mumkin ikkilamchi psixoz.[24] Bunga misollar:
- buzilishlarni keltirib chiqaradi deliryum (toksik psixoz), unda ong buzilgan
- neyro rivojlanishning buzilishi va xromosoma anomaliyalari, shu jumladan velocardiofacial sindrom
- kabi neyrodejenerativ kasalliklar Altsgeymer kasalligi,[39] Lewy tanalari bilan demans,[40] va Parkinson kasalligi[41][42]
- kabi fokal nevrologik kasallik qon tomir, miya shishi,[43] skleroz,[42] va ba'zi shakllari epilepsiya
- malignite (odatda miyadagi massalar orqali, paraneoplastik sindromlar )[42]
- yuqumli va postinfektsion sindromlar, shu jumladan infektsiyalarni keltirib chiqaradi deliryum, virusli ensefalit, OIV / OITS,[44] bezgak,[45] sifiliz[46]
- kabi endokrin kasallik hipotiroidizm, gipertireoz, Kushing sindromi, gipoparatireoz va giperparatireoz;[47] jinsiy gormonlar psixotik alomatlarga ham ta'sir qiladi va ba'zida tug'ilish psixozni keltirib chiqarishi mumkin tug'ruqdan keyingi psixoz[48]
- kabi metabolizmning tug'ma xatolari Süksin semialdegid dehidrogenaza etishmovchiligi, porfiriya va metakromatik leykodistrofiya[49][50][51][52]
- kabi oziqlanish etishmovchiligi B vitamini12 etishmovchilik[9]
- boshqa erishilgan metabolik kasalliklar, shu jumladan elektrolit kabi buzilishlar hipokalsemiya, gipernatremiya,[53] giponatremi,[54] gipokalemiya,[55] gipomagnezemiya,[56] gipermagnezemiya,[57] giperkalsemiya,[58] va gipofosfatemiya,[59] Biroq shu bilan birga gipoglikemiya,[60] gipoksiya va ishlamay qolishi jigar yoki buyraklar
- otoimmun va shunga o'xshash buzilishlar, masalan tizimli eritematoz (lupus, SLE), sarkoidoz, Xashimoto ensefalopatiyasi, anti-NMDA-retseptorlari ensefaliti va çölyak bo'lmagan kleykovina sezgirligi[49][61]
- zaharlanish, terapevtik dorilar (pastga qarang), rekreatsion dorilar (pastga qarang) va bir qator o'simliklar, zamburug'lar, metallar, organik birikmalar va bir nechta hayvon toksinlari[24]
- kabi uyqu buzilishi narkolepsiya (unda REM uyqu hushyorlikka kirsa)[24]
- kabi parazitar kasalliklar neyrosistitserkoz
Psixoaktiv dorilar
Turli xil psixoaktiv moddalar (qonuniy va noqonuniy) foydalanuvchilarning turli darajadagi dalillari bilan psixotik holatlarni yoki buzilishlarni keltirib chiqarishi, kuchaytirishi yoki kuchaytirishi bilan bog'liq. Bu mastlikdan keyin foydalanishdan keyin uzoqroq muddat yoki undan keyin sodir bo'lishi mumkin chekinish.[24] Psixozni keltirib chiqaradigan moddasi bo'lgan shaxslar o'zlarining psixozlari to'g'risida ko'proq ma'lumotga ega bo'lishadi va yuqori darajalarga ega bo'lishadi. o'z joniga qasd qilish fikri birlamchi psixotik kasallikka chalingan shaxslarga nisbatan.[62] Odatda psixotik simptomlarni keltirib chiqaradigan giyohvand moddalar kiradi spirtli ichimliklar, nasha, kokain, amfetaminlar, katinonlar, psixedel dorilar (kabi LSD va psilotsibin ), b-opioid retseptorlari agonistlar (kabi enadolin va salvinorin A ) va NMDA retseptorlari antagonistlari (kabi fentsiklidin va ketamin ).[24][63] Kofein shizofreniya bilan og'rigan odamlarda alomatlarni kuchaytirishi va kasalliksiz odamlarda juda yuqori dozalarda psixozni keltirib chiqarishi mumkin.[64][65] Nasha va boshqa noqonuniy rekreatsion giyohvand moddalar ko'pincha o'spirinlarda psixoz bilan bog'liq bo'lib, 15 yoshga to'lgunga qadar nasha ishlatilishi keyinchalik katta yoshdagi psixoz xavfini oshirishi mumkin.[6]
Spirtli ichimliklar
Chalingan odamlarning taxminan uch foizi alkogolizm o'tkir intoksikatsiya yoki tushkunlik paytida psixozni boshdan kechirish. Spirtli ichimliklar bilan bog'liq psixoz a orqali o'zini namoyon qilishi mumkin yoqish mexanizmi. Spirtli ichimliklar bilan bog'liq psixoz mexanizmi spirtli ichimliklarni iste'mol qilishning uzoq muddatli ta'siri natijada neyron membranalariga buzilishlar, gen ekspressioni, shu qatorda; shu bilan birga tiamin etishmovchilik. Ba'zi hollarda alkogolni yoqish mexanizmi orqali suiiste'mol qilish surunkali moddani keltirib chiqaradigan psixotik buzilish, ya'ni shizofreniya rivojlanishiga olib kelishi mumkin. Spirtli ichimliklar bilan bog'liq psixozning ta'siriga ruhiy tushkunlik va o'z joniga qasd qilish xavfi, shuningdek, psixologik buzilishlar kiradi.[66]
Nasha
Ba'zi tadkikotlarga ko'ra, nasha tez-tez ishlatilsa, odamda psixotik kasallik paydo bo'lishi ehtimoli ko'proq bo'ladi,[67] tez-tez ishlatib turish psixoz va shizofreniya xavfining ikki barobariga bog'liq.[68][69] Nasha foydalanish shizofreniya sababchisi sifatida qabul qilingan bo'lsa-da,[70] nasha foydalanish va psixoz o'rtasidagi bog'liqlikka ta'sir qiluvchi asosiy omil sifatida psixozga nisbatan zaiflik paydo bo'ldi.[71][72] Ba'zi tadqiqotlar shuni ko'rsatadiki, nasha tarkibidagi ikkita faol birikmaning ta'siri, tetrahidrokannabinol (THC) va kannabidiol (CBD), psixozga qarama-qarshi ta'sir ko'rsatadi. THC sog'lom odamlarda psixotik alomatlarni keltirib chiqarishi mumkin bo'lsa-da, CBD nasha sababli alomatlarni kamaytirishi mumkin.[73]
So'nggi bir necha o'n yillikda nasha iste'mol qilish darajasi keskin oshdi, psixoz darajasi esa oshmadi. Ushbu topilmalar birgalikda nasha foydalanish psixozga moyil bo'lganlarda psixoz paydo bo'lishini tezlashtirishi mumkin.[74] Kuchli nasha iste'mol qilish haqiqatan ham moyil bemorlarda psixoz paydo bo'lishini tezlashtiradiganga o'xshaydi.[75] 2012 yilgi tadqiqotlar shuni ko'rsatdiki, nasha zaif odamlarda psixoz rivojlanishida muhim rol o'ynaydi va o'spirinning erta davrida nasha foydalanishdan voz kechish kerak.[76]
Metamfetamin
Metamfetamin og'ir foydalanuvchilarning 26-46 foizida psixozni keltirib chiqaradi. Ushbu odamlarning ba'zilari olti oydan ko'proq davom etishi mumkin bo'lgan uzoq muddatli psixozni rivojlantiradilar. Metamfetamindan qisqa muddatli psixozni boshdan kechirganlar, metamfetaminga qaytmaganiga qaramay, og'ir uyqusizlik yoki og'ir spirtli ichimliklarni iste'mol qilish davri kabi stressli hodisalardan keyin bir necha yil o'tgach metamfetamin psixozining qaytalanishi mumkin.[77] Metamfetaminni uzoq vaqtdan beri suiiste'mol qilgan va ilgari metamfetaminni suiiste'mol qilgan psixozni boshdan kechirgan shaxslar, giyohvand moddalarni iste'mol qilish tavsiya etilsa, metamfetamin psixozini qayta boshdan kechirishlari mumkin. Metamfetamin bilan bog'liq psixoz, genetik zaiflik bilan kechishi mumkin, bu takroriy qo'llanilgandan so'ng miya neyrokimyosida uzoq muddatli o'zgarishlarni keltirib chiqarishi mumkin.[78]
Dori-darmon
Ko'p sonli dori-darmonlarni qabul qilish yoki ba'zan ulardan voz kechish psixotik simptomlarni keltirib chiqarishi mumkin.[24] Eksperimental ravishda yoki odamlarning katta qismida psixozni keltirib chiqaradigan dorilar kiradi amfetamin va boshqalar sempatomimetika, dopamin agonistlar, ketamin, kortikosteroidlar (ko'pincha qo'shimcha ravishda kayfiyat o'zgarishi bilan) va ba'zi bir antikonvulsanlar vigabatrin.[24][79] Bunga olib kelishi mumkin bo'lgan stimulyatorlar kiradi lisdexamfetamin.[80]
Meditatsiya psixologik yon ta'sirlarni keltirib chiqarishi mumkin, shu jumladan shaxssizlashtirish, derealizatsiya va shunga o'xshash psixotik alomatlar gallyutsinatsiyalar shuningdek, kayfiyatning buzilishi.[81]
Patofiziologiya
Neyroimaging
Psixoz bilan kasallangan odamning birinchi miyadagi tasviri 1935 yilga kelib ushbu uslub yordamida yakunlangan pnevmenseensefalografiya[82] (og'riqli va endi eskirgan protsedura qaerda miya omurilik suyuqligi miya atrofidan drenajlanadi va miyaning tuzilishi anda aniqroq ko'rinishini ta'minlash uchun havo bilan almashtiriladi Rentgen rasm).
Ikkalasi ham birinchi epizod psixoz va yuqori xavfli holat kulrang moddalar hajmining (GMV) pasayishi bilan bog'liq. Birinchi epizod psixotik va yuqori xavfli populyatsiyalar GMVda o'xshash, ammo aniq anormalliklarga bog'liq. O'ngdagi qisqartirish o'rta vaqtinchalik girus, to'g'ri yuqori vaqtinchalik girus (STG), to'g'ri parahippokampus, to'g'ri gipokampus, to'g'ri o'rta frontal girus va chap oldingi singulat korteksi (ACC) yuqori xavfli populyatsiyalarda kuzatiladi. Birinchi epizod psixozining qisqarishi o'ng STG dan o'ngga, chapga va serebellumgacha bo'lgan mintaqani qamrab oladi va o'ng ACC, o'ng STG, insula va serebellumda og'irroq bo'ladi.[83][84]
Boshqa bir meta-tahlil insula, operkulum, STG, medial frontal korteks va ACC ning ikki tomonlama pasayishi haqida xabar berdi, ammo GMV ning o'ng tomonida ko'payganligi haqida xabar berdi lisoniy girus va ketdi prekentral girus.[85] The Kraepelinian dixotomiyasi shubhali qilingan[tushuntirish kerak ] bipolyar va shizofreniyada kulrang moddalarning anormalliklari bilan; shizofreniya bipolyardan ajralib turadi, chunki kulrang moddalarning qisqarishi mintaqalari kattaligi jihatidan kattaroqdir, ammo jinsi farqlariga moslashish chapdagi farqni kamaytiradi dorsomedial prefrontal korteks va to'g'ri dorsolateral prefrontal korteks.[86]
Diqqatli topshiriqlar paytida birinchi epizod psixozi o'ng o'rta frontal girusda gipoaktivatsiya bilan bog'liq bo'lib, odatda mintaqani o'z ichiga olgan dorsolateral prefrontal korteks (dlPFC). Kulrang moddalar miqdori bo'yicha tadqiqotlar bilan mos ravishda, o'ng insula va o'ng pastki parietal lobda gipoaktivlik ham bildirilgan.[87] Kognitiv vazifalar paytida o'ng insula, dACC va chap prekreusdagi gipoaktivliklar, shuningdek o'ngdagi deaktivatsiyalar kamayadi bazal ganglionlar, to'g'ri talamus, to'g'ri pastki frontal va ketdi prekentral giriya kuzatilmoqda. Ushbu natijalar juda izchil va takrorlanishi mumkin, ehtimol o'ng pastki frontal girusning anormalliklari bundan mustasno.[88] Ikki tomonlama hipoaktivlik bilan birgalikda kulrang moddalar hajmining pasayishi oldingi insula, dorsal medial frontal korteks va dorsal ACCda kuzatiladi. Orqa insula, ventral medial frontal korteks va ventral ACCda kulrang moddalar miqdori kamayganligi va ikki tomonlama giperaktivlik qayd etilgan.[89]
Gallyutsinatsiyalar
Gallyutsinatsiyalarning o'tkir tajribalari davomida o'tkazilgan tadqiqotlar birlamchi yoki ikkilamchi sezgir kortekslarda faollik oshganligini namoyish etadi. Psixozda eshitish gallyutsinatsiyalari eng ko'p uchraganligi sababli, chap tomonda faollikni oshirish uchun eng ishonchli dalillar mavjud o'rta vaqtinchalik girus, chap yuqori vaqtinchalik girus va chap pastki frontal girus (ya'ni Brokaning maydoni ). Faoliyat ventral striatum, gipokampus, va ACC gallyutsinatsiyalarning ravshanligi bilan bog'liq bo'lib, hissiy elektronlarning faollashishi yoki ishtirok etishi sezgir korteksdagi g'ayritabiiy faoliyat ta'sirining kalitidir. Birgalikda, ushbu topilmalar ichki ishlab chiqarilgan hissiy tajribalarni g'ayritabiiy qayta ishlashini va g'ayritabiiy hissiy ishlov berish bilan birgalikda gallyutsinatsiyalarni keltirib chiqaradi. Taklif etilayotgan modellardan biri, sezgir kortekslardan pastki frontal korteksgacha bo'lgan uzatish tarmoqlarining ishlamay qolishini o'z ichiga oladi, bu odatda ichki ishlab chiqarilgan nutq paytida sezgir korteks faolligini bekor qiladi. Natijada kutilayotgan va idrok etilayotgan nutqning buzilishi aniq gallyutsinatsiya tajribalarini keltirib chiqaradi deb o'ylashadi.[90]
Xayollar
Ikki omilli aldanishlar modeli ikkala e'tiqodni shakllantirish tizimida ham, e'tiqodni baholash tizimida ham disfunktsiya xayolot uchun zarurdir. O'ng lateral prefrontal korteksga joylashtirilgan baholash tizimlarining buzilishi, delusion tarkibidan qat'i nazar, neyroimaging tadqiqotlari bilan qo'llab-quvvatlanadi va sog'lom odamlarda mojarolarni kuzatishda uning roliga mos keladi. G'ayritabiiy faollashuv va hajmning pasayishi xayollarga chalingan odamlarda, shuningdek, xayolot bilan bog'liq kasalliklarda kuzatiladi. frontotemporal demans, psixoz va Lewy tana demansi. Bundan tashqari, ushbu mintaqadagi shikastlanishlar "shoshilib xulosa qilish" bilan bog'liq bo'lib, ushbu mintaqaga zarar etkazish qon tomiridan keyingi delusiyalar bilan va bu mintaqada gipometabolizm bilan deluziya bilan kechadigan kaudat qon tomirlari bilan bog'liq.
The aberrant salience modeli aldanishlar odamlarning ahamiyatsiz stimullarga haddan tashqari muhim ahamiyat berishlari natijasidir. Ushbu gipotezani qo'llab-quvvatlash uchun odatda mintaqalar muhim tarmoq aldangan odamlarda va neyrotransmitterda pasaygan kulrang moddalarni namoyish etish dopamin shoshilinch ishlov berishda keng ishtirok etadigan, shuningdek, psixotik kasalliklarda keng tarqalgan.
Muayyan mintaqalar aldanishlarning o'ziga xos turlari bilan bog'liq edi. Gipokampus va parahippokampus hajmi paranoidal xayollarga bog'liq Altsgeymer kasalligi, va bir odamda o'limdan keyin g'ayritabiiy bo'lganligi haqida xabar berilgan. Capgras delusions oksipito-temporal shikastlanish bilan bog'liq bo'lib, yuzlarga javoban oddiy his-tuyg'ularni yoki xotiralarni keltirib chiqarmaslik bilan bog'liq bo'lishi mumkin.[91]
Salbiy alomatlar
Ushbu bo'lim aksariyat o'quvchilar tushunishi uchun juda texnik bo'lishi mumkin. Iltimos uni yaxshilashga yordam bering ga buni mutaxassis bo'lmaganlarga tushunarli qilish, texnik ma'lumotlarni olib tashlamasdan. (Noyabr 2019) (Ushbu shablon xabarini qanday va qachon olib tashlashni bilib oling) |
Psixoz bilan bog'liq ventral striatal mukofotni kutish va fikr-mulohazalar paytida gipoaktivlik. Chap ventral striatumdagi gipoaktivlik zo'ravonlik bilan bog'liq salbiy alomatlar.[92] Anhedoniya psixozda tez-tez uchraydigan alomat bo'lsa-da, hedonik tajribalar shizofreniya bilan kasallangan odamlarning ko'pchiligida aslida buzilmagan. O'zini anhedoniya deb ko'rsatishi mumkin bo'lgan buzilish, ehtimol, maqsadlarni aniqlay olmaslik, maqsadlarga erishish uchun zarur bo'lgan xatti-harakatlarni aniqlay olmaslikdir.[93] Tadqiqotlar maqsadlar va maqsadga yo'naltirilgan xatti-harakatlarning asabiy ifodalanishidagi etishmovchilikni mukofotni olish (kutish emas) ventral striatumda kuchli javob bilan bog'liqligini namoyish etish orqali qo'llab-quvvatlaydi; rag'batlantirish mukofotiga oid favqulodda vaziyatlar mavjud bo'lganda, ammo aniq asabiy ishlov berishni talab qilganda kuchaytirishni o'rganish buzilmaydi; mukofotni bashorat qilish xatolari (funktsional neyroimaging tadqiqotlari paytida), ayniqsa ijobiy PElar g'ayritabiiydir. Ijobiy bashorat qilishda xatolik, miya mintaqasida faollashuv kuchayganda, odatda striatum, kutilmagan mukofotlarga javoban. Bashorat qilishning salbiy javobi, bashorat qilingan mukofotlar sodir bo'lmaganda mintaqada aktivizatsiya pasayganda yuz beradi.[93] ACC javobi, kuch sarflash ko'rsatkichi sifatida qabul qilingan, mukofot yoki mukofot ehtimolligi oshishi bilan ko'paymaydi va salbiy alomatlar bilan bog'liq; dlPFC faoliyatidagi kamchiliklar va pul imtiyozlari mavjud bo'lganda, kognitiv vazifalar bo'yicha ishlarning yaxshilanmaganligi; va dofamin vositachiligi funktsiyalari g'ayritabiiydir.[93]
Neyrobiologiya
Ushbu bo'lim aksariyat o'quvchilar tushunishi uchun juda texnik bo'lishi mumkin. Iltimos uni yaxshilashga yordam bering ga buni mutaxassis bo'lmaganlarga tushunarli qilish, texnik ma'lumotlarni olib tashlamasdan. (Noyabr 2019) (Ushbu shablon xabarini qanday va qachon olib tashlashni bilib oling) |
Psixoz an'anaviy ravishda haddan tashqari faollik bilan bog'liq neyrotransmitter dopamin. Xususan, uning ta'siriga mezolimbik yo'l. Ushbu nazariyani qo'llab-quvvatlash uchun berilgan ikkita asosiy dalil manbai shu dopamin retseptorlari D2 dorilarni blokirovka qilish (ya'ni, antipsikotiklar ) psixotik alomatlar intensivligini pasaytiradi va dofamin ajralishini kuchaytiradigan yoki uni qaytarib olishga to'sqinlik qiladigan dorilar (masalan amfetaminlar va kokain ) ba'zi odamlarda psixozni keltirib chiqarishi mumkin (qarang) stimulyator psixoz ).[94]
NMDA retseptorlari disfunktsiyasi psixozda mexanizm sifatida taklif qilingan.[95] Ushbu nazariya haqiqat bilan mustahkamlangan dissotsiativ NMDA retseptorlari antagonistlari kabi ketamin, PCP va dekstrometorfan (katta dozani oshirib yuborishda) psixotik holatni keltirib chiqaradi. Dissotsiatsiya belgilari mastlik shizofreniya alomatlarini aks ettirish, shu jumladan salbiy alomatlar.[96] NMDA retseptorlari antagonizmi, psixozni eslatuvchi alomatlarni hosil qilishdan tashqari, neyrofiziologik jihatlarni, masalan, amplituda pasayishni taqlid qiladi. P50, P300 va MMN uyg'ongan potentsial.[97] Neyroimaging adabiyotlari bilan kelishilgan holda, sensorli geribildirimning ierarxik Bayesiya neyrokompyuter modellari NMDA retseptorlari gipofontsiyasini delusional yoki gallyutsinatsion simptomlarga bog'lab, NMDA vositachiligining yuqoridan pastga prognozlarini muvaffaqiyatsizlikni taklif qilish orqali kuchaytirilgan pastdan yuqoriga AMPA vositachiligidagi prognozlar xatolarini bekor qilish.[98] Odatda bunday reaktsiyani keltirib chiqarmaydigan stimullarga javoban haddan tashqari bashorat qilish xatolari, aks holda dunyoviy voqealarga haddan tashqari shov-shuv berishdan kelib chiqadi deb o'ylashadi.[99] Vakillik mavhumroq bo'lgan ierarxiyadagi yuqori darajadagi disfunktsiya xayollarga olib kelishi mumkin.[100] Umumiy topilma qisqartirildi GAD67 psixotik kasalliklarda ifoda etish GABAergik inhibisyonunun kamayishi natijasida kelib chiqqan AMPA vositachiligining kuchayganligini tushuntirishi mumkin.[101][102]
Dopamin va psixoz o'rtasidagi bog'liqlik odatda murakkab deb hisoblanadi. Dopamin retseptorlari D2 bostirilganda adenilat siklaza faoliyat, D1 retseptorlari uni ko'paytiradi. Agar D2-blokirovka qiluvchi dorilar qo'llanilsa, bloklangan dofamin D1 retseptorlariga to'kiladi. Adenilat siklaza faolligining oshishiga ta'sir qiladi genetik ifoda vaqt talab qiladigan asab hujayrasida. Shuning uchun antipsikotik dorilar psixoz alomatlarini kamaytirish uchun bir-ikki hafta vaqt oladi. Bundan tashqari, yangi va bir xil darajada samarali antipsikotik dorilar miyada dopaminni eski dori-darmonlarga qaraganda biroz kamroq to'sadi, 5-HT2A retseptorlarini esa blokirovka qiladi, bu esa "dopamin gipotezasi" ni soddalashtirilgan bo'lishi mumkin.[103] Soyka va uning hamkasblari spirtli psixoz bilan og'rigan odamlarda dopaminerjik disfunktsiyaning mavjudligini aniqlamadilar[104] va Zoldan va boshq. ning o'rtacha darajada muvaffaqiyatli ishlatilishini xabar qildi ondansetron, 5-HT3 retseptorlari antagonisti, davolashda levodopa psixoz Parkinson kasalligi bemorlar.[105]
Ko'rib chiqish psixoz va prediyabetning birinchi epizodi bilan bog'liqligini aniqladi.[106]
Psixodan uzoq yoki yuqori dozada foydalanishstimulyatorlar normal ishlashini o'zgartirishi mumkin, bipolyar buzilishning manik fazasiga o'xshashdir.[107] NMDA antagonistlari o'xshash "salbiy" alomatlarni takrorlaydi fikr buzilishi subanestetik dozalarda (induktsiya qilish uchun etarli bo'lmagan dozalar behushlik ) va katatoniya yuqori dozalarda). Psixostimulyatorlar, ayniqsa psixotik tafakkurga moyil bo'lgan odamlarda, ba'zi "ijobiy" alomatlarni keltirib chiqarishi mumkin, masalan, aldangan e'tiqodlar, xususan tabiatdagi ta'qiblar.
Tashxis
Psixoz bilan og'rigan odamda ruhiy kasallik tashxisini qo'yish boshqa mumkin bo'lgan sabablarni chiqarib tashlash kerak.[108] Dastlabki baholash tibbiy xizmat ko'rsatuvchi shaxsning keng qamrovli tarixi va fizik tekshiruvini o'z ichiga oladi. Sinovlar moddani iste'mol qilishni, dori-darmonlarni, toksinlarni, jarrohlik asoratlarni yoki boshqa tibbiy kasalliklarni istisno qilish uchun o'tkazilishi mumkin. Psikozli odam psixotik deb ataladi.
Deliryum vizual gallyutsinatsiyalar, o'tkir boshlanish va ongning o'zgaruvchan darajasi bilan ajralib turadigan, boshqa asosiy omillarni, shu jumladan tibbiy kasalliklarni ko'rsatadigan holda chiqarib tashlanishi kerak.[109] Psixoz bilan bog'liq tibbiy kasalliklarni hisobga olmaganda, qonni tekshirish yordamida quyidagi usullarni o'lchash mumkin:
- Qalqonsimon bezni stimulyatsiya qiluvchi gormon chiqarib tashlamoq gipo- yoki gipertireoz,
- Asosiy elektrolitlar va sarum kaltsiy metabolizm buzilishini istisno qilish,
- To'liq qon tekshiruvi shu jumladan ESR tizimli infektsiyani yoki surunkali kasallikni istisno qilish va
- Serologiya chiqarib tashlamoq sifiliz yoki OIV infektsiya.
Boshqa tekshiruvlarga quyidagilar kiradi:
- EEG chiqarib tashlamoq epilepsiya va
- MRI yoki KTni tekshirish miya lezyonlarini istisno qilish uchun boshning.
Psixoz tez-tez uchrab turishi yoki kuchayishi mumkin bo'lgan dorilarning umumiy sinflari tufayli, dori vositasida psixoz bo'lishi kerak chiqarib tashlandi, ayniqsa birinchi epizodli psixoz uchun. Ham modda, ham dorilar ta'sirida psixoz bo'lishi mumkin chiqarib tashlandi toksikologik skrining yordamida yuqori aniqlik darajasida.
Chunki ba'zi xun takviyeleri shuningdek, psixoz yoki maniyani keltirib chiqarishi mumkin, ammo laboratoriya tekshiruvlari bilan istisno etilishi mumkin emas, psixotik shaxsning oilasi, sherigi yoki do'stlaridan bemor hozirda biron bir parhez qo'shimchasini qabul qiladimi, deb so'rash kerak.[110]
Common mistakes made when diagnosing people who are psychotic include:[108]
- Not properly excluding delirium,
- Not appreciating medical abnormalities (e.g., vital signs),
- Not obtaining a medical history and family history,
- Indiscriminate screening without an organizing framework,
- Missing a toxic psychosis by not screening for substances va dorilar,
- Not asking their family or others about dietary supplements,
- Premature diagnostic closure, and
- Not revisiting or questioning the initial diagnostic impression of primary psychiatric disorder.
Only after relevant and known causes of psychosis are excluded, a mental health clinician may make a psychiatric differentsial diagnostika using a person's family history, incorporating information from the person with psychosis, and information from family, friends, or significant others.
Types of psychosis in psychiatric disorders may be established by formal rating scales. The Qisqa psixiatrik reyting shkalasi (BPRS)[111] assesses the level of 18 symptom constructs of psychosis such as dushmanlik, shubha, gallyutsinatsiya va ulug'vorlik. It is based on the clinician's interview with the patient and observations of the patient's behavior over the previous 2–3 days. The patient's family can also answer questions on the behavior report. During the initial assessment and the follow-up, both positive and negative symptoms of psychosis can be assessed using the 30 item Positive and Negative Symptom Scale (PANSS).[112]
The DSM-5 characterizes disorders as psychotic or on the schizophrenia spectrum if they involve hallucinations, delusions, disorganized thinking, grossly disorganized motor behavior, or negative symptoms.[16] The DSM-5 does not include psychosis as a definition in the glossary, although it defines "psychotic features", as well as "psychoticism" with respect to personality disorder. The ICD-10 has no specific definition of psychosis.[113]
Faktor tahlili of symptoms generally regarded as psychosis frequently yields a five factor solution, albeit five factors that are distinct from the five domains defined by the DSM-5 to encompass psixotik or schizophrenia spectrum disorders. The five factors are frequently labeled as hallucinations, delusions, disorganization, excitement, and emotional distress.[113] The DSM-5 emphasizes a psixotik spektr, wherein the low end is characterized by schizoid personality disorder, and the high end is characterized by schizophrenia.[42]
Oldini olish
The evidence for the effectiveness of early interventions to oldini olish psychosis appeared inconclusive.[114] But psychosis caused by drugs can be prevented.[115] Whilst early intervention in those with a psychotic episode might improve short-term outcomes, little benefit was seen from these measures after five years.[116] However, there is evidence that kognitiv xulq-atvor terapiyasi (CBT) may reduce the risk of becoming psychotic in those at high risk,[117] and in 2014 the UK Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti (NICE) recommended preventive CBT for people at risk of psychosis.[118][119]
Davolash
The treatment of psychosis depends on the specific diagnosis (such as schizophrenia, bipolar disorder or substance intoxication). The first-line treatment for many psychotic disorders is antipsychotic medication,[120] which can reduce the positive symptoms of psychosis in about 7 to 14 days. For youth or adolescents, treatment options include medications, psychological interventions, and social interventions.[6]
Dori-darmon
The choice of which antipsikotik to use is based on benefits, risks, and costs.[116] It is debatable whether, as a class, tipik yoki atipik antipsikotiklar are better.[121][122] Tentative evidence supports that amisulprid, olanzapin, risperidon va klozapin may be more effective for positive symptoms but result in more side effects.[123] Odatda antipsikotiklar past va o'rtacha dozalarda qo'llanganda atipiklarga tushish va simptomlarning qaytalanish darajasi teng.[124] There is a good response in 40–50%, a partial response in 30–40%, and treatment resistance (failure of symptoms to respond satisfactorily after six weeks to two or three different antipsychotics) in 20% of people.[125] Klozapin - boshqa dorilarga ("davolanishga chidamli" yoki "refrakter" shizofreniya) yomon ta'sir ko'rsatadiganlar uchun samarali davo,[126] ammo bu mumkin bo'lgan jiddiy yon ta'sirga ega agranulotsitoz (tushirildi oq qon hujayrasi odamlarning 4 foizidan kamrog'ida).[116][127][128]
Most people on antipsychotics get side effects. People on typical antipsychotics tend to have a higher rate of ekstrapiramidal yon ta'siri while some atypicals are associated with considerable weight gain, diabetes and risk of metabolik sindrom; this is most pronounced with olanzapine, while risperidone and ketiapin are also associated with weight gain.[123] Risperidone has a similar rate of extrapyramidal symptoms to haloperidol.[123]
Maslahat
Psychological treatments such as qabul qilish va majburiyat terapiyasi (ACT) are possibly useful in the treatment of psychosis, helping people to focus more on what they can do in terms of valued life directions despite challenging symptomology.[129]
There are psychological interventions that seek to treat the symptoms of psychosis. In a 2019 review, nine classes of psychosocial interventions were identified: need adapted treatment, open dialogue, psychoanalysis/psychodynamic psychotherapy, major role therapy, soteria, psychosocial outpatient and inpatient treatment, o'rta terapiya va KBT. This paper concluded that when on minimal or no medication "the overall evidence supporting the effectiveness of these interventions is generally weak".[130]
Erta aralashuv
Early intervention in psychosis is based on the observation that identifying and treating someone in the early stages of a psychosis can improve their longer term outcome.[131] This approach advocates the use of an intensive multi-disciplinary approach during what is known as the muhim davr, where intervention is the most effective, and prevents the long-term morbidity associated with chronic psychotic illness.
Tarix
Etimologiya
So'z psixoz was introduced to the psychiatric literature in 1841 by Karl Friedrich Canstatt uning ishida Handbuch der Medizinischen Klinik. He used it as a shorthand for 'psychic neurosis'. At that time neurosis meant any disease of the asab tizimi, and Canstatt was thus referring to what was considered a psychological manifestation of brain disease.[132] Ernst fon Feuchtersleben is also widely credited as introducing the term in 1845,[133] ga alternativa sifatida aqldan ozish va mani.
Bu atama kelib chiqadi Zamonaviy lotin psixoz, "a giving soul or life to, animating, quickening" and that from Qadimgi yunoncha ψυχή (ruhiyat), "soul" and the suffix -ωσις (-osis), in this case "abnormal condition".[134][135]
In its adjective form "psychotic", references to psychosis can be found in both clinical and non-clinical discussions. However, in a non-clinical context, "psychotic" is generally used as a synonym for "insane".
Tasnifi
The word was also used to distinguish a condition considered a disorder of the mind, as opposed to nevroz, which was considered a disorder of the nervous system.[136] The psychoses thus became the modern equivalent of the old notion of jinnilik, and hence there was much debate on whether there was only one (unitar) or many forms of the new disease.[137] One type of broad usage would later be narrowed down by Koch in 1891 to the 'psychopathic inferiorities'—later renamed abnormal personalities by Shnayder.[132]
The division of the major psychoses into manic depressive illness (now called bipolyar buzilish ) and dementia praecox (now called shizofreniya ) tomonidan qilingan Emil Kraepelin, who attempted to create a synthesis of the various mental disorders identified by 19th-century psixiatrlar, by grouping diseases together based on classification of common symptoms. Kraepelin used the term 'manic depressive insanity' to describe the whole spectrum of kayfiyatning buzilishi, in a far wider sense than it is usually used today.
In Kraepelin's classification this would include 'unipolar' klinik depressiya, as well as bipolar disorder and other mood disorders such as siklotimiya. These are characterised by problems with mood control and the psychotic episodes appear associated with disturbances in mood, and patients often have periods of normal functioning between psychotic episodes even without medication. Shizofreniya is characterized by psychotic episodes that appear unrelated to disturbances in mood, and most non-medicated patients show signs of disturbance between psychotic episodes.
Davolash
Early civilizations considered madness a supernaturally inflicted phenomenon. Archaeologists have unearthed skulls with clearly visible drillings, some datable back to 5000 BC suggesting that trepanning was a common treatment for psychosis in ancient times.[138] Written record of supernatural causes and resultant treatments can be traced back to the Yangi Ahd. Mark 5:8–13 describes a man displaying what would today be described as psychotic symptoms. Masih cured this "iblis madness" by casting out the demons and hurling them into a herd of swine. Exorcism is still utilized in some religious circles as a treatment for psychosis presumed to be demonic possession.[139] A research study of out-patients in psychiatric clinics found that 30 percent of religious patients attributed the cause of their psychotic symptoms to evil spirits. Many of these patients underwent exorcistic healing rituals that, though largely regarded as positive experiences by the patients, had no effect on symptomology. Results did, however, show a significant worsening of psychotic symptoms associated with exclusion of medical treatment for coercive forms of exorcism.[140]
The medical teachings of the fourth-century philosopher and physician Hippocrates of Cos proposed a natural, rather than supernatural, cause of human illness. In Hippocrates' work, the Gippokrat korpus, a holistic explanation for health and disease was developed to include madness and other "diseases of the mind." Hippocrates writes:
Men ought to know that from the brain, and from the brain only, arise our pleasures, joys, laughter, and jests, as well as our sorrows, pains, griefs and tears. Through it, in particular, we think, see, hear, and distinguish the ugly from the beautiful, the bad from the good, the pleasant from the unpleasant…. It is the same thing which makes us mad or delirious, inspires us with dread and fear, whether by night or by day, brings sleeplessness, inopportune mistakes, aimless anxieties, absentmindedness, and acts that are contrary to habit.[141]
Hippocrates espoused a theory of humoralizm wherein disease is resultant of a shifting balance in bodily fluids including qon, phlegm, qora safro va sariq safro.[142] According to humoralism, each fluid or "hazil " has temperamental or behavioral correlates. In the case of psychosis, symptoms are thought to be caused by an excess of both blood and yellow bile. Thus, the proposed surgical intervention for psychotic or manic behavior was qon ketish.[143]
18th-century physician, educator, and widely considered "founder of American psychiatry", Benjamin Rush, also prescribed bloodletting as a first-line treatment for psychosis. Although not a proponent of humoralism, Rush believed that active purging and bloodletting were efficacious corrections for disruptions in the circulatory system, a complication he believed was the primary cause of "insanity".[144] Although Rush's treatment modalities are now considered antiquated and brutish, his contributions to psychiatry, namely the biological underpinnings of psychiatric phenomenon including psychosis, have been invaluable to the field. In honor of such contributions, Benjamin Rush's image is in the official seal of the Amerika psixiatriya assotsiatsiyasi.
Early 20th-century treatments for severe and persisting psychosis were characterized by an emphasis on shocking the nervous system. Such therapies include insulin shok terapiyasi, kardiyazol shock therapy, and elektrokonvulsiv terapiya.[145] Despite considerable risk, shock therapy was considered highly efficacious in the treatment of psychosis including shizofreniya. The acceptance of high-risk treatments led to more invasive medical interventions including psixosurgiya.[146]
In 1888, Swiss psychiatrist Gottlieb Burckhardt performed the first medically sanctioned psychosurgery in which the miya yarim korteksi was excised. Although some patients showed improvement of symptoms and became more subdued, one patient died and several developed afazi or seizure disorders. Burckhardt would go on to publish his clinical outcomes in a scholarly paper. This procedure was met with criticism from the medical community and his academic and surgical endeavors were largely ignored.[147] 30-yillarning oxirida, Egas Moniz homilador bo'lgan leykotomiya (AKA prefrontal lobotomy ) in which the fibers connecting the frontal lobes to the rest of the brain were severed. Moniz's primary inspiration stemmed from a demonstration by neuroscientists John Fulton and Carlyle's 1935 experiment in which two chimpanzees were given leucotomies and pre- and post-surgical behavior was compared. Prior to the leucotomy, the chimps engaged in typical behavior including throwing feces and fighting. After the procedure, both chimps were pacified and less violent. During the Q&A, Moniz asked if such a procedure could be extended to human subjects, a question that Fulton admitted was quite startling.[148] Moniz would go on to extend the controversial practice to humans suffering from various psychotic disorders, an endeavor for which he received a Nobel mukofoti 1949 yilda.[149] Between the late 1930s and early 1970s, the leucotomy was a widely accepted practice, often performed in non-steril environments such as small ambulatoriya clinics and patient homes.[148] Psychosurgery remained standard practice until the discovery of antipsychotic pharmacology in the 1950s.[150]
The first clinical trial of antipsikotiklar (also commonly known as neuroleptics) for the treatment of psychosis took place in 1952. Xlorpromazin (brand name: Thorazine) passed clinical trials and became the first antipsychotic medication approved for the treatment of both acute and chronic psychosis. Although the mechanism of action was not discovered until 1963, the administration of chlorpromazine marked the advent of the dopamine antagonist, or first generation antipsychotic.[151] While clinical trials showed a high response rate for both acute psychosis and disorders with psychotic features, the yon effektlar were particularly harsh, which included high rates of often irreversible Parkinsonian symptoms such as kech diskineziya. Kelishi bilan atipik antipsikotiklar (also known as second generation antipsychotics) came a dopamine antagonist with a comparable response rate but a far different, though still extensive, side-effect profile that included a lower risk of Parkinsonian symptoms but a higher risk of cardiovascular disease.[152] Atypical antipsychotics remain the first-line treatment for psychosis associated with various psychiatric and asab kasalliklari including schizophrenia, bipolyar buzilish, katta depressiv buzilish, tashvishlanish buzilishi, dementia va ba'zilari autizm spektri buzilishlar.[153]
Dopamine is now one of the primary neurotransmitters implicated in psychotic symptomology. Blocking dopamine receptors (namely, the dopamine D2 receptors) and decreasing dopaminergic activity continues to be an effective but highly unrefined effect of antipsychotics, which are commonly used to treat psychosis. Recent pharmacological research suggests that the decrease in dopaminergic activity does not eradicate psychotic xayollar yoki gallyutsinatsiyalar, but rather attenuates the reward mechanisms involved in the development of delusional thinking; that is, connecting or finding meaningful relationships between unrelated stimuli or ideas.[94] The author of this research paper acknowledges the importance of future investigation:
The model presented here is based on incomplete knowledge related to dopamine, schizophrenia, and antipsychotics—and as such will need to evolve as more is known about these.
— Shitij Kapur, From dopamine to salience to psychosis—linking biology, pharmacology and phenomenology of psychosis
Freud's former student Wilhelm Reich explored independent insights into the physical effects of neurotic and traumatic upbringing, and published his holistic psychoanalytic treatment with a schizophrenic. With his incorporation of breathwork and insight with the patient, a young woman, she achieved sufficient self-management skills to end the therapy.[154]
Lakan extended Freud's ideas to create a psychoanalytic model of psychosis based upon the concept of " musodara qilish ", the rejection of the symbolic concept of the father.
Jamiyat
Psixiatr Devid Xili has criticised pharmaceutical companies for promoting simplified biological theories of mental illness that seem to imply the primacy of pharmaceutical treatments while ignoring social and developmental factors that are known important influences in the etiology of psychosis.[155]
Tadqiqot
Further research in the form of randomized controlled trials is needed to determine the effectiveness of treatment approaches for helping adolescents with psychosis.[6]
Shuningdek qarang
Adabiyotlar
- ^ Kelly, Evelyn B. (2001). Coping with schizophrenia (1-nashr). Nyu-York: Rosen Pub. p. 25. ISBN 978-0-8239-2853-8.
- ^ Maio DV, Franscell R (2016). Morgue: A Life in Death. Sent-Martin matbuoti. p. 236. ISBN 978-1-4668-7506-7.
- ^ Bogousslavsky J, Boller F (2005). Neurological Disorders in Famous Artists. Karger tibbiyot va ilmiy nashrlari. p. 125. ISBN 978-3-8055-7914-8.
- ^ a b v d e f g h men j k l "RAISE Questions and Answers". NIMH. Olingan 23 yanvar 2018.
- ^ a b v d e "Psixoz". NHS. 2016 yil 23-dekabr. Olingan 24 yanvar 2018.
- ^ a b v d e f g h men Datta, Soumitra S; Daruvala, Rhea; Kumar, Ajit (2020-07-03). Cochrane Shizophrenia Group (tahrir). "Psychological interventions for psychosis in adolescents". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 7: CD009533. doi:10.1002/14651858.CD009533.pub2. PMC 7388907. PMID 32633858.
- ^ "Psychosis Symptoms". NHS. Olingan 24 yanvar 2018.
- ^ "Psychosis Causes". NHS. Olingan 24 yanvar 2018.
- ^ a b Griswold KS, Del Regno PA, Berger RC (June 2015). "Recognition and Differential Diagnosis of Psychosis in Primary Care". Amerika oilaviy shifokori. 91 (12): 856–63. PMID 26131945.
- ^ Cardinal RN, Bullmore ET (2011). The Diagnosis of Psychosis. Kembrij universiteti matbuoti. p. 279. ISBN 978-1-139-49790-9.
- ^ Foster, Norman L. (2011). The American Psychiatric Publishing Textbook of Geriatric Neuropsychiatry. Amerika Psixiatriya Pub. p. 523. ISBN 978-1-58562-952-7.
- ^ Leucht S, Arbter D, Engel RR, Kissling V, Devis JM (aprel 2009). "Ikkinchi avlod antipsikotik preparatlari qanchalik samaralidir? Platsebo nazorati ostida o'tkazilgan sinovlarning meta-tahlili". Molekulyar psixiatriya. 14 (4): 429–47. doi:10.1038 / sj.mp.4002136. PMID 18180760.
- ^ Rattehalli RD, Jayaram MB, Smith M (May 2010). "Risperidone versus placebo for schizophrenia". Shizofreniya byulleteni. 36 (3): 448–9. doi:10.1093/schbul/sbq030. PMC 2879694. PMID 20368309.
- ^ Gibbs, Ronald S. (2008). Danforth's Obstetrics and Gynecology. Lippincott Uilyams va Uilkins. p. 508. ISBN 978-0-7817-6937-2.
- ^ Giddens, Jean Foret (2015). Concepts for Nursing Practice - E-Book. Elsevier sog'liqni saqlash fanlari. p. 348. ISBN 978-0-323-38946-4.
- ^ a b v Assotsiatsiya, Amerika psixiatriyasi (2013). Diagnostic and statistical manual of mental disorders : DSM-5 (5-nashr). Vashington, DC: Amerika Psixiatriya Assotsiatsiyasi. p.125. ISBN 978-0-89042-554-1.
- ^ Toh, WL; Thomas, N; Rossell, SL (15 September 2015). "Auditory verbal hallucinations in bipolar disorder (BD) and major depressive disorder (MDD): A systematic review". Affektiv buzilishlar jurnali. 184: 18–28. doi:10.1016/j.jad.2015.05.040. PMID 26066781.
- ^ a b v d e f Lewis S, Escalona R, Keith S. "Phenomenology of Schizophrenia". In Sadock V, Sadock B, Ruiz P (eds.). Kaplan and Sadock's Comprehensive Textbook of Psychiatry. Wolters Kluwer.
- ^ Sato, Y .; Berrios, G. E. (26 April 2003). "Extracampine hallucinations". Lanset. 361 (9367): 1479–1480. doi:10.1016/S0140-6736(03)13128-5. PMID 12727431. S2CID 205939829. Olingan 8 iyun 2020.
- ^ Cannon, Brooke J.; Kramer, Lorraine Masinos (2011-03-18). "Delusion content across the 20th century in an American psychiatric hospital". Xalqaro ijtimoiy psixiatriya jurnali. SAGE nashrlari. 58 (3): 323–327. doi:10.1177/0020764010396413. ISSN 0020-7640. PMID 21421637. S2CID 42421925.
- ^ Seikkula, Birgitta Alakare, Jukka A, Jaakko (2001). "Open Dialogue in Psychosis I: An Introduction and Case Illustration". Journal of Constructivist Psychology. Informa UK Limited. 14 (4): 247–265. doi:10.1080/10720530125965. ISSN 1072-0537.CS1 maint: bir nechta ism: mualliflar ro'yxati (havola)
- ^ Jaspers K (1997-11-27) [1963]. Allgemeine Psychopathologie (General Psychopathology). Translated by J. Hoenig and M.W. Hamilton from German (Reprint ed.). Baltimor, Merilend: Jons Xopkins universiteti matbuoti. ISBN 978-0-8018-5775-1.
- ^ "What is Psychosis? Symptoms of Psychosis". earlypsychosis.ca. 2018. Arxivlangan asl nusxasi 2018-10-11 kunlari. Olingan 2018-10-11.
- ^ a b v d e f g h men j k Cardinal RN, Bullmore, ET (2011). The Diagnosis of Psychosis. Kembrij universiteti matbuoti. ISBN 978-0-521-16484-9.
- ^ Ohayon MM, Priest RG, Caulet M, Guilleminault C (October 1996). "Hypnagogic and hypnopompic hallucinations: pathological phenomena?". Britaniya psixiatriya jurnali. 169 (4): 459–67. doi:10.1192/bjp.169.4.459. PMID 8894197.
- ^ Sharma V, Mazmanian D (April 2003). "Sleep loss and postpartum psychosis". Bipolyar buzilishlar. 5 (2): 98–105. doi:10.1034/j.1399-5618.2003.00015.x. PMID 12680898.
- ^ Chan-Ob T, Boonyanaruthee V (September 1999). "Meditation in association with psychosis". Tailand tibbiyot birlashmasi jurnali = Chotmaihet Thangphaet. 82 (9): 925–30. PMID 10561951.
- ^ Devillieres P, Opitz M, Clervoy P, Stephany J (May–June 1996). "Delusion and sleep deprivation". L'Encefale. 22 (3): 229–31. PMID 8767052.
- ^ Gispen-de Wied, Christine C (2000-09-29). "Stress in schizophrenia: an integrative view". Evropa farmakologiya jurnali. Festschrift David de Wied. 405 (1): 375–384. doi:10.1016/S0014-2999(00)00567-7. ISSN 0014-2999. PMID 11033342.
- ^ a b v Gibson LE, Alloy LB, Ellman LM (November 2016). "Trauma and the psychosis spectrum: A review of symptom specificity and explanatory mechanisms". Klinik psixologiyani o'rganish. 49: 92–105. doi:10.1016/j.cpr.2016.08.003. PMC 5157832. PMID 27632064.
- ^ a b v Misiak B, Krefft M, Bielawski T, Moustafa AA, Sąsiadek MM, Frydecka D (April 2017). "Toward a unified theory of childhood trauma and psychosis: A comprehensive review of epidemiological, clinical, neuropsychological and biological findings". Neyrologiya va biobehavioral sharhlar. 75: 393–406. doi:10.1016/j.neubiorev.2017.02.015. PMID 28216171. S2CID 21614845.
- ^ J, van Os J, Morrison AP, Ross CA (2005 yil noyabr) ni o'qing. "Bolalik travması, psixoz va shizofreniya: nazariy va klinik oqibatlari bilan adabiyotni o'rganish". Acta Psychiatrica Scandinavica. 112 (5): 330–50. doi:10.1111 / j.1600-0447.2005.00634.x. PMID 16223421. S2CID 5324960.
- ^ Jahon Sog'liqni saqlash tashkiloti, The ICD-10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines (CDDG), 1992.
- ^ Amerika psixiatriya assotsiatsiyasi, Ruhiy kasalliklarning diagnostikasi va statistik qo'llanmasi, fourth edition, text revision (DSM-IV-TR), American Psychiatric Association, 2000.
- ^ Shibayama M (2011). "[Dissotsiativ kasalliklar va shizofreniya o'rtasidagi differentsial diagnostika]". Seishin Shinkeigaku Zasshi = Psychiatria et Neurologia Japonica. 113 (9): 906–11. PMID 22117396.
- ^ Jauch DA, Carpenter WT (February 1988). "Reactive psychosis. I. Does the pre-DSM-III concept define a third psychosis?". Asab va ruhiy kasalliklar jurnali. 176 (2): 72–81. doi:10.1097/00005053-198802000-00002. PMID 3276813. S2CID 35381672.
- ^ Jeronimus BF, Kotov R, Riese H, Ormel J (oktyabr 2016). "Neurotizmning ruhiy kasalliklar bilan istiqbolli aloqasi boshlang'ich alomatlar va psixiatrik tarixga moslashtirilgandan so'ng ikki baravar kamayadi, ammo tuzatilgan assotsiatsiya vaqt o'tishi bilan deyarli pasayib ketmaydi: 44 uzunlik / istiqbolli tadqiqotlarda 443 313 ishtirokchi bilan meta-tahlil". Psixologik tibbiyot. 46 (14): 2883–2906. doi:10.1017 / S0033291716001653. PMID 27523506.
- ^ a b v Pillmann F, Marneros A (2004). Acute and transient psychoses. Kembrij, Buyuk Britaniya: Kembrij universiteti matbuoti. p. 188. ISBN 978-0-521-83518-3. OCLC 144618418.
- ^ Lesser JM, Hughes S (December 2006). "Psychosis-related disturbances. Psychosis, agitation, and disinhibition in Alzheimer's disease: definitions and treatment options". Geriatriya. 61 (12): 14–20. PMID 17184138.
- ^ McKeith IG (February 2002). "Lyusi tanalari bilan demans". Britaniya psixiatriya jurnali. 180 (2): 144–7. doi:10.1192/bjp.180.2.144. PMID 11823325.
- ^ Wedekind S (June 2005). "[Depressive syndrome, psychoses, dementia: frequent manifestations in Parkinson disease]". MMW Fortschritte der Medizin (nemis tilida). 147 (22): 11. PMID 15977623.
- ^ a b v d Arciniegas DB (June 2015). "Psixoz". Davom etish. 21 (3 Behavioral Neurology and Neuropsychiatry): 715–36. doi:10.1212/01.CON.0000466662.89908.e7. PMC 4455840. PMID 26039850.
- ^ Lisanby SH, Kohler C, Swanson CL, Gur RE (January 1998). "Psychosis Secondary to Brain Tumor". Klinik neyropsikiyatriyadagi seminarlar. 3 (1): 12–22. PMID 10085187.
- ^ Evans DL, Mason KI, Leserman J, Bauer R, Petitto J (2002-02-01). "Chapter 90: Neuropsychiatric Manifestations of HIV-1 Infection and AIDS". Devis KL, Charney D, Coyle JT, Nemeroff C (tahrir). Nöropsikofarmakologiya: taraqqiyotning beshinchi avlodi (5-nashr). Filadelfiya: Lippincott Uilyams va Uilkins. pp. 1281–1301. ISBN 978-0-7817-2837-9. Arxivlandi asl nusxasi 2006-10-19 kunlari. Olingan 2006-10-16.
- ^ Nevin RL, Croft AM (June 2016). "Psychiatric effects of malaria and anti-malarial drugs: historical and modern perspectives". Bezgak jurnali. 15: 332. doi:10.1186/s12936-016-1391-6. PMC 4918116. PMID 27335053.
- ^ Friedrich F, Aigner M, Fearns N, Friedrich ME, Frey R, Geusau A (2014). "Psychosis in neurosyphilis -- clinical aspects and implications". Psixopatologiya. 47 (1): 3–9. doi:10.1159/000350059. PMID 23711816. S2CID 25903116.
- ^ Keshavan MS, Kaneko Y (February 2013). "Secondary psychoses: an update". Jahon psixiatriyasi. 12 (1): 4–15. doi:10.1002/wps.20001. PMC 3619167. PMID 23471787.
- ^ Sit D, Rothschild AJ, Wisner KL (May 2006). "A review of postpartum psychosis". Journal of Women's Health. 15 (4): 352–68. doi:10.1089/jwh.2006.15.352. PMC 3109493. PMID 16724884.
- ^ a b Foucher JR, Luck D (2006). "Psychosis related to neurological conditions: pro and cons of the dis- / mis-connectivity models of schizophrenia". Klinik nevrologiya sohasidagi suhbatlar. 8 (1): 17–27. doi:10.31887/DCNS.2006.8.1/jfoucher. PMC 3181754. PMID 16640110.
- ^ Bonnot O, Klünemann HH, Sedel F, Tordjman S, Cohen D, Walterfang M (April 2014). "Diagnostic and treatment implications of psychosis secondary to treatable metabolic disorders in adults: a systematic review". Noyob kasalliklar jurnali. 9: 65. doi:10.1186/1750-1172-9-65. PMC 4043981. PMID 24775716.
- ^ Sedel F, Baumann N, Turpin JC, Lyon-Caen O, Saudubray JM, Cohen D (October 2007). "Psychiatric manifestations revealing inborn errors of metabolism in adolescents and adults". Irsiy metabolik kasallik jurnali. 30 (5): 631–41. doi:10.1007/s10545-007-0661-4. PMID 17694356. S2CID 8419283.
- ^ Bonnot O, Herrera PM, Tordjman S, Walterfang M (2015). "Secondary psychosis induced by metabolic disorders". Nevrologiya chegaralari. 9: 177. doi:10.3389/fnins.2015.00177. PMC 4436816. PMID 26074754.
- ^ Jana DK, Romano-Jana L (October 1973). "Hypernatremic psychosis in the elderly: case reports". Amerika Geriatriya Jamiyati jurnali. 21 (10): 473–7. doi:10.1111/j.1532-5415.1973.tb01212.x. PMID 4729012. S2CID 766003.
- ^ Haensch CA, Hennen G, Jörg J (April 1996). "[Reversible exogenous psychosis in thiazide-induced hyponatremia of 97 mmol/l]". Der Nervenarzt. 67 (4): 319–22. PMID 8684511.
- ^ Hafez H, Strauss JS, Aronson MD, Holt C (June 1984). "Hypokalemia-induced psychosis in a chronic schizophrenic patient". Klinik psixiatriya jurnali. 45 (6): 277–9. PMID 6725222.
- ^ Konstantakos AK, Grisoni E (May 25, 2006). "Gipomagnezemiya". eTibbiyot. WebMD. Olingan 16 oktyabr, 2006.
- ^ Velasco PJ, Manshadi M, Breen K, Lippmann S (1 December 1999). "Psychiatric aspects of parathyroid disease". Psixosomatika. 40 (6): 486–90. doi:10.1016/S0033-3182(99)71186-2. PMID 10581976.
- ^ Rosenthal M, Gil I, Habot B (1997). "Primary hyperparathyroidism: neuropsychiatric manifestations and case report". Isroil psixiatriya va tegishli fanlari jurnali. 34 (2): 122–5. PMID 9231574.
- ^ Nanji AA (November 1984). "The psychiatric aspect of hypophosphatemia". Kanada psixiatriya jurnali. 29 (7): 599–600. doi:10.1177/070674378402900710. PMID 6391648. S2CID 39370705.
- ^ Padder T, Udyawar A, Azhar N, Jaghab K (December 2005). "Acute Hypoglycemia Presenting as Acute Psychosis". Onlaynda psixiatriya. Olingan 2006-09-27.
- ^ Losurdo G, Principi M, Iannone A, Amoruso A, Ierardi E, Di Leo A, Barone M (April 2018). "Çölyak bo'lmagan kleykovina sezgirligining ichakdan tashqaridagi ko'rinishlari: kengayib borayotgan paradigma". Jahon Gastroenterologiya jurnali (Sharh). 24 (14): 1521–1530. doi:10.3748 / wjg.v24.i14.1521. PMC 5897856. PMID 29662290.
- ^ Grant KM, LeVan TD, Wells SM, Li M, Stoltenberg SF, Gendelman HE, Carlo G, Bevins RA (March 2012). "Metamfetamin bilan bog'liq psixoz". Neyroimmun farmakologiya jurnali. 7 (1): 113–39. doi:10.1007 / s11481-011-9288-1. PMC 3280383. PMID 21728034.
- ^ Krebs TS, Johansen PØ (August 2013). "Psychedelics and mental health: a population study". PLOS ONE. 8 (8): e63972. Bibcode:2013PLoSO...863972K. doi:10.1371 / journal.pone.0063972. PMC 3747247. PMID 23976938.
- ^ Broderick P, Benjamin AB (December 2004). "Caffeine and psychiatric symptoms: a review". The Journal of the Oklahoma State Medical Association. 97 (12): 538–42. PMID 15732884.
- ^ Cardinal RN, Bullmore ET (2011). The Diagnosis of Psychosis. Kembrij universiteti matbuoti. p. 126. ISBN 978-1-139-49790-9.
- ^ Spirtli ichimliklar bilan bog'liq psixoz da eTibbiyot
- ^ Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G (July 2007). "Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review" (PDF). Lanset. 370 (9584): 319–28. doi:10.1016/S0140-6736(07)61162-3. PMID 17662880. S2CID 41595474.
- ^ Leweke FM, Koethe D (June 2008). "Cannabis and psychiatric disorders: it is not only addiction". Giyohvandlik biologiyasi. 13 (2): 264–75. doi:10.1111/j.1369-1600.2008.00106.x. PMID 18482435. S2CID 205400285.
- ^ Sewell RA, Ranganathan M, D'Souza DC (April 2009). "Cannabinoids and psychosis". Xalqaro psixiatriya sharhi. 21 (2): 152–62. doi:10.1080/09540260902782802. PMID 19367509. S2CID 8221928.
- ^ Henquet C, Di Forti M, Morrison P, Kuepper R, Murray RM (November 2008). "Gene-environment interplay between cannabis and psychosis". Shizofreniya byulleteni. 34 (6): 1111–21. doi:10.1093/schbul/sbn108. PMC 2632498. PMID 18723841.
- ^ McLaren JA, Silins E, Hutchinson D, Mattick RP, Hall W (January 2010). "Assessing evidence for a causal link between cannabis and psychosis: a review of cohort studies". The International Journal on Drug Policy. 21 (1): 10–9. doi:10.1016/j.drugpo.2009.09.001. PMID 19783132.
- ^ Ben Amar M, Potvin S (June 2007). "Cannabis and psychosis: what is the link?". Journal of Psychoactive Drugs. 39 (2): 131–42. doi:10.1080/02791072.2007.10399871. PMID 17703707. S2CID 21243420.
- ^ Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, Nosarti C, O' Carroll CM, Seal M, Allen P, Mehta MA, Stone JM, Tunstall N, Giampietro V, Kapur S, Murray RM, Zuardi AW, Crippa JA, Atakan Z, McGuire PK (February 2010). "Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology". Nöropsikofarmakologiya. 35 (3): 764–74. doi:10.1038/npp.2009.184. PMC 3055598. PMID 19924114.
- ^ Degenhardt L, Xoll V, Linski M (2001). "Nasha bilan psixoz o'rtasidagi komorbidlik: ba'zi mumkin bo'lgan munosabatlarni modellashtirish" (PDF). Technical Report No. 121. Sydney: National Drug and Alcohol Research Centre. Olingan 2006-08-19. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ Di Forti M, Sallis H, Allegri F, Trotta A, Ferraro L, Stilo SA, et al. (2014 yil noyabr). "Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users". Shizofreniya byulleteni. 40 (6): 1509–17. doi:10.1093/schbul/sbt181. PMC 4193693. PMID 24345517.
- ^ Dragt S, Nieman DH, Schultze-Lutter F, van der Meer F, Becker H, de Haan L, et al. (Yanvar 2012). "Cannabis use and age at onset of symptoms in subjects at clinical high risk for psychosis". Acta Psychiatrica Scandinavica. 125 (1): 45–53. doi:10.1111/j.1600-0447.2011.01763.x. PMID 21883099.
- ^ Glasner-Edwards, Suzette; Mooney, Larissa J. (2014). "Methamphetamine psychosis: epidemiology and management". CNS dorilar. 28 (12): 1115–1126. doi:10.1007/s40263-014-0209-8. ISSN 1179-1934. PMC 5027896. PMID 25373627.
- ^ Greening, David W.; Notaras, Michael; Chen, Maoshan; Xu, Rong; Smith, Joel D.; Cheng, Lesley; Simpson, Richard J.; Xill, Endryu F.; van den Buuse, Maarten (2019-12-10). "Chronic methamphetamine interacts with BDNF Val66Met to remodel psychosis pathways in the mesocorticolimbic proteome". Molekulyar psixiatriya: 1–17. doi:10.1038/s41380-019-0617-8. ISSN 1476-5578. PMID 31822818. S2CID 209169489.
- ^ Sander JW, Hart YM, Trimble MR, Shorvon SD (May 1991). "Vigabatrin and psychosis". Nevrologiya, neyroxirurgiya va psixiatriya jurnali. 54 (5): 435–9. doi:10.1136/jnnp.54.5.435. PMC 488544. PMID 1865207.
- ^ "Adderall XR ma'lumotlarini tayinlash" (PDF). Amerika Qo'shma Shtatlari oziq-ovqat va farmatsevtika idorasi. December 2013. pp. 4–6. Olingan 30 dekabr 2013.
- ^ Kuijpers HJ, van der Heijden FM, Tuinier S, Verhoeven WM (2007). "Meditation-induced psychosis". Psixopatologiya. 40 (6): 461–4. doi:10.1159/000108125. PMID 17848828. S2CID 38745071.
- ^ Moore MT, Nathan D, Elliott AR, Laubach C (1935). "Encephalographic studies in mental disease". Amerika psixiatriya jurnali. 92 (1): 43–67. doi:10.1176/ajp.92.1.43.
- ^ Fusar-Poli P, Radua J, McGuire P, Borgwardt S (November 2012). "Neuroanatomical maps of psychosis onset: voxel-wise meta-analysis of antipsychotic-naive VBM studies". Shizofreniya byulleteni. 38 (6): 1297–307. doi:10.1093/schbul/sbr134. PMC 3494061. PMID 22080494.
- ^ Palaniyappan L, Balain V, Liddle PF (October 2012). "The neuroanatomy of psychotic diathesis: a meta-analytic review". Psixiatriya tadqiqotlari jurnali. 46 (10): 1249–56. doi:10.1016/j.jpsychires.2012.06.007. PMID 22790253.
- ^ Radua J, Borgvardt S, Krescini A, Mataix-Cols D, Meyer-Lindenberg A, McGuire PK, Fusar-Poli P (Noyabr 2012). "Birinchi epizod psixozidagi miya tuzilishi va funktsional o'zgarishlarining multimodal meta-tahlili va antipsikotik dorilar ta'siri". Neyrologiya va biobehavioral sharhlar. 36 (10): 2325–33. doi:10.1016 / j.neubiorev.2012.07.012. PMID 22910680.
Patients with an FEP showed large and robust bilateral decreases of GMV in a peri-Sylvian cluster that included the insula, operculum and the superior temporal gyrus, and in the medial frontal and anterior cingulate cortices (MeF/ACC) (Fig. 2A and Supplementary Table S2). Patients had relatively greater GMV than controls in the right lingual gyrus and left precentral gyrus.
- ^ Bora E, Fornito A, Yücel M, Pantelis C (February 2012). "The effects of gender on grey matter abnormalities in major psychoses: a comparative voxelwise meta-analysis of schizophrenia and bipolar disorder". Psixologik tibbiyot. 42 (2): 295–307. doi:10.1017/S0033291711001450. PMID 21835091.
- ^ Del Casale A, Kotzalidis GD, Rapinesi C, Sorice S, Girardi N, Ferracuti S, Girardi P (2016). "Functional Magnetic Resonance Imaging Correlates of First-Episode Psychoses during Attentional and Memory Task Performance". Nöropsikobiologiya. 74 (1): 22–31. doi:10.1159/000448620. PMID 27698323. S2CID 5806628.
- ^ Radua et al. 2012 yil, 3.3. Changes in regional brain response to cognitive tasks. "In the anterior part of the right insula and in the dorsal ACC there was hypoactivation relative to controls, whereas in the right basal ganglia/thalamus extending to the posterior part of the insula and in the medial frontal cortex, there was a relative reduction in deactivation... Patients also showed reductions in deactivation in the right inferior frontal and left precentral gyri, as well as hypoactivation in left precuneus. ... The analyses of robustness showed that all these results were highly replicable, with the possible exception of the abnormalities in right inferior frontal gyrus..."
- ^ Radua et al. 2012 yil, 3.4. Multimodal analysis of grey matter volume and brain response."Spesifik ravishda, MeF / ACC ning izolyatsiyasining old qismlari va dorsal qismi gipoaktivatsiyani ko'rsatdi, insulalarning orqa qismlari va MeF / ACC ning ventral qismida deaktivatsiyaning pasayishi kuzatildi (3-rasm va 1-jadval). "
- ^ Braun G, Tompson V. "Shizofreniyada miyani funktsional tasvirlash: tanlangan natijalar va usullar". Sverdlovda N (tahrir). Shizofreniya xatti-harakatlarining neyrobiologiyasi va uni davolash. Springer. 185-189 betlar.
- ^ Naasan G. "Eluziyalar anatomiyasi". Lehner T, Miller B, shtat M (tahrir). Klinik neyropsikiyatriyadagi genomika, sxemalar va yo'llar. Elsevier Science. 366-369 betlar.
- ^ Radua J, Shmidt A, Borgvardt S, Xaynts A, Schlagenhauf F, McGuire P, Fusar-Poli P (dekabr 2015). "Psixozda mukofotni qayta ishlash jarayonida ventral striatal faollashuv: neyrofunktsional meta-tahlil". JAMA psixiatriyasi. 72 (12): 1243–51. doi:10.1001 / jamapsychiatry.2015.2196. PMID 26558708.
- ^ a b v Young J, Anticevic A, Barch D. "Psixotik buzilishlarning kognitiv va motivatsion nevrologiyasi". Charney D, Sklar P, Nestler E, Buxbaum J (tahrir). Ruhiy kasallikning neyrobiologiyasi (5-nashr). Oksford universiteti matbuoti.
- ^ a b Kapur S, Mizrahi R, Li M (noyabr 2005). "Dopamindan tortib to psixozgacha psixologiya - biologiya, farmakologiya va fenomenologiyani bog'lash". Shizofreniya tadqiqotlari. 79 (1): 59–68. doi:10.1016 / j.schres.2005.01.003. PMID 16005191. S2CID 2654713.
- ^ Egerton A, Fusar-Poli P, Stone JM (2012). "Glutamat va psixoz xavfi". Amaldagi farmatsevtika dizayni. 18 (4): 466–78. doi:10.2174/138161212799316244. PMID 22239577.
- ^ Bergeron R, Coyle JT (2012). "NAAG, NMDA retseptorlari va psixoz". Hozirgi dorivor kimyo. 19 (9): 1360–4. doi:10.2174/092986712799462685. PMC 3424071. PMID 22304714.
- ^ Adams RA, Stephan KE, Brown HR, Frith CD, Friston KJ (2013). "Psixozning hisoblash anatomiyasi". Psixiatriyadagi chegaralar. 4: 47. doi:10.3389 / fpsyt.2013.00047. PMC 3667557. PMID 23750138.
- ^ Corlett PR, Frith CD, Fletcher PC (2009 yil noyabr). "Giyohvandlikdan mahrum etishgacha: psixoz modellarini tushunish uchun Bayes asoslari". Psixofarmakologiya. 206 (4): 515–30. doi:10.1007 / s00213-009-1561-0. PMC 2755113. PMID 19475401.
- ^ Corlett PR, Honey GD, Krystal JH, Fletcher PC (yanvar 2011). "Glutamaterjik model psixozlari: bashorat qilishda xatolik, o'rganish va xulosa chiqarish". Nöropsikofarmakologiya. 36 (1): 294–315. doi:10.1038 / npp.2010.163. PMC 3055519. PMID 20861831.
- ^ Corlett PR, Teylor JR, Vang XJ, Fletcher Kompyuter, Krystal JH (2010 yil noyabr). "Xayollarning neyrobiologiyasiga qarshi". Neyrobiologiyada taraqqiyot. 92 (3): 345–69. doi:10.1016 / j.pneurobio.2010.06.007. PMC 3676875. PMID 20558235.
- ^ Kalkman HO, Loetscher E (2003 yil iyul). "GAD (67): GABA defitsiti gipotezasi va psixozning dopaminerjik va glutamaterjik nazariyalari o'rtasidagi bog'liqlik". Asab uzatish jurnali. 110 (7): 803–12. doi:10.1007 / s00702-003-0826-8. PMID 12811640. S2CID 31685339.
- ^ Akbarian S, Huang HS (2006 yil sentyabr). "Shizofreniya va unga bog'liq kasalliklarda o'zgargan GAD1 / GAD67 ekspresiyasining molekulyar va hujayra mexanizmlari". Miya tadqiqotlari bo'yicha sharhlar. 52 (2): 293–304. doi:10.1016 / j.brainresrev.2006.04.001. PMID 16759710. S2CID 25771139.
- ^ Jons XM, Pilovskiy LS (oktyabr 2002). "Dopamin va antipsikotik dori ta'sirini qayta ko'rib chiqish". Britaniya psixiatriya jurnali. 181 (4): 271–5. doi:10.1192 / bjp.181.4.271. PMID 12356650.
- ^ Soyka M, Zetzsche T, Dresel S, Tatsch K (may 2000). "FDG-PET va IBZM-SPECT talamik faollikni pasayishiga olib keladi, ammo surunkali alkogol gallyutsinozida dopaminerjik disfunktsiya mavjud emas". Nöropsikiyatriya va klinik nevrologiya jurnali. 12 (2): 287–8. doi:10.1176 / appi.neuropsych.12.2.287. PMID 11001615.
- ^ Zoldan J, Fridberg G, Livneh M, Melamed E (iyul 1995). "Oldinga Parkinson kasalligida psixoz: ondansetron bilan davolash, 5-HT3 retseptorlari antagonisti". Nevrologiya. 45 (7): 1305–8. doi:10.1212 / WNL.45.7.1305. PMID 7617188. S2CID 45540572.
- ^ Perry BI, McIntosh G, Weich S, Singh S, Rees K (Noyabr 2016). "Birinchi epizodli psixoz va g'ayritabiiy glyukemik nazorat o'rtasidagi bog'liqlik: tizimli tahlil va meta-tahlil" (PDF). Lanset. Psixiatriya. 3 (11): 1049–1058. doi:10.1016 / S2215-0366 (16) 30262-0. PMID 27720402.
- ^ Curran C, Byrappa N, McBride A (sentyabr 2004). "Stimulant psixoz: tizimli ko'rib chiqish". Britaniya psixiatriya jurnali. 185 (3): 196–204. doi:10.1192 / bjp.185.3.196. PMID 15339823.
- ^ a b Freydenreyx, Oliver (2012 yil 3-dekabr). "Psixotik simptomlarning differentsial diagnostikasi: tibbiy" mimika"". Psixiatrik Times. UBM Medica. Olingan 16 mart 2017.
- ^ Nordqvist C (2016 yil 8-avgust). "Shizoaffektiv buzilish nima? Shizoaffektiv buzuqlik nima?". Bugungi tibbiy yangiliklar. Olingan 16 mart, 2017.
- ^ Oziq-ovqat dori-darmonlarini boshqarish, HHS (2004 yil fevral). "Efedrin alkaloidlarini o'z ichiga olgan xun takviyasini aralashtirishni e'lon qilgan yakuniy qoida, chunki ular asossiz xavf tug'diradi. Yakuniy qoida". Federal reestr. 69 (28): 6787–854. PMID 14968803. (69 FR 6814 va 69 FR 6818 )
- ^ Umuman olganda JE, Gorham DR. Qisqa psixiatrik reyting shkalasi. Psixol Rep.1962; 10: 799-812
- ^ Kay SR, Fissbein A, Opler LA (1987). "Shizofreniya uchun ijobiy va salbiy sindrom o'lchovi (PANSS)". Shizofreniya byulleteni. 13 (2): 261–76. doi:10.1093 / schbul / 13.2.261. PMID 3616518.
- ^ a b Gaebel V, Zielasek J (mart 2015). "Psixozga e'tibor". Klinik nevrologiya sohasidagi suhbatlar. 17 (1): 9–18. doi:10.31887 / DCNS.2015.17.1 / wgaebel. PMC 4421906. PMID 25987859.
- ^ Marshall M, Rathbone J (iyun 2011). "Psixozga erta aralashuv". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (6): CD004718. doi:10.1002 / 14651858.CD004718.pub3. PMC 4163966. PMID 21678345.
- ^ NHS (2017-10-23). "Psixoz - oldini olish - NHS tanlovi". www.nhs.uk. Olingan 2018-10-15.
- ^ a b v van Os J, Kapur S (2009 yil avgust). "Shizofreniya". Lanset. 374 (9690): 635–45. doi:10.1016 / S0140-6736 (09) 60995-8. PMID 19700006. S2CID 208792724.
- ^ Stafford MR, Jekson X, Mayo-Uilson E, Morrison AP, Kendall T (yanvar 2013). "Psixozning oldini olish bo'yicha dastlabki choralar: tizimli tahlil va meta-tahlil". BMJ. 346: f185. doi:10.1136 / bmj.f185. PMC 3548617. PMID 23335473.
- ^ "Psixoz va shizofreniya xavfi bo'lgan odamlarga nutq terapiyasini taklif eting". Nice.org.uk. 2014-02-12. Olingan 2014-04-15.
- ^ "Kattalardagi psixoz va shizofreniya". Nice.org.uk. 2014-03-31. Olingan 2014-04-15.
- ^ Ruhiy salomatlik bo'yicha Milliy hamkorlik markazi (2009 yil 25 mart). "Shizofreniya: Birlamchi va ikkinchi darajali tibbiy yordamga asosiy aralashuvlar bo'yicha to'liq milliy klinik qo'llanma" (PDF). Olingan 25 noyabr 2009.
- ^ Keyn JM, Correll CU (2010). "Shizofreniyani farmakologik davolash". Klinik nevrologiya sohasidagi suhbatlar. 12 (3): 345–57. doi:10.31887 / DCNS.2010.12.3 / jkane. PMC 3085113. PMID 20954430.
- ^ Xartling L, Abou-Setta AM, Dursun S, Musavi SS, Pasichnyk D, Nyuton AS (oktyabr 2012). "Shizofreniya bilan kasallangan kattalardagi antipsikotiklar: birinchi avlod bilan ikkinchi avlod dori-darmonlarining qiyosiy samaradorligi: tizimli tahlil va meta-tahlil". Ichki tibbiyot yilnomalari. 157 (7): 498–511. doi:10.7326/0003-4819-157-7-201210020-00525. PMID 22893011.
- ^ a b v Barri SJ, Gaughan TM, Hunter R (iyun 2012). "Shizofreniya". BMJ klinik dalillari. 2012. PMC 3385413. PMID 23870705. Arxivlandi asl nusxasi 2014-09-11.
- ^ Schultz SH, Shimoliy SW, Shilds CG (iyun 2007). "Shizofreniya: sharh". Amerika oilaviy shifokori. 75 (12): 1821–9. PMID 17619525.
- ^ Smit T, Ueston S, Liberman J (avgust 2010). "Shizofreniya (davolashni davolash)". Amerika oilaviy shifokori. 82 (4): 338–9. PMID 20704164.
- ^ Teylor DM, Duncan-McConnell D (2000). "Olovga chidamli shizofreniya va atipik antipsikotiklar". Psixofarmakologiya jurnali. 14 (4): 409–18. doi:10.1177/026988110001400411. PMID 11198061. S2CID 27270415.
- ^ Picchioni MM, Murray RM (2007 yil iyul). "Shizofreniya". BMJ. 335 (7610): 91–5. doi:10.1136 / bmj.39227.616447.BE. PMC 1914490. PMID 17626963.
- ^ Essali A, Al-Haj Xasan N, Li S, Rathbone J (yanvar 2009). "Klozapin va shizofreniya uchun odatdagi neyroleptik dorilarga qarshi". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (1): CD000059. doi:10.1002 / 14651858.CD000059.pub2. PMC 7065592. PMID 19160174.
- ^ LG Ost (2014 yil oktyabr). "Qabul qilish va majburiyat terapiyasining samaradorligi: yangilangan tizimli tahlil va meta-tahlil". Xulq-atvorni o'rganish va terapiya. 61: 105–21. doi:10.1016 / j.brat.2014.07.018. PMID 25193001.
- ^ Kuper, Rut E.; Laxman, Neilam; Krellin, Nadiya; Monriff, Joanna; Priebe, Stefan (2019-05-21). "Shizofreniya yoki psixoz bilan og'rigan odamlarga antipsikotik dorilarni minimal yoki yo'qligi bo'yicha psixososial aralashuvlar: tizimli tahlil". Shizofreniya tadqiqotlari. doi:10.1016 / j.schres.2019.05.020. ISSN 0920-9964. PMID 31126806. S2CID 159040608. Olingan 2020-05-28.
- ^ Birchwood M, Todd P, Jekson S (1998). "Psixozga erta aralashish. Kritik davr gipotezasi". Britaniya psixiatriya jurnali. Qo'shimcha. 172 (33): 53–9. doi:10.1192 / S0007125000297663. PMID 9764127. S2CID 32411917.
- ^ a b Burgi M (noyabr 2008). "Psixoz tushunchasi: tarixiy va fenomenologik jihatlar". Shizofreniya byulleteni. 34 (6): 1200–10. doi:10.1093 / schbul / sbm136. PMC 2632489. PMID 18174608.
- ^ Pivo MD (iyun 1995). "Psixoz: ruhiy buzuqlikdan kasallik tushunchasiga". Psixiatriya tarixi. 6 (22 Pt 2): 177-200. doi:10.1177 / 0957154X9500602204. PMID 11639691. S2CID 36424931.
- ^ "Psixoz, Genri Jorj Liddell, Robert Skott, Yunoncha-inglizcha leksika, Perseyda ". Perseus.tufts.edu. Olingan 2011-06-11.
- ^ "Onlayn etimologiya lug'ati". Duglas Xarper. 2001 yil. Olingan 2006-08-19.
- ^ Berrios GE (1987 yil iyul). "Psixozlarning tarixiy jihatlari: 19-asr muammolari". Britaniya tibbiyot byulleteni. 43 (3): 484–98. doi:10.1093 / oxfordjournals.bmb.a072197. PMID 3322481.
- ^ Berrios GE, Pivo D (mart 1994). "Unitar psixoz tushunchasi: kontseptual tarix". Psixiatriya tarixi. 5 (17 Pt 1): 13-36. doi:10.1177 / 0957154X9400501702. PMID 11639278. S2CID 21417530.
- ^ Porter R (2003). Jinnilik: qisqacha tarix. AQSh: Oksford universiteti matbuoti. p. 10. ISBN 978-0-19-280267-5.
- ^ Vlachos IO, Beratis S, Hartocollis P (1997). "Magiko-diniy e'tiqod va psixoz". Psixopatologiya. 30 (2): 93–9. doi:10.1159/000285035. PMID 9168565.
- ^ Pfeifer S (1994 yil sentyabr). "Shveytsariyadagi psixiatrik bemorlarda jinlarga ishonish va exorcism". Britaniya tibbiyot psixologiyasi jurnali. 67 (3): 247–58. doi:10.1111 / j.2044-8341.1994.tb01794.x. PMID 7803317.
- ^ Gippokrat korpus
- ^ Bennet S (2008). "Klassik antik davrdagi aql va aqldan ozish". Psixiatriya va tibbiy psixologiya tarixi: 175–197. doi:10.1007/978-0-387-34708-0_3. ISBN 978-0-387-34707-3.
- ^ Bahor B, Vaynshteyn L, Limon M, Haskell A (1991). "Gipokratdan Kraepelinga qadar shizofreniya". Klinik psixologiya: 259–277. doi:10.1007/978-1-4757-9715-2_10. ISBN 978-1-4757-9717-6.
- ^ Rush B (1830). Aqliy kasalliklarga oid tibbiy so'rovlar va kuzatishlar. Filadelfiya. 98-190 betlar. ISBN 978-0-559-92167-4.
- ^ Qisqa, Edvard (1998). Psixiatriya tarixi: Boshpana davridan Prozak yoshigacha. Xoboken, Nyu-Jersi: John Wiley & Sons. ISBN 978-0-471-24531-5.
- ^ Stone JL (2001 yil mart). "Doktor Gotlib Burkxardt - psixoserurgiyaning kashshofi". Neuroscience tarixi jurnali. 10 (1): 79–92. doi:10.1076 / jhin.10.1.79.5634. PMID 11446267. S2CID 29727830.
- ^ Gross D, Schäfer G (2011 yil fevral). "Egas Moniz (1874-1955) va zamonaviy psixosurgiyaning" ixtirosi ": Portugaliyaning asl manbalarini alohida ko'rib chiqqan holda tarixiy va axloqiy qayta tahlil qilish". Neyroxirurgik diqqat. 30 (2): E8. doi:10.3171 / 2010.10.FOCUS10214. PMID 21284454.
- ^ a b Pressman JD (1998). Oxirgi kurort: psixoxirurgiya va tibbiyot chegaralari. Tibbiyot tarixidagi Kembrij tadqiqotlari. Kembrij, Buyuk Britaniya: Kembrij universiteti matbuoti. 18-40 betlar. ISBN 978-0-521-35371-7. OCLC 36729044.
- ^ Berrios GE (mart 1997). "Psixoxirurgiyaning kelib chiqishi: Shou, Burkxardt va Moniz". Psixiatriya tarixi. 8 (29 pt 1): 61-81. doi:10.1177 / 0957154X9700802905. PMID 11619209. S2CID 22225524.
- ^ Mashour GA, Walker EE, Martuza RL (iyun 2005). "Psixoxirurgiya: o'tmish, hozirgi va kelajak". Miya tadqiqotlari. Miya tadqiqotlari bo'yicha sharhlar. 48 (3): 409–19. doi:10.1016 / j.brainresrev.2004.09.002. PMID 15914249. S2CID 10303872.
- ^ Stip E (2002 yil may). "Nöroleptiklar tug'ilgan kuningiz bilan! 50 yildan so'ng: la folie du doute" Evropa psixiatriyasi. 17 (3): 115–9. doi:10.1016 / S0924-9338 (02) 00639-9. PMID 12052571.
- ^ Crossley NA, Constante M, McGuire P, Power P (iyun 2010). "Erta psixozni davolashda atipik va tipik antipsikotiklarning samaradorligi: meta-tahlil". Britaniya psixiatriya jurnali. 196 (6): 434–9. doi:10.1192 / bjp.bp.109.066217. PMC 2878818. PMID 20513851.
- ^ Maher AR, Maglione M, Bagley S, Suttorp M, Xu JH, Eving B, Vang Z, Timmer M, Sultzer D, Shekelle PG (sentyabr 2011). "Kattalar uchun yorliqdan tashqari foydalanish uchun atipik antipsikotik dorilarning samaradorligi va qiyosiy samaradorligi: tizimli tahlil va meta-tahlil". JAMA. 306 (12): 1359–69. doi:10.1001 / jama.2011.1360. PMID 21954480.
- ^ Reyx, Vilgelm, Belgilar tahlili, 437
- ^ Heali D (2002). Psixofarmakologiyaning yaratilishi. Kembrij: Garvard universiteti matbuoti. ISBN 978-0-674-00619-5.
Qo'shimcha o'qish
- Sims A (2002). Ongdagi alomatlar: tavsiflovchi psixopatologiya bilan tanishish (3-nashr). Edinburg: Elsevier Science Ltd. ISBN 978-0-7020-2627-0.
- Murray ED, Buttner N, Narx BH (aprel 2012). "Nevrologik amaliyotda depressiya va psixoz". Bredli WG, Daroff RB, Fenichel GM, Yankovich J (tahr.). Klinik amaliyotda nevrologiya (6-nashr). Butterworth Heinemann. ISBN 978-1-4377-0434-1.
- Uilyams P (2012). Jinnilikni qayta ko'rib chiqish: Psixozni tushunish va davolashda paradigma o'zgarishi tomon. Sky's Edge Publishing. ISBN 978-0-9849867-0-5.
- Shaxsiy hisob qaydnomalari
- Dik PK (1981). VALIS. London: Gollancz. ISBN 978-0-679-73446-8. [Yarim avtobiografik]
- Jeymison KR (1995). Tinch bo'lmagan aql: kayfiyat va aqldan ozish xotirasi. London: Pikador. ISBN 978-0-679-76330-7.
- Schreber DP (2000). Mening asabiy kasalligim haqidagi xotiralar. Nyu-York: Nyu-York kitoblarining sharhi. ISBN 978-0-940322-20-2.
- Hinshaw SP (2002). Sukunat yillari o'tdi: Otamning bipolyar buzuqlik bilan hayoti. Kembrij: Kembrij universiteti matbuoti.
- McLean R (2003). Davolanmagan shifo: Shizofreniya orqali sayohat. Avstraliya: Allen va Unvin. ISBN 978-1-86508-974-4.
- Saks ER (2007). Markaz ushlab turolmaydi - Mening aqldan ozgan sayohatim. Nyu-York: Hyperion. ISBN 978-1-4013-0138-5.
Tashqi havolalar
| Tasnifi | |
|---|---|
| Tashqi manbalar |
