Opioid - Opioid
| Opioid | |
|---|---|
| Giyohvand moddalar sinfi | |
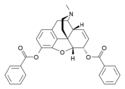
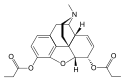
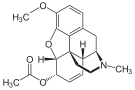
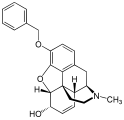
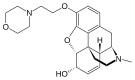
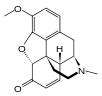
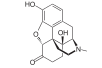
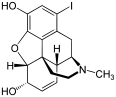
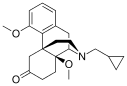
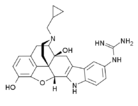
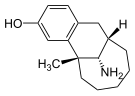
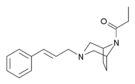
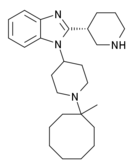
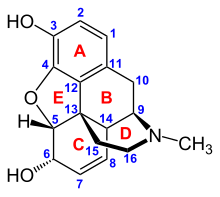
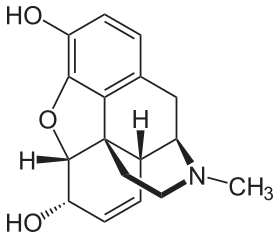 Morfinning kimyoviy tuzilishi, prototipik opioid.[1] | |
| Sinf identifikatorlari | |
| Foydalanish | Og'riqni yo'qotish |
| ATC kodi | N02A |
| Faoliyat tartibi | Opioid retseptorlari |
| Tashqi havolalar | |
| MeSH | D000701 |
| Vikidatada | |
Opioidlar etib borganda, ular moddalardir opioid retseptorlari, ta'siriga o'xshash effektlarga ega morfin.[2] Tibbiy jihatdan ular birinchi navbatda ishlatiladi og'riqni yo'qotish, shu jumladan behushlik.[3] Boshqa tibbiy maqsadlarda bostirish kiradi diareya, almashtirish terapiyasi opioiddan foydalanish buzilishi orqaga qaytarish opioidning haddan tashqari dozasi, yo'talni bostirish,[3] shu qatorda; shu bilan birga Qo'shma Shtatlarda ijro. Kabi juda kuchli opioidlar karfentanil faqat veterinariyada foydalanish uchun tasdiqlangan.[4][5][6] Opioidlar ular uchun tez-tez tibbiy bo'lmagan tarzda qo'llaniladi eyforik effektlar yoki oldini olish uchun chekinish.[7]
Opioidlarning yon ta'siri o'z ichiga olishi mumkin qichishish, tinchlantirish, ko'ngil aynish, nafas olish tushkunligi, ich qotishi va eyforiya. Uzoq muddatli foydalanish sabab bo'lishi mumkin bag'rikenglik, ya'ni bir xil ta'sirga erishish uchun dozalarning ko'payishi talab etiladi va jismoniy qaramlik, ya'ni preparatni to'satdan to'xtatish nojo'ya alomatlarga olib keladi.[8] Eforiya rekreatsion foydalanishni jalb qiladi va tez-tez o'sib boradigan, opioidlarning rekreatsion foydalanish odatda giyohvandlikka olib keladi. An dozani oshirib yuborish yoki boshqalar bilan bir vaqtda foydalanish depressant dorilar kabi benzodiazepinlar yoki spirtli ichimliklar odatda nafas olish tushkunligidan o'limga olib keladi.[9]
Opioidlar opioid retseptorlari bilan bog'lanish orqali harakat qiladi. Ular asosan markaziy va periferik asab tizimi va oshqozon-ichak trakti. Ushbu retseptorlar ikkala vositachilik qiladi psixoaktiv va opioidlarning somatik ta'siri. Opioid dorilariga quyidagilar kiradi qisman agonistlar, diareyaga qarshi dori kabi loperamid va antagonistlar kabi naloksegol opioid ta'sirida ich qotishi uchun. Ular kesib o'tolmaydilar qon-miya to'sig'i, ammo boshqa opioidlarni ushbu retseptorlarga bog'lashdan siqib chiqarishi mumkin.[iqtibos kerak ]
Dunyo bo'ylab har yili opioid dozasini oshirib yuborish natijasida 69000 kishi vafot etadi va 15 million kishi opioidga qaramdir.[10]
Opioidlar o'ziga qaram bo'lib, o'limga olib keladigan dozani oshirib yuborishi mumkinligi sababli, ko'pchilik boshqariladigan moddalar. 2013 yilda 28 dan 38 milliongacha odam opioidlardan noqonuniy foydalangan (15 yoshdan 65 yoshgacha bo'lgan dunyo aholisining 0,6% dan 0,8% gacha).[11] 2011 yilda Qo'shma Shtatlarda taxminan 4 million kishi opioidlardan rekreatsion foydalangan yoki ularga qaram bo'lgan.[12] 2015 yilga kelib, rekreatsion foydalanish va giyohvandlikning ko'payishi opioid dorilarining haddan tashqari retsepti va arzon taqiqlanganligi bilan bog'liq. geroin.[13][14][15] Aksincha, haddan tashqari buyurish, haddan tashqari oshirib yuborilgan nojo'ya ta'sirlar va opioidlarga qaramlikdan qo'rqish og'riqni etarli darajada davolashda ayblanmoqda.[16][17]
Terminologiya
Opioidlarga quyidagilar kiradi afyun, olingan bunday dorilarni nazarda tutadigan eski atama afyun, shu jumladan morfin o'zi.[18] Boshqa opioidlar yarim sintetik va sintetik kabi dorilar gidrokodon, oksikodon va fentanil; kabi antagonist dorilar nalokson; va endogen peptidlar kabi endorfinlar.[19] Shartlar afyun va giyohvandlik ba'zan opioid uchun sinonim sifatida uchraydi. Opiat to'g'ri tabiiy bilan cheklangan alkaloidlar qatronidan topilgan ko'knori garchi ba'zilariga yarim sintetik hosilalar kiradi.[18][20] Narkotik, "karaxtlik" yoki "uxlash" ma'nosidagi so'zlardan kelib chiqqan bo'lib, Amerika qonuniy atamasi sifatida kokain opioidlar va ularning manbalari. Shuningdek, u har qanday noqonuniy yoki nazorat ostida bo'lgan psixoaktiv dori-darmonlarga nisbatan yumshoq qo'llaniladi.[21][22] Ba'zi yurisdiktsiyalarda barcha nazorat ostidagi dorilar qonuniy ravishda tasniflanadi giyohvand moddalar. Bu atama mazmunli ma'noga ega bo'lishi mumkin va bu holda, odatda, foydalanish taqiqlanadi.[23][24]
Tibbiy maqsadlarda foydalanish
Og'riq
Zaif opioid kodein, past dozalarda va bir yoki bir nechta boshqa dorilar bilan birgalikda, odatda mavjud retseptsiz[25] va engil og'riqni davolash uchun ishlatilishi mumkin.[26] Boshqa opioidlar odatda o'rtacha va og'ir og'riqlarni yo'qotish uchun ajratilgan.[26]
O'tkir og'riq
Opioidlar o'tkir davolash uchun samarali og'riq (operatsiyadan keyingi og'riq kabi).[27] O'rtacha va og'ir o'tkir og'riqni tezda bartaraf etish uchun opioidlar tez-tez tanlanadi. Bu ularning tezkor boshlanishi, samaradorligi va qaramlik xavfining pasayishi bilan bog'liq. Shu bilan birga, yangi hisobotda opioid paytida uzoq vaqt davomida opioiddan foydalanish xavfi aniqlandi og'riq qoldiruvchi vositalar jarrohlik yoki travmadan keyin o'tkir og'riqni boshqarish uchun boshlangan.[28] Ular, shuningdek, muhim deb topildi palliativ yordam saraton va degenerativ holatlar kabi ba'zi bir terminal sharoitlarda paydo bo'lishi mumkin bo'lgan og'ir, surunkali, nogiron og'riqlarga yordam berish. romatoid artrit. Ko'pgina hollarda, opioidlar surunkali kasallarga uzoq muddatli parvarish qilishning muvaffaqiyatli strategiyasidir saraton og'rig'i.
AQShdagi barcha shtatlarning deyarli yarmidan ko'pi o'tkir og'riq uchun opioidni tayinlashni yoki tarqatishni cheklaydigan qonun chiqargan.[29]
Surunkali og'riqsiz saraton og'rig'i
Ko'rsatmalarga ko'ra, opioidlar xavfi ularning saratonga qarshi bo'lmagan surunkali kasalliklari uchun foydaliligidan ko'proq bo'lishi mumkin bosh og'rig'i, orqa og'riq va fibromiyalgiya.[30] Shunday qilib, ular surunkali saraton bo'lmagan og'riqlarda ehtiyotkorlik bilan ishlatilishi kerak.[31] Agar ishlatilsa, foyda va zararlar kamida uch oyda bir marta qayta ko'rib chiqilishi kerak.[32]
Surunkali og'riqni davolashda opioidlar - bu kamroq xavfli og'riq qoldiruvchi vositalar ko'rib chiqilgandan so'ng sinash uchun imkoniyatdir. Bunga quyidagilar kiradi paratsetamol / asetaminofen yoki NSAID kabi ibuprofen yoki naproksen.[33] Surunkali og'riqning ayrim turlari, shu jumladan sabab bo'lgan og'riq fibromiyalgiya yoki O'chokli, opioidlardan tashqari boshqa dorilar bilan davolash afzalroq.[34][35] Surunkali holatni kamaytirish uchun opioidlardan foydalanish samaradorligi neyropatik og'riq noaniq.[36]
Opioidlar bosh og'rig'ini davolashning birinchi usuli sifatida kontrendikedir, chunki ular hushyorlikni susaytiradi, qaramlik xavfini keltirib chiqaradi va epizodik bosh og'rig'i surunkali shaklga o'tish xavfini oshiradi.[37] Opioidlar shuningdek, bosh og'rig'iga yuqori sezuvchanlikni keltirib chiqarishi mumkin.[37] Boshqa muolajalar muvaffaqiyatsiz bo'lganda yoki mavjud bo'lmaganda, bemorni surunkali bosh og'rig'ini rivojlanishiga yo'l qo'ymaslik uchun kuzatilishi mumkin bo'lsa, bosh og'rig'ini davolash uchun opioidlar mos kelishi mumkin.[37]
Xavfli bo'lmagan kasalliklarni davolashda opioidlar tez-tez ishlatiladi surunkali og'riq.[38][39][40] Ushbu amaliyot endi giyohvandlik va opioidlarni noto'g'ri ishlatish bilan bog'liq yangi va o'sib borayotgan muammoga olib keldi.[31][41] Turli xil salbiy ta'sirlar tufayli surunkali og'riqni uzoq muddat boshqarish uchun opioidlardan foydalanish, agar unchalik xavfli bo'lmagan og'riq qoldiruvchi vositalar samarasiz deb topilmasa. Faqatgina vaqti-vaqti bilan yuzaga keladigan surunkali og'riq, masalan asab og'rig'i, O'chokli va fibromiyalgiya, tez-tez opioidlardan boshqa dorilar bilan yaxshi davolanadi.[34] Paratsetamol va nosteroid yallig'lanishga qarshi dorilar shu jumladan ibuprofen va naproksen xavfsizroq alternativalar deb hisoblanadi.[42] Ular opioidlar bilan birgalikda tez-tez ishlatiladi, masalan, paratsetamol bilan birgalikda oksikodon (Perkotset ) va ibuprofen bilan birlashtirilgan gidrokodon (Vikoprofen ), qaysi og'riqni kamaytirishni kuchaytiradi shuningdek, rekreatsion foydalanishni to'xtatish uchun ham mo'ljallangan.[43][44]
Boshqalar
Yutalish
Kodein ilgari yo'talni bostiruvchi vositalarda "oltin standart" sifatida qaraldi, ammo hozirda bu holat shubha ostiga olinadi.[45] Ba'zi yaqinda platsebo - nazorat ostida o'tkazilgan tekshiruvlar natijasida ba'zi sabablarga ko'ra plasebodan yaxshiroq bo'lmasligi mumkin, shu jumladan bolalardagi o'tkir yo'tal.[46][47] Shunday qilib, bolalar uchun tavsiya etilmaydi.[47] Bundan tashqari, bunga dalil yo'q gidrokodon bolalarda foydalidir.[48] Xuddi shunday, 2012 yilgi Gollandiyada o'tkir yo'talni davolash bo'yicha ko'rsatma ham uni ishlatishni tavsiya etmaydi.[49] (Opioid analogi dekstrometorfan, uzoq vaqt davomida kodein kabi samarali yo'talni bostiruvchi vosita deb da'vo qilgan,[50] yaqinda o'tkazilgan bir qator tadqiqotlarda xuddi shunday foyda keltirmadi.[51])
Kam miqdordagi morfin surunkali yo'talga yordam berishi mumkin, ammo uni qo'llash nojo'ya ta'sirlar bilan cheklanadi.[52]
Diareya va ich qotishi
Diareya holatlarida ustunlik qiladi irritabiy ichak sindromi, diareyani bostirish uchun opioidlardan foydalanish mumkin. Loperamid a periferik tanlangan opioid mavjud retseptsiz va diareyani bostirish uchun ishlatiladi.
Diareyani bostirish qobiliyati, shuningdek, opioidlar bir necha haftadan keyin ishlatilganda ich qotishini keltirib chiqaradi.[53] Naloksegol, endi opioid kelib chiqadigan ich qotishini davolash uchun periferik-selektiv opioid antagonisti mavjud.[54]
Nafas qisilishi
Opioidlar yordam berishi mumkin nafas qisilishi ayniqsa, saraton va kabi rivojlangan kasalliklarda KOAH Boshqalar orasida.[55][56]
Yomon ta'sir
Boshqalar
- Kognitiv effektlar
- Opioidga qaramlik
- Bosh aylanishi
- Ishtahani yo'qotish
- Oshqozonni bo'shatish kechiktirildi
- Jinsiy aloqani kamaytirish
- Jinsiy funktsiya buzilgan
- Testosteron darajasining pasayishi
- Depressiya
- Immunitet tanqisligi
- Og'riqqa sezgirlikni oshirish
- Noqonuniy hayz ko'rish
- Xavfining oshishi tushadi
- Sekin nafas olish
- Koma
Keksa kattalarda opioiddan foydalanish "sedasyon, ko'ngil aynishi, qusish, ich qotishi, siydikni ushlab turish va tushish" kabi salbiy ta'sirlarni kuchayishi bilan bog'liq.[58] Natijada, opioidlarni qabul qiladigan keksa yoshdagi odamlar shikastlanish xavfi yuqori.[59] Opioidlar, masalan, boshqa ko'plab dori-darmonlardan farqli o'laroq, o'ziga xos organ toksikligini keltirib chiqarmaydi aspirin va paratsetamol. Ular yuqori oshqozon-ichak trakti qon ketishi va buyrak toksikligi bilan bog'liq emas.[60]
O'tkir bel og'rig'i va artrozni davolash uchun opioidlarning retsepti uzoq muddatli salbiy ta'sirga ega bo'lib tuyuladi[61][62]
Opioidga qaram bo'lgan onalardan tug'ilgan bolalar, ayniqsa metadon buyurilganlar, asab rivojlanishining buzilishi xavfi ostida, ruhiy rivojlanish indekslari va psixomotor rivojlanish indekslari ochilmagan bolalarga qaraganda pastroq.[63]
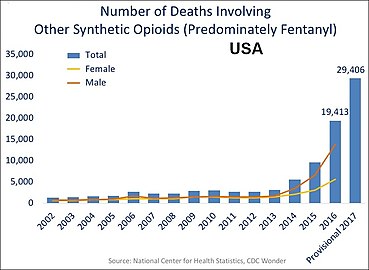
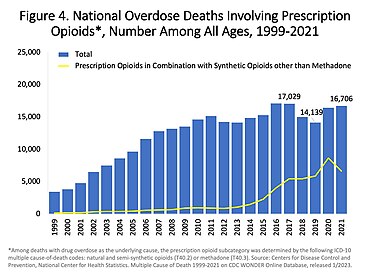
Tadqiqotlar shuni ko'rsatadiki, qachon metadon uzoq vaqtdan beri qo'llaniladi, u tanada oldindan aytib bo'lmaydigan darajada to'planib, o'lik nafasni sekinlashtirishi mumkin.[64][65] Tibbiy jihatdan foydalanilsa, toksikaning yaqinlashishi tan olinmaydi, chunki og'riq qoldiruvchi dorilar ta'sir preparatning yo'q bo'lishidan ancha oldin tugaydi.[66] Ga ko'ra USCDC, metadon 1999-2010 yillarda AQShda opioid bilan bog'liq o'limning 31 foizida qatnashgan va 40 foizga yagona dori sifatida jalb qilingan, bu boshqa opioidlarga qaraganda ancha yuqori.[67] Uzoq muddatli opioidlarni o'rganish shuni ko'rsatdiki, noxush hodisalar odamlarni uzoq vaqt davomida opioidlarni qabul qilishni to'xtatishi mumkin.[68] Qo'shma Shtatlarda 2016 yilda opioidning haddan tashqari dozasi 10000 kishidan 1,7 kishining o'limiga olib keldi.[69]
AQSh o'lchovlari jadvalida ko'plab o'limlar bir nechta opioidlarni o'z ichiga oladi:

AQShda geroin bilan bog'liq har yili haddan tashqari dozada o'lim.[70]
Kuchaytirishning buzilishi
Bag'rikenglik
Bag'rikenglik bilan xarakterlanadigan jarayondir neyroadaptatsiyalar natijada giyohvand moddalar ta'siri kamayadi. Esa retseptorlari regulyatsiyasi ko'pincha muhim rol o'ynashi mumkin, boshqa mexanizmlar ham ma'lum.[72] Tolerantlik boshqalarnikiga qaraganda ba'zi ta'sirlar uchun ko'proq seziladi; bag'rikenglik kayfiyat, qichishish, siydikni ushlab turish va nafas olish tushkunligiga ta'sirida asta-sekin paydo bo'ladi, ammo analjeziya va boshqa jismoniy yon ta'sirlarda tezroq yuz beradi. Biroq, bag'rikenglik kabızlığa yoki rivojlanmaydi mioz (ko'z qorachig'ining torayishi ikki millimetrdan kam yoki unga teng). Biroq, ushbu g'oya e'tirozga uchradi, ammo ba'zi mualliflar bu bag'rikenglik haqida bahslashishdi qiladi miozgacha rivojlanadi.[73]
Opioidlarga chidamlilik bir qator moddalar bilan susayadi, jumladan:
- kaltsiy kanal blokerlari[74][75][76]
- intratekal magniy[77][78] va rux[79]
- NMDA antagonistlari, kabi dekstrometorfan, ketamin,[80] va memantin.[81]
- xoletsistokinin antagonistlari, kabi proglumid[82][83][84]
- Kabi yangi agentlar fosfodiesteraza inhibitori ibudilast ushbu dastur uchun ham tadqiq qilingan.[85]
Tolerantlik - bu fiziologik jarayon, bu organizm tez-tez mavjud bo'lgan dori-darmonlarga moslashadi. Odatda bir xil ta'sirga erishish uchun vaqt o'tishi bilan bir xil dorilarning yuqori dozalari talab qilinadi. Odamlar uchun uzoq vaqt davomida yuqori miqdorda opioidlarni qabul qilish odatiy holdir. Biroq, bu suiiste'mol qilish yoki giyohvandlikning har qanday munosabatini taxmin qilmaydi. Avstraliyada o'tkazilgan retrospektiv kohort tadqiqotlari shuni ko'rsatdiki, tarqatish birinchi oyda tugamagan bo'lsa, keyingi davrda tarqatish ehtimoli juda yuqori bo'lib qoldi. Birinchi oyda tarqatish epizodlarining miqdori va soni keyingi davrda tarqatishning umumiy davomiyligini sezilarli darajada bashorat qilgan.[86]
Jismoniy qaramlik
Jismoniy qaramlik bu organizmning fiziologik moslashuvi, bu holda, opioid dori. Bu modda to'xtatilganda, dozani keskin kamaytirganda yoki, ayniqsa opioidlar holatida, antagonist bo'lganida, olib tashlash alomatlarini rivojlanishi bilan belgilanadi (masalan., nalokson ) yoki agonist-antagonist (masalan., pentazotsin ) boshqariladi. Jismoniy qaramlik ba'zi dorilarning odatiy va kutilgan jihati bo'lib, bemorning o'ziga qaramligini anglatmaydi.
Opiatlarni olib tashlash alomatlari og'ir bo'lishi mumkin disforiya, boshqa afyun dozasini istash, asabiylashish, terlash, ko'ngil aynish, rinorea, titroq, qusish va mialgiya. Bir necha kun va haftalar davomida opioidlarni iste'mol qilishni asta-sekin kamaytirish, olib tashlash alomatlarini kamaytirishi yoki yo'q qilishi mumkin.[87] Chiqib ketish tezligi va zo'ravonligi opioidning yarim umriga bog'liq; geroin va morfinni olib tashlash tezroq sodir bo'ladi metadon chekinish. O'tkir tushkunlik bosqichi ko'pincha bir necha oy davom etishi mumkin bo'lgan depressiya va uyqusizlikning uzaygan bosqichiga to'g'ri keladi. Opioidni olib tashlash belgilari boshqa dorilar bilan davolash mumkin, masalan klonidin.[88] Jismoniy qaramlik giyohvand moddalarni suiiste'mol qilishni yoki haqiqiy giyohvandlikni bashorat qilmaydi va bag'rikenglik mexanizmi bilan chambarchas bog'liqdir. Bilan nafaqa berish to'g'risidagi latifaviy da'volar mavjud bo'lsa-da ibogain, uning moddaga bog'liqlikda foydalanilishini qo'llab-quvvatlovchi ma'lumotlar yomon.[89]
Muntazam ravishda opioid dozalarini olgan tanqidiy bemorlarda tez-tez uchraydigan sindrom sifatida yatrogenik ajralish kuzatiladi.[90]
Giyohvandlik
Giyohvandlik bu odatda ba'zi dorilarni suiiste'mol qilish bilan bog'liq bo'lgan, vaqt o'tishi bilan rivojlanib boradigan va yuqori dori dozalari bilan bog'liq bo'lgan xatti-harakatlarning murakkab to'plamidir. Giyohvandlik psixologik majburlashni o'z ichiga oladi, bu esa azob chekayotgan odam xavfli yoki zararli oqibatlarga olib keladigan harakatlarida davom etaveradi. Opioidga qaramlik o'z ichiga oladi etishmovchilik tibbiy sabablarga ko'ra buyurilgan opioidlarni og'iz orqali qabul qilish o'rniga yoki in'ektsiya.[87]
Avstriya, Bolgariya va Slovakiya singari Evropa davlatlarida buprenorfinning yon ta'siriga toqat qilmaydigan bemorlar uchun afyun o'rnini bosuvchi terapiyada (OST) sekin chiqariladigan og'iz morfin formulalari qo'llaniladi. metadon. Buprenorfin bilan birga ham ishlatilishi mumkin nalokson giyohvandlikni uzoqroq davolash uchun. Boshqa Evropa mamlakatlarida, shu jumladan Buyuk Britaniyada, bu OST uchun qonuniy ravishda qo'llaniladi, ammo qabul qilishning har xil miqyosida.
Sekin-asta chiqariladigan dorilarning tarkibi suiiste'mol qilish va giyohvandlik darajasini kamaytirishga qaratilgan bo'lib, og'riqli bemorlarga qonuniy og'riqni kamaytirish va ulardan foydalanish qulayligini ta'minlashga harakat qilmoqda. Biroq, ushbu turdagi preparatlarning samaradorligi va xavfsizligi to'g'risida savollar qolmoqda. Hozirgi vaqtda buzishga chidamli dori-darmonlarni FDA tomonidan bozor tomonidan tasdiqlash uchun sinovlar ko'rib chiqilmoqda.[91][92]
Mavjud dalillar miqdori faqat zaif xulosa chiqarishga imkon beradi, ammo bu tarixiy bo'lmagan bemorlarda opioiddan foydalanishni to'g'ri boshqaradigan shifokorni taklif qiladi. moddaga bog'liqlik yoki giyohvand moddalarni suiiste'mol qilish giyohvandlik, suiiste'mol yoki boshqa jiddiy yon ta'sirlarni rivojlanish xavfi kam bo'lgan holda uzoq muddatli og'riqni kamaytirishi mumkin.[68]
Opioidlar bilan bog'liq muammolar quyidagilarni o'z ichiga oladi:
- Ba'zi odamlar opioidlar barcha og'riqlarini engillashtirmasligini payqashadi.[93]
- Ba'zi odamlar opioidlarning nojo'ya ta'sirlari terapiyadan ko'proq foyda keltiradigan muammolarni keltirib chiqaradi[68]
- Ba'zi odamlar vaqt o'tishi bilan opioidlarga nisbatan bag'rikenglikni shakllantiradilar. Bu ularga foydani saqlab qolish uchun dori dozalarini oshirishni talab qiladi va bu o'z navbatida istalmagan yon ta'sirlarni kuchaytiradi.[68]
- Opioiddan uzoq muddatli foydalanish sabab bo'lishi mumkin opioid bilan bog'liq giperaljeziya, bu bemorning og'riqqa sezgirligini oshiradigan holat.[94]
Barcha opioidlar yon ta'sirga olib kelishi mumkin.[57] Og'riqni kamaytirish uchun opioidlarni qabul qiladigan bemorlarda tez-tez uchraydigan nojo'ya reaktsiyalarga quyidagilar kiradi ko'ngil aynish va qusish, uyquchanlik, qichima, quruq og'iz, bosh aylanishi va ich qotishi.[57][87]
Bulantı va gijjalar
Bardoshlik ko'ngil aynish 7-10 kun ichida sodir bo'ladi, bu davrda qusishga qarshi vositalar juda samarali bo'ladi.[iqtibos kerak ] Tardiv diskineziya kabi jiddiy yon ta'sirlar tufayli haloperidol kamdan kam qo'llaniladi. Bilan bog'liq dori, proxlorperazin shunga o'xshash xavfga ega bo'lsa-da, tez-tez ishlatiladi. Kabi kuchli antiemetika ondansetron yoki tropisetron ba'zida ko'ngil aynish og'ir yoki doimiy va bezovta qiladigan bo'lsa ham, ularning narxi yuqori bo'lishiga qaramay qo'llaniladi. Arzonroq alternativa dopamin antagonistlari, masalan, domperidon va metoklopramid. Domperidon kesib o'tmaydi qon-miya to'sig'i va markaziy antidopaminerjik ta'sirni keltirib chiqaradi, ammo opioid emetik ta'sirini bloklaydi chemoreceptor trigger zonasi. (Preparat AQShda mavjud emas) Antikolinerjik xususiyatlarga ega bo'lgan ba'zi antihistaminiklar (masalan. orfenadrin yoki difenhidramin) ham samarali bo'lishi mumkin. Birinchi avlod antihistaminik gidroksizin juda tez-tez ishlatiladi, bu harakatning buzilishini keltirib chiqarmaslikning qo'shimcha afzalliklari bilan, shuningdek analjezikni saqlovchi xususiyatlarga ega. Δ9-tetrahidrokannabinol ko'ngil aynishi va qayt qilishni ketkazadi;[95][96] shuningdek, ko'ngil aynish va gijjalar kamaygan opioidlarning past dozalarini olishiga imkon beradigan og'riq qoldiruvchi vositalarni ishlab chiqaradi.[97][98]
- 5-HT3 antagonistlar (masalan. ondansetron )
- Dopamin antagonistlari (masalan. domperidon )
- Xolinergik antigistaminlar (masalan. dimedrol )
- Δ9-tetrahidrokannabinol (masalan. dronabinol )
Gijjalar tufayli oshqozon staziyasi (katta hajmdagi qusish, qusish bilan qisqa muddatli ko'ngil aynish, qizilo'ngach reflyuksiyasi, epigastral to'lish, erta to'yish), to'g'ridan-to'g'ri ta'sir qilishdan tashqari chemoreceptor trigger zonasi ning hudud postrema, miyaning qusish markazi. Shunday qilib prokinetik agentlar tomonidan qusishni oldini olish mumkin (masalan. domperidon yoki metoklopramid ). Agar gijjalar allaqachon boshlangan bo'lsa, ushbu preparatlarni og'iz orqali yuborish kerak (masalan. metoklopramid uchun teri osti, domperidon uchun rektal).
- Prokinetik vositalar (masalan. domperidon )
- Xolinergik vositalar (masalan. orfenadrin )
Dalillarga ko'ra, opioid-inkluziv behushlik operatsiyadan keyingi ko'ngil aynishi va qayt qilish bilan bog'liq.[99]
Opioidlardan foydalangan holda surunkali og'riqlar bilan og'rigan bemorlarda og'riq va jismoniy faoliyati biroz yaxshilangan va qusish xavfi ortgan.[100]
Uyquchanlik
Bardoshlik uyquchanlik odatda 5-7 kun ichida rivojlanadi, ammo muammoli bo'lsa, muqobil opioidga o'tish ko'pincha yordam beradi. Kabi ba'zi bir opioidlar fentanil, morfin va diamorfin (geroin) ayniqsa tinchlantiruvchi xususiyatga ega, boshqalari esa oksikodon, tilidin va meperidin (pethidine) nisbatan kam sedasyon ishlab chiqarishga moyil, ammo bemorlarning individual javoblari sezilarli darajada farq qilishi mumkin va ma'lum bir bemor uchun eng munosib dori-darmonni topish uchun ba'zi sinov va xatolarga ehtiyoj sezilishi mumkin. Aks holda, davolanish CNS stimulyatorlar umuman samarali.[101][102]
- Stimulyatorlar (masalan. kofein, modafinil, amfetamin, metilfenidat )
Qichishish
Qichishish opioidlar og'riqni kamaytirish uchun ishlatilganda jiddiy muammo bo'lishga moyil emas, ammo antigistaminlar paydo bo'lganda qichishish bilan kurashish uchun foydalidir. Feksofenadin kabi sedativ bo'lmagan antigistaminlarga ko'pincha afzallik beriladi, chunki ular opioid ta'sirida uyquchanlikni kuchaytiradi. Biroq, ba'zi sedativ antigistaminlar orfenadrin opioidlarning kichik dozalarini qo'llashga imkon beradigan sinergetik og'riqni kamaytiruvchi ta'sirni keltirib chiqarishi mumkin. Binobarin, opioid / antigistamin kombinatsiyasining bir nechta mahsulotlari, masalan Meprozin (meperidin /prometazin ) va Dikonal (dipipanon /siklizin ), va ular opioid bilan bog'liq ko'ngil aynishini kamaytirishi mumkin.
- Antigistaminlar (masalan. feksofenadin )
Kabızlık
Opioid bilan bog'liq ich qotishi (OIC) uzoq muddatli opioidlarni qabul qiladigan odamlarning 90 dan 95 foizigacha rivojlanadi.[103] Ushbu muammoga nisbatan bag'rikenglik umuman rivojlanmaganligi sababli, uzoq muddatli opioidlarga ega bo'lganlarning ko'pchiligi a laksatif yoki klizmalar.[104]
OICni davolash ketma-ket va zo'ravonlikka bog'liq.[105] Davolashning birinchi usuli farmakologik emas va tobora ortib borayotgan turmush tarzini o'zgartirishni o'z ichiga oladi xun tolasi, suyuqlikni iste'mol qilish (kuniga 1,5 L (51 AQSh oz oz)) va jismoniy faoliyat.[105] Agar farmakologik bo'lmagan choralar samarasiz bo'lsa, laksatiflar, shu jumladan najasni yumshatuvchi moddalar (masalan., polietilen glikol ), massa hosil qiluvchi laksatiflar (masalan., tolali qo'shimchalar ), stimulyator laksatiflari (masalan., bisakodil, senna ) va / yoki klizmalar, ishlatilishi mumkin.[105] OIC uchun keng tarqalgan laksatif rejim bu dokusat va bisakodil birikmasidir.[105][106][107][yangilanishga muhtoj ] Osmotik laksatiflar, shu jumladan laktuloza, polietilen glikol va magneziya suti (magniy gidroksidi), shuningdek mineral moy (a moylash uchun laksatif ), shuningdek, odatda IHT uchun ishlatiladi.[106][107]
Periferik ta'sir qiluvchi u-opioid retseptorlari antagonisti OIC bo'lgan bemorlar uchun samarali va bardoshli ekanligi isbotlangan.[108]
Agar laksatiflar etarli darajada samarasiz bo'lsa (ko'pincha shunday bo'ladi),[109] periferik-selektivni o'z ichiga olgan opioid formulalari yoki sxemalari opioid antagonisti, kabi metilnaltrekson bromidi, naloksegol, alvimopan, yoki nalokson (kabi.) oksikodon / nalokson ), sud qilinishi mumkin.[105][107][110] 2018 yilgi Cochrane tekshiruvi shuni ko'rsatdiki, dalillar alvimopan, nalokson yoki metilnaltrekson bromidi uchun taxminiy bo'lgan.[111] Og'iz orqali nalokson eng samarali bo'lib ko'rinadi.[112] Kundalik 0,2 mg naldemedinning dozasi OIC bo'lgan bemorlarda simptomlarni sezilarli darajada yaxshilashi ko'rsatilgan.[113]
Opioidning aylanishi uzoq muddatli foydalanuvchilarda ich qotishining ta'sirini kamaytirish uchun tavsiya etilgan usullardan biri.[114] Barcha opioidlar konstipatsiyani keltirib chiqarsa-da, tadqiqotlar shuni ko'rsatadiki, giyohvand moddalar o'rtasida ba'zi farqlar mavjud tramadol, tapentadol, metadon va fentanil bilan nisbatan kamroq konstipatsiyaga olib kelishi mumkin kodein, morfin, oksikodon yoki gidromorfon ich qotishi nisbatan og'irroq bo'lishi mumkin.
Nafas olish depressiyasi
Nafas olish depressiyasi opioidni qo'llash bilan bog'liq bo'lgan eng jiddiy nojo'ya reaktsiya, ammo odatda opioid-naiv bemorda tomir ichiga yuboriladigan bitta dozada kuzatiladi. Og'riqni kamaytirish uchun muntazam ravishda opioidlarni qabul qiladigan bemorlarda nafas olish depressiyasiga chidamlilik tezda yuzaga keladi, shuning uchun bu klinik muammo emas. Nafas olish depressiyasini qisman blokirovka qilishi mumkin bo'lgan bir nechta dorilar ishlab chiqilgan, ammo hozirda ushbu maqsad uchun tasdiqlangan yagona nafas olish stimulyatori doxapram, bu ushbu dasturda faqat cheklangan samaradorlikka ega.[115][116] Kabi yangi dorilar BIMU-8 va CX-546 ancha samarali bo'lishi mumkin.[117][118][119][birlamchi bo'lmagan manba kerak ]
- Nafas olish stimulyatorlari: karotisli xemoretseptor agonistlari (masalan. doxapram ), 5-HT4 agonistlar (masalan. BIMU8 ), b-opioid agonistlari (masalan. BW373U86 ) va AMPAkines (masalan. CX717 ) analjezikaga ta'sir qilmasdan opioidlar tomonidan kelib chiqqan nafas olish depressiyasini kamaytirishi mumkin, ammo bu dorilarning aksariyati faqat o'rtacha darajada samarali yoki odamlarda foydalanishni istisno qiladigan yon ta'sirga ega. 5-HT1A kabi agonistlar 8-OH-DPAT va repinotan shuningdek, opioid ta'siridagi nafas olish depressiyasiga qarshi kurashadi, ammo shu bilan birga analjeziyani kamaytiradi, bu ularning ushbu dastur uchun foydaliligini cheklaydi.
- Opioid antagonistlari (masalan. nalokson, nalmefen, diprenorfin )
Opioid yuborilgandan keyingi dastlabki 24 soat hayot uchun xavfli bo'lgan OIRD bilan bog'liq eng muhim bo'lib ko'rinadi, ammo opioiddan foydalanishga nisbatan ehtiyotkorlik bilan yondoshish bilan oldini olish mumkin.[120]
Yurak, nafas yo'llari kasalligi va / yoki obstruktiv uyqu apnesi bo'lgan bemorlarda OIRD xavfi yuqori.[121]
Og'riqqa sezgirlikni oshirish
Opioid bilan bog'liq giperaljeziya - bu erda og'riqni engillashtirish uchun opioidlardan foydalanadigan shaxslar paradoksal ravishda ushbu dorilar natijasida ko'proq og'riqni boshdan kechirish - ba'zi odamlarda kuzatilgan. Ushbu hodisa, kamdan-kam uchraydigan bo'lsa ham, ba'zi odamlarni qabul qilishda kuzatiladi palliativ yordam, ko'pincha dozani tez oshirganda.[122][123] Agar duch kelsa, turli xil opioidli og'riqli dorilar o'rtasida aylanish rivojlanishning pasayishiga olib kelishi mumkin og'riqni kuchaytirdi.[124][125] Opioid bilan bog'liq giperaljeziya tez-tez surunkali foydalanish yoki qisqa muddatli yuqori dozalarda yuzaga keladi, ammo ba'zi tadqiqotlar shuni ko'rsatadiki, bu juda past dozalarda ham bo'lishi mumkin.[126][127]
Giperaljeziya va kabi nojo'ya ta'sirlar allodiniya, ba'zan yomonlashuvi bilan birga keladi neyropatik og'riq, opioidli analjeziklar bilan uzoq muddatli davolanishning oqibatlari bo'lishi mumkin, ayniqsa, bag'rikenglikni oshirish samaradorlikni yo'qotishiga va natijada vaqt o'tishi bilan dozani ko'payishiga olib keladi. Bu asosan opioid retseptorlari, shu jumladan uchta klassik opioid retseptorlaridan tashqari, maqsadga qaratilgan opioid dorilarining ta'siridan kelib chiqadi. nosiseptin retseptorlari, sigma retseptorlari va Pullik kabi retseptorlari 4, va shunga o'xshash antagonistlar tomonidan hayvon modellarida qarshi turish mumkin J-113,397, BD-1047 yoki (+) - nalokson navbati bilan.[128] Hozirgi vaqtda odamlarda opioid ta'sirida giperaljeziyaga qarshi kurashish uchun biron bir dori-darmon tasdiqlanmagan va og'ir holatlarda yagona echim opioid analjeziklaridan foydalanishni to'xtatish va ularni opioid bo'lmagan analjezik dorilar bilan almashtirishdir. Shu bilan birga, ushbu yon ta'sirning rivojlanishiga individual sezgirlik juda dozaga bog'liq va qaysi opioid analjezik ishlatilishiga qarab farq qilishi mumkinligi sababli, ko'plab bemorlar ushbu ta'sirni oddiygina opioid preparatining dozasini kamaytirish orqali oldini olishlari mumkin (odatda qo'shimcha qo'shilishi bilan birga) opioid bo'lmagan analjezik), turli xil opioid dorilar orasida aylanmoqda yoki aralash ta'sir rejimi bilan yumshoqroq opioidga o'tish orqali, shuningdek, neyropatik og'riqlarga qarshi, xususan tramadol yoki tapentadol.[129][130][131]
- NMDA retseptorlari antagonistlari kabi ketamin
- SNRIlar kabi milnacipran
- Antikonvulsanlar kabi gabapentin yoki pregabalin
Boshqa salbiy ta'sirlar
Jinsiy gormonlarning past darajasi
Klinik tadqiqotlar tibbiy va rekreatsion opioid bilan doimiy ravishda bog'liq gipogonadizm (past jinsiy gormon darajalar) turli jinslarda. Effekt dozaga bog'liq. Ko'pgina tadqiqotlar shuni ko'rsatadiki, surunkali opioidli foydalanuvchilarning aksariyati (ehtimol 90%) gipogonadizmdan aziyat chekmoqda. Opioidlar ham xalaqit berishi mumkin hayz ko'rish ishlab chiqarishni cheklash orqali ayollarda luteinizan gormon (LH). Opioid tomonidan kelib chiqadigan gipogonadizm, ehtimol, opioiddan foydalanish bilan kuchli bog'liqlikni keltirib chiqaradi osteoporoz va suyak sinishi, etishmovchiligi tufayli estradiol. Shuningdek, u og'riqni kuchaytirishi va shu bilan opioidni davolashning mo'ljallangan klinik ta'siriga xalaqit berishi mumkin. Opioid bilan bog'liq gipogonadizm, ehtimol ularning tarkibidagi opioid retseptorlari agonizmi tufayli yuzaga keladi gipotalamus va gipofiz.[iqtibos kerak ] Bir tadqiqot shuni ko'rsatdiki, tushkunlikka tushgan testosteron bir oy ichida geroin giyohvandlik darajasi normal holatga qaytdi, natijada bu ta'sir tezda tiklanishi mumkin va doimiy emas.[iqtibos kerak ] 2013 yildan boshlab[yangilash], past dozali yoki o'tkir opioiddan foydalanishning ta'siri endokrin tizim bu tushunarsiz.[132][133][134][135] Opioidlardan uzoq muddatli foydalanish boshqasiga ta'sir qilishi mumkin gormonal tizimlar shuningdek.[132]
Ishning buzilishi
Opioidlardan foydalanish ish joyiga qaytmaslik xavfi bo'lishi mumkin.[136][137]
Xavfsizlikka oid har qanday vazifani bajaradigan shaxslar opioidlardan foydalanmasliklari kerak.[138] Tibbiy xizmat ko'rsatuvchi xodimlar ishchilarga maslahat bermasliklari kerak haydash yoki foydalanish og'ir uskunalar shu jumladan kranlar yoki forkliftlar surunkali yoki o'tkir og'riqni opioidlar bilan davolash.[138] Xavfsizlikni sezgir operatsiyalarni bajaradigan ishchilarni boshqaradigan ish joylari, shifokorlar tomonidan opioidlar bilan davolangan ekan, ishchilarni unchalik sezgir bo'lmagan ishlarga tayinlashlari kerak.[138]
Opioidlarni uzoq muddat qabul qiladigan odamlar ishsiz bo'lish ehtimolini oshirdilar.[139] Opioidlarni qabul qilish bemorning hayotini yanada buzishi mumkin va opioidlarning o'zlari salbiy ta'sir ko'rsatishi bemorlarning faol hayot kechirishi, ish topishi va martaba bilan ta'minlanishi uchun muhim to'siq bo'lishi mumkin.
Bundan tashqari, ish joyining etishmasligi retsept bo'yicha buyurilgan opioidlardan aberrant foydalanishni bashorat qilishi mumkin.[140]
Voqea sodir bo'lishining kuchayishi
Opioiddan foydalanish ko'payishi mumkin baxtsiz hodisalar. Opioidlar yo'l-transport hodisalari xavfini oshirishi mumkin[141][142] va tasodifiy tushish.[143]
Diqqat kamayadi
Opioidlar diqqatni kamaytirishi isbotlangan, ko'proq antidepressantlar va / yoki antikonvulsanlar bilan ishlatilganda.[144]
Giperaljeziya
Opioid bilan bog'liq giperaljeziya (OIH) surunkali opioid ta'siridan keyin bemorlarda aniq bo'ldi.[145][146]
yon effektlar
Og'riqni kamaytirish uchun opioidlarni qabul qiladigan bemorlarda kamdan-kam uchraydigan nojo'ya reaktsiyalarga quyidagilar kiradi: dozaga bog'liq nafas olish depressiyasi (ayniqsa ko'proq) kuchli opioidlar), chalkashlik, gallyutsinatsiyalar, deliryum, ürtiker, gipotermiya, bradikardiya /taxikardiya, ortostatik gipotenziya, bosh aylanishi, bosh og'rig'i, siydikni ushlab turish, siydik chiqarish yo'llari yoki o't yo'llari spazmi, mushaklarning qattiqlashishi, mioklonus (yuqori dozalarda) va qizarish (fentanil va remifentanildan tashqari gistamin ajralib chiqishi tufayli).[87]Opioidlarni terapevtik va surunkali qo'llash ham funktsiyasini buzishi mumkin immunitet tizimi. Opioidlar ko'payishini pasaytiradi makrofag avlod hujayralari va limfotsitlar va hujayralar differentsiatsiyasiga ta'sir qiladi (Roy va Loh, 1996). Opioidlar ham inhibe qilishi mumkin leykotsit migratsiya. Ammo bu og'riqni kamaytirish sharoitida dolzarbligi ma'lum emas.
O'zaro aloqalar
Opioidlardan foydalangan bemorlarni boshqa dorilar bilan birgalikda davolaydigan shifokorlar doimiy davolanishni ko'rsatadigan hujjatlarni doimiy ravishda saqlab turadilar va agar bemorning ahvoli kamroq xavfli terapiyaga aylansa, davolanishni sozlash imkoniyatlari to'g'risida xabardor.[147]
Boshqa depressant dorilar bilan

Opioidlarni boshqa depressant dorilar bilan bir vaqtda qo'llash benzodiazepinlar yoki etanol noxush hodisalar va dozani oshirib yuborish darajasini oshiradi.[147] Opioidlarni boshqa depressant dorilar, masalan benzodiazepinlar yoki etanol bilan bir vaqtda qo'llash noxush hodisalar va dozani oshirib yuborishini oshiradi. Shunga qaramay, opioidlar va benzodiazepinlar bir vaqtning o'zida ko'plab sharoitlarda tarqatiladi.[148][149] Faqatgina opioidning haddan tashqari dozasida bo'lgani kabi, opioid va boshqa depressantning kombinatsiyasi nafas olish depressiyasini tez-tez o'limga olib kelishi mumkin.[150] Ushbu xatarlar shifokor tomonidan sinchkovlik bilan kuzatilishi bilan kamayadi, ular bemorlarning xulq-atvori va davolanishning muvofiqligi uchun doimiy tekshiruv o'tkazishi mumkin.[147]
Opioid antagonisti
Opioid ta'sirini (salbiy yoki boshqacha), masalan, opioid antagonisti bilan tiklash mumkin nalokson yoki naltrekson.[151] Bular raqobatdosh antagonistlar agonistlarga qaraganda afinitori yuqori bo'lgan opioid retseptorlari bilan bog'lanadi, ammo retseptorlarni faollashtirmaydi. Bu agonistni siqib chiqaradi, agonist ta'sirini susaytiradi yoki qaytaradi. Biroq, yarim umrni yo'q qilish naloksonning o'zi opioidnikiga qaraganda qisqa bo'lishi mumkin, shuning uchun takroriy dozalash yoki doimiy infuziya talab qilinishi mumkin, yoki uzoqroq ta'sir qiluvchi antagonist, masalan. nalmefen ishlatilishi mumkin. Muntazam ravishda opioidlarni qabul qiladigan bemorlarda opioidni qisman orqaga qaytarib, azob chekayotgan og'riqda uyg'onish reaktsiyasini oldini olish kerak. Bunga to'liq dozani bermaslik, ammo nafas olish tezligi yaxshilanmaguncha ozgina dozada berish orqali erishiladi. Keyin og'riqni kamaytirganda, reversivni shu darajada ushlab turish uchun infuziya boshlanadi. Opioid antagonistlari opioid dozasini oshirib yuborganidan keyin nafas olish depressiyasining standart davolash usuli bo'lib qolmoqda, ammo nalokson eng ko'p ishlatiladi, ammo uzoqroq ta'sir qiluvchi antagonist nalmefen metadon kabi uzoq muddatli opioidlarning haddan tashqari dozasini davolashda ishlatilishi mumkin va diprenorfin orqaga qaytish uchun ishlatiladi veterinariya tibbiyotida ishlatiladigan etorfin va karfentanil kabi juda kuchli opioidlarning ta'siri. Shu bilan birga, opioid antagonistlari opioid analjezikalarining foydali ta'sirini blokirovka qilganligi sababli, ular odatda dozani oshirib yuborish uchun foydalidir, yon ta'sirlarni kamaytirish uchun opioid antagonistlari bilan bir qatorda opioid antagonistlaridan foydalanish, dozani ehtiyotkorlik bilan titrlash talab etiladi va ko'pincha etarlicha past dozalarda yomon ta'sir qiladi. og'riq qoldiruvchi vositani saqlashga imkon bering.
Naltrekson jiddiy nojo'ya hodisalar xavfini oshirmaydi, bu og'iz orqali naltreksonning xavfsizligini tasdiqlaydi.[152] Nalokson bilan og'rigan bemorlarda tiklanish toksikligi tufayli o'lim yoki jiddiy nojo'ya hodisalar kamdan-kam uchraydi.[153]
Farmakologiya
| Giyohvand moddalar | Nisbiy Quvvat [154] | Birlashtirilmagan Fraksiya | Oqsil Majburiy | Lipid Eriydiganlik [155][156][157] |
|---|---|---|---|---|
| Morfin | 1 | ++ | ++ | ++ |
| Pethidin (meperidin) | 0.1 | + | +++ | +++ |
| Gidromorfon | 10 | + | +++ | |
| Alfentanil | 10–25 | ++++ | ++++ | +++ |
| Fentanil | 75–125 | + | +++ | ++++ |
| Remifentanil | 250 | +++ | +++ | ++ |
| Sufentanil | 500–1000 | ++ | ++++ | ++++ |
| Etorfin | 1000–3000 | |||
| Karfentanil | 10000 |
Opioidlar o'ziga xos xususiyatga ega opioid retseptorlari ichida asab tizimi va boshqa to'qimalar. Opioid retseptorlarining uchta asosiy klassi mavjud, m, κ, δ (mu, kappa va delta), garchi o'n etti kishiga qadar xabar berilgan bo'lsa ham, ular tarkibiga ph, i, ph va ζ (Epsilon, Iota, Lambda va Zeta) retseptorlari kiradi. Aksincha, σ (Sigma ) retseptorlari endi opioid retseptorlari deb hisoblanmaydi, chunki ularning faollashishi opioid teskari-agonist tomonidan qaytarilmaydi nalokson, ular klassik opioidlar uchun yuqori darajadagi bog'lanishni namoyish etmaydi va ular uchun stereoselektivdir dekstro-rotatsion izomerlar boshqa opioid retseptorlari esa stereo-selektivdir levo-rotator izomerlar. Bundan tashqari, ning uchta kichik turi mavjud m -retseptor: m1 va m2va yangi kashf etilgan m3. Klinik ahamiyatga ega bo'lgan yana bir retseptor - og'riq qoldiruvchi vositalar sifatida ishlatiladigan m-opioid agonistlariga nisbatan bag'rikenglikni rivojlantirishda katta ahamiyatga ega bo'lgan og'riq ta'sirida ishtirok etadigan opioid-retseptorlarga o'xshash retseptorlari 1 (ORL1). Bularning barchasi G-oqsil bilan bog'langan retseptorlar harakat qilish GABAerjik nörotransmisyon.
The farmakodinamik opioidga javob uning bog'langan retseptoriga, uning ushbu retseptorga yaqinligiga va opioidning agonist yoki an antagonist. Masalan, supraspinal opioid agonistning analjezik xususiyatlari morfin m ning faollashishi bilan vositachilik qiladi1 retseptor; nafas olish depressiyasi va jismoniy qaramlik m tomonidan2 retseptor; va retseptorlari tomonidan sedasyon va o'murtqa analjeziya[iqtibos kerak ]. Opioid retseptorlarining har bir guruhi retseptorlari subtiplari (masalan, m kabi) bilan alohida nevrologik reaktsiyalar to'plamini keltirib chiqaradi.1 va m2 Masalan) aniqroq javoblarni taqdim etish. Har bir opioid uchun o'ziga xosligi, uning turli xil opioid retseptorlari sinflariga bog'liqligi ()masalan. m, b va g opioid retseptorlari opioidning o'ziga xos retseptorlari bilan bog'lanishiga qarab har xil kattaliklarda faollashadi). Masalan, afyun alkaloidi morfin m-opioid retseptorlari bilan yuqori darajadagi bog'lanishni namoyish etadi ketazotsin retseptorlari bilan yuqori yaqinlikni namoyish etadi. Aynan shu kombinatorial mexanizm har birining o'ziga xos effekt profiliga ega bo'lgan bunday keng ko'lamli opioidlar va molekulyar konstruktsiyalar mavjud bo'lishiga imkon beradi. Ularning individual molekulyar tuzilishi, shuningdek, ularning turli xil ta'sir qilish muddati uchun javobgardir, shu bilan metabolik parchalanish (masalan N-dealkilatsiya) opioid metabolizmi uchun javobgardir.
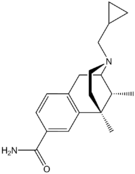
Funktsional selektivlik
Dori vositalarini rivojlantirishning yangi strategiyasi retseptorlarni qabul qiladi signal uzatish hisobga olish. Ushbu strategiya kerakli signalizatsiya yo'llarining faolligini oshirishga harakat qiladi va shu bilan birga kiruvchi yo'llarga ta'sirini kamaytiradi. Ushbu differentsial strategiyaga bir nechta nomlar berilgan, shu jumladan funktsional selektivlik va noaniq agonizm. Qasddan xolis agonist sifatida ishlab chiqilgan va joylashtirilgan birinchi opioid klinik baholash bu dori olitseridin. Bu og'riq qoldiruvchi faollikni va salbiy ta'sirni kamaytiradi.[159]
Opioidni taqqoslash
Opioidlarning nisbiy kuchini taqqoslaydigan ekvivalentlik nisbatlarini aniqlash uchun keng qamrovli tadqiqotlar o'tkazildi. Opioid dozasi berilganida, an ekvanialjezik jadval boshqasining ekvivalent dozasini topish uchun ishlatiladi. Bunday jadvallar opioidni aylantirish amaliyotida qo'llaniladi va opioidni morfin bilan taqqoslash orqali tavsiflash uchun mos yozuvlar opioididir. Equianalgesic jadvallarida odatda preparatning yarim umrlari, ba'zida esa morfin: og'iz orqali va tomir orqali yuborish orqali bir xil preparatning ekvianaljezik dozalari keltirilgan.
Majburiy profillar
Foydalanish
| Modda | Eng yaxshi smeta | Kam smeta | Yuqori smeta |
|---|---|---|---|
| Amfetamin- turdagi stimulyatorlar | 34.16 | 13.42 | 55.24 |
| Nasha | 192.15 | 165.76 | 234.06 |
| Kokain | 18.20 | 13.87 | 22.85 |
| Ekstaz | 20.57 | 8.99 | 32.34 |
| Opiat | 19.38 | 13.80 | 26.15 |
| Opioidlar | 34.26 | 27.01 | 44.54 |
AQShda opioid retseptlari 1991 yildagi 76 milliondan 2013 yilda 207 milliongacha o'sdi.[176]
1990-yillarda opioidni buyurish sezilarli darajada oshdi. Bir vaqtlar deyarli faqat o'tkir og'riq yoki saraton kasalligi sababli og'riqni davolash uchun ishlatilgan, opioidlar endi surunkali og'riqni boshdan kechirayotgan odamlar uchun juda ko'p miqdorda buyuriladi. This has been accompanied by rising rates of accidental addiction and accidental overdoses leading to death. Ga ko'ra Xalqaro Narkotik moddalarni nazorat qilish kengashi, the United States and Canada lead the per capita consumption of prescription opioids.[177] The number of opioid prescriptions per capita in the United States and Canada is double the consumption in the European Union, Australia, and New Zealand.[178] Certain populations have been affected by the opioid addiction crisis more than others, including Birinchi dunyo jamoalar[179] and low-income populations.[180] Public health specialists say that this may result from the unavailability or high cost of alternative methods for addressing chronic pain.[181] Opioids have been described as a cost-effective treatment for chronic pain, but the impact of the opioid epidemic and deaths caused by opioid overdoses should be considered in assessing their cost-effectiveness.[182] Data from 2017 suggest that in the U.S. about 3.4 percent of the U.S. population are prescribed opioids for daily pain management.[183] Call for opioid deprescribing have led to broad scale opioid tapering practices with little scientific evidence to support the safety or benefit for patients with chronic pain.
Tarix
Naturally occurring opioids

Opioids are among the world's oldest known drugs.[184] The earliest known evidence of Papaver somniferum in a human archaeological site dates to the Neolitik period around 5,700–5,500 BC. Its seeds have been found at Cueva de los Murciélagos ichida Iberiya yarim oroli va La Marmotta ichida Italiya yarim oroli.[185][186][187]
Use of the opium poppy for medical, recreational, and religious purposes can be traced to the 4th century BC, when ideograms on Shumerlar clay tablets mention the use of "Hul Gil", a "plant of joy".[188][189][190]Opium was known to the Egyptians, and is mentioned in the Ebers Papirus as an ingredient in a mixture for the soothing of children,[191][190] and for the treatment of breast abscesses.[192]
Opium was also known to the Greeks.[191]It was valued by Gippokrat (c. 460 – c. 370 BC) and his students for its sleep-inducing properties, and used for the treatment of pain.[193] The Latin saying "Sedare dolorem opus divinum est", trans. "Alleviating pain is the work of the divine", has been variously ascribed to Hippocrates and to Pergamning Galeni.[194] The medical use of opium is later discussed by Pedanius Dioscorides (c. 40 – 90 AD), a Greek physician serving in the Roman army, in his five-volume work, De Materia Medica.[195]
Davomida Islomiy Oltin Asr, the use of opium was discussed in detail by Avitsena (c. 980 – June 1037 AD) in Tibbiyot kanoni. The book's five volumes include information on opium's preparation, an array of physical effects, its use to treat a variety of illness, contraindications for its use, its potential danger as a poison and its potential for addiction. Avicenna discouraged opium's use except as a last resort, preferring to address the causes of pain rather than trying to minimize it with og'riq qoldiruvchi vositalar. Many of Avicenna's observations have been supported by modern medical research.[196][191]
Exactly when the world became aware of opium in India and China is uncertain, but opium was mentioned in the Chinese medical work K'ai-pao-pen-tsdo (973 AD)[190] By 1590 AD, opium poppies were a staple spring crop in the Subahlar ning Agra mintaqa.[197]
Shifokor Paracelsus (ca.1493–1541) is often credited with reintroducing opium into medical use in G'arbiy Evropa, davomida Germaniya Uyg'onish davri. He extolled opium's benefits for medical use. He also claimed to have an "arcanum", a pill which he called laudanum, that was superior to all others, particularly when death was to be cheated. ("Ich hab' ein Arcanum – heiss' ich Laudanum, ist über das Alles, wo es zum Tode reichen will.")[198] Later writers have asserted that Paracelsus' recipe for laudanum contained opium, but its composition remains unknown.[198]
Laudanum
The term laudanum was used generically for a useful medicine until the 17th century. Keyin Tomas Sydenham introduced the first liquid tincture of opium, "laudanum" came to mean a mixture of both opium and alcohol.[198]Sydenham's 1669 recipe for laudanum mixed opium with wine, saffron, clove and cinnamon.[199] Sydenham's laudanum was used widely in both Europe and the Americas until the 20th century.[191][199]Other popular medicines, based on opium, included Paregorik, a much milder liquid preparation for children; Black-drop, a stronger preparation; va Dover kukuni.[199]
The opium trade
Opium became a major colonial commodity, moving legally and illegally through trade networks involving Hindiston, Portugal, Golland, Inglizlar va Xitoy, Boshqalar orasida.[200]Inglizlar East India kompaniyasi saw the opium trade as an investment opportunity in 1683 AD.[197] In 1773 the Governor of Bengal established a monopoly on the production of Bengal opium, on behalf of the East India Company. The cultivation and manufacture of Indian opium was further centralized and controlled through a series of acts, between 1797 and 1949.[197][201] The British balanced an economic deficit from the importation of Xitoy choyi by selling Indian opium which was smuggled into China in defiance of Xitoy hukumati bans. Bu sabab bo'ldi Birinchidan (1839-1842) va Ikkinchi afyun urushlari (1856–1860) between China and Britain.[202][201][200][203]
Morfin
In the 19th century, two major scientific advances were made that had far-reaching effects. Around 1804, German pharmacist Fridrix Sertyurner izolyatsiya qilingan morfin from opium. He described its crystallization, structure, and pharmacological properties in a well-received paper in 1817.[202][204][199][205]Morphine was the first alkaloid to be isolated from any medicinal plant, the beginning of modern scientific drug discovery.[202][206]
The second advance, nearly fifty years later, was the refinement of the hipodermik igna tomonidan Aleksandr Vud va boshqalar. Development of a glass syringe with a subcutaneous needle made it possible to easily administer controlled measurable doses of a primary active compound.[207][199][190][208][209]
Morphine was initially hailed as a wonder drug for its ability to ease pain.[210] It could help people sleep,[202] and had other useful side effects, including control of yo'tal va diareya.[211] It was widely prescribed by doctors, and dispensed without restriction by pharmacists. Davomida Amerika fuqarolar urushi, opium and laudanum were used extensively to treat soldiers.[212][210] It was also prescribed frequently for women, for hayz paytida og'riq and diseases of a "nervous character".[213]:85At first it was assumed (wrongly) that this new method of application would not be addictive.[202][213]
Kodein
Kodein was discovered in 1832 by Per Jan Robiquet. Robiquet was reviewing a method for morphine extraction, described by Scottish chemist Uilyam Gregori (1803–1858). Processing the residue left from Gregory's procedure, Robiquet isolated a crystalline substance from the other active components of opium. He wrote of his discovery: "Here is a new substance found in opium ... We know that morphine, which so far has been thought to be the only active principle of opium, does not account for all the effects and for a long time the physiologists are claiming that there is a gap that has to be filled."[214] His discovery of the alkaloid led to the development of a generation of antitussive and antidiarrheal medicines based on codeine.[215]
Semisynthetic and synthetic opioids
Synthetic opioids were invented, and biological mechanisms for their actions discovered, in the 20th century.[190] Scientists have searched for non-addictive forms of opioids, but have created stronger ones instead. Angliyada Charlz Romli Alder Rayt developed hundreds of opiate compounds in his search for a nonaddictive opium derivative. In 1874 he became the first person to synthesize diamorfin (heroin), using a process called atsetilatsiya which involved boiling morphine with sirka angidrid bir necha soat davomida.[202]
Heroin received little attention until it was independently synthesized by Feliks Xofmann (1868–1946), working for Geynrix Drezer (1860–1924) at Bayer Laboratoriyalar.[216] Dreser brought the new drug to market as an og'riq qoldiruvchi and a cough treatment for sil kasalligi, bronxit va Astma in 1898. Bayer ceased production in 1913, after heroin's addictive potential was recognized.[202][217][218]
Several semi-synthetic opioids were developed in Germany in the 1910s. Birinchi, oksimorfon, was synthesized from thebaine, an opioid alkaloid in opium poppies, in 1914.[219]Next, Martin Freund and Edmund Speyer developed oksikodon, also from thebaine, at the University of Frankfurt in 1916.[220]1920 yilda, gidrokodon tomonidan tayyorlangan Karl Mannich va Helene Löwenheim, deriving it from codeine. 1924 yilda, gidromorfon was synthesized by adding hydrogen to morphine. Etorfin was synthesized in 1960, from the oripavin in opium poppy straw. Buprenorfin was discovered in 1972.[219]
The first fully synthetic opioid was meperidin (later demerol), found serendipitously by German chemist Otto Eisleb (or Eislib) at IG Farben 1932 yilda.[219] Meperidine was the first opiate to have a structure unrelated to morphine, but with opiate-like properties.[190] Its analgesis effects were discovered by Otto Schaumann in 1939.[219]Gustav Ehrxart va Maks Bokmuhl, also at IG Farben,built on the work of Eisleb and Schaumann. They developed "Hoechst 10820" (later metadon ) around 1937.[221]In 1959 the Belgian physician Pol Yanssen ishlab chiqilgan fentanil, a synthetic drug with 30 to 50 times the potency of heroin.[202][222]Nearly 150 synthetic opioids are now known.[219]
Criminalization and medical use
Non-clinical use of opium was criminalized in the United States by the Xarrison giyohvand moddalar to'g'risidagi soliq to'g'risidagi qonun of 1914, and by many other laws.[223][224] The use of opioids was stigmatized, and it was seen as a dangerous substance, to be prescribed only as a last resort for dying patients.[202] The Boshqariladigan moddalar to'g'risidagi qonun of 1970 eventually relaxed the harshness of the Harrison Act.[iqtibos kerak ]
In the United Kingdom the 1926 report of the Departmental Committee on Morfin and Heroin Giyohvandlik under the Chairmanship of the President of the Royal College of Physicians reasserted medical control and established the "British system" of control—which lasted until the 1960s.[225]
In the 1980s the World Health Organization published guidelines for prescribing drugs, including opioids, for different levels of pain. In the U.S., Kathleen Foley and Russell Portenoy became leading advocates for the liberal use of opioids as painkillers for cases of "intractable non-malignant pain".[226][227]With little or no scientific evidence to support their claims, industry scientists and advocates suggested that chronic pain sufferers would be resistant to addiction.[202][228][226]
Ning chiqarilishi OxyContin in 1996 was accompanied by an aggressive marketing campaign promoting the use of opioids for pain relief. Increasing prescription of opioids fueled a growing black market for heroin. Between 2000 and 2014 there was an "alarming increase in heroin use across the country and an epidemic of drug overdose deaths".[228][202][229]
As a result, health care organizations and public health groups, such as Physicians for Responsible Opioid Prescribing, have called for decreases in the prescription of opioids.[228] In 2016, the Centers for Disease Control and Prevention (CDC) issued a new set of guidelines for the prescription of opioids "for chronic pain outside of active cancer treatment, palliative care, and end-of-life care" and the increase of opioid tapering.[230]
"Remove the Risk"
In April 2019 the U.S. Oziq-ovqat va dori-darmonlarni boshqarish announced the launch of a new education campaign to help Americans understand the important role they play in removing and properly disposing of unused prescription opioids from their homes. This new initiative is part of the FDA's continued efforts to address the nationwide opioid inqirozi (see below) and aims to help decrease unnecessary exposure to opioids and prevent new addiction. The “Remove the Risk” campaign is targeting women ages 35–64, who are most likely to oversee household health care decisions and often serve as the gatekeepers to opioids and other prescription medications in the home.[231]
Jamiyat va madaniyat
Ta'rif
The term "opioid" originated in the 1950s.[232] It combines "opium" + "-oid" meaning "opiate-like" ("opiates" being morphine and similar drugs derived from afyun ). The first scientific publication to use it, in 1963, included a footnote stating, "In this paper, the term, 'opioid', is used in the sense originally proposed by George H. Acheson (personal communication) to refer to any chemical compound with morphine-like activities".[233] By the late 1960s, research found that opiate effects are mediated by activation of specific molecular receptors in the nervous system, which were termed "opioid receptors".[234] The definition of "opioid" was later refined to refer to substances that have morphine-like activities that are mediated by the activation of opioid receptors. One modern pharmacology textbook states: "the term opioid applies to all agonists and antagonists with morphine-like activity, and also the naturally occurring and synthetic opioid peptides".[235] Another pharmacology reference eliminates the morphine-like requirement: "Opioid, a more modern term, is used to designate all substances, both natural and synthetic, that bind to opioid receptors (including antagonists)".[2] Some sources define the term opioid chiqarib tashlamoq afyun, and others use afyun comprehensively instead of opioid, lekin opioid used inclusively is considered modern, preferred and is in wide use.[18]
Efforts to reduce abuse in the US
In 2011, the Obama administration released a white paper describing the administration's plan to deal with the opioid inqirozi. The administration's concerns about addiction and accidental overdosing have been echoed by numerous other medical and government advisory groups around the world.[181][236][237][238]
As of 2015, prescription drug monitoring programs exist in every state, except for Missouri.[239] These programs allow pharmacists and prescribers to access patients' prescription histories in order to identify suspicious use. However, a survey of US physicians published in 2015 found that only 53% of doctors used these programs, while 22% were not aware that the programs were available to them.[240] The Kasalliklarni nazorat qilish va oldini olish markazlari was tasked with establishing and publishing a new guideline, and was heavily lobbied.[241] In 2016, the United States Kasalliklarni nazorat qilish va oldini olish markazlari published its Guideline for Prescribing Opioids for Chronic Pain, recommending that opioids only be used when benefits for pain and function are expected to outweigh risks, and then used at the lowest effective dosage, with avoidance of concurrent opioid and benzodiazepine use whenever possible.[32] Research suggests that the prescription of high doses of opioids related to chronic opioid therapy (COT) can at times be prevented through state legislative guidelines and efforts by health plans that devote resources and establish shared expectations for reducing higher doses.[242]
On 10 August 2017, Donald Tramp declared the opioid crisis a (non-FEMA) national public health emergency.[243]
Global shortages
Morfin and other poppy-based medicines have been identified by the World Health Organization as essential in the treatment of severe pain. As of 2002, seven countries (USA, UK, Italy, Australia, France, Spain and Japan) use 77% of the world's morfin supplies, leaving many emerging countries lacking in pain relief medication.[244] The current system of supply of raw poppy materials to make poppy-based medicines is regulated by the Xalqaro Narkotik moddalarni nazorat qilish kengashi under the provision of the 1961 Giyohvand moddalarga qarshi yagona konventsiya. The amount of raw poppy materials that each country can demand annually based on these provisions must correspond to an estimate of the country's needs taken from the national consumption within the preceding two years. In many countries, underprescription of morphine is rampant because of the high prices and the lack of training in the prescription of poppy-based drugs. The Jahon Sog'liqni saqlash tashkiloti is now working with administrations from various countries to train healthworkers and to develop national regulations regarding drug prescription to facilitate a greater prescription of poppy-based medicines.[245]
Another idea to increase morphine availability is proposed by the Senlis Kengashi, who suggest, through their proposal for Afghan Morphine, bu Afg'oniston could provide cheap pain relief solutions to emerging countries as part of a second-tier system of supply that would complement the current INCB regulated system by maintaining the balance and closed system that it establishes while providing finished product morphine to those suffering from severe pain and unable to access poppy-based drugs under the current system.
Dam olish uchun foydalanish
Opioids can produce strong feelings of eyforiya[246] and are frequently used recreationally. Traditionally associated with illicit opioids such as heroin, prescription opioids are misused recreationally.
Giyohvand moddalarni suiiste'mol qilish and non-medical use include the use of drugs for reasons or at doses other than prescribed. Opioid misuse can also include providing medications to persons for whom it was not prescribed. Such diversion may be treated as crimes, punishable by imprisonment in many countries.[247][248] In 2014, almost 2 million Americans abused or were dependent on prescription opioids.[249]
Tasnifi
Ushbu bo'lim uchun qo'shimcha iqtiboslar kerak tekshirish. (2011 yil avgust) (Ushbu shablon xabarini qanday va qachon olib tashlashni bilib oling) |
There are a number of broad classes of opioids:[iqtibos kerak ]
- Tabiiy afyun: alkaloidlar contained in the resin of the ko'knori, birinchi navbatda morfin, kodein va thebaine, lekin emas papaverin va noskapin which have a different mechanism of action; The following could be considered natural opiates: The leaves from Mitragyna speciosa (shuningdek, nomi bilan tanilgan kratom ) contain a few naturally-occurring opioids, active via Mu- and Delta receptors. Salvinorin A, found naturally in the Salvia divinorum plant, is a kappa-opioid receptor agonist.[250]
- Esters of morphine opiates: slightly chemically altered but more natural than the semi-synthetics, as most are morphine prodrugs, diatsetilmorfin (morphine diacetate; heroin), nikomorfin (morphine dinicotinate), dipropanoylmorphine (morphine dipropionate), desomorfin, atsetilpropionilmorfin, dibenzoylmorfin, diacetyldihydromorphine;[251][252]
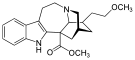
- Semi-synthetic opioids: created from either the natural opiates or morphine esters, such as gidromorfon, gidrokodon, oksikodon, oksimorfon, ethylmorphine va buprenorfin;
- Fully synthetic opioids: kabi fentanil, petsidin, levorfanol, metadon, tramadol, tapentadol va dekstropropoksifen;
- Endogen opioid peptidlar, produced naturally in the body, such as endorfinlar, enkefalinlar, dinorfinlar va endomorphins. Morphine, and some other opioids, which are produced in small amounts in the body, are included in this category.
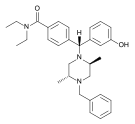
Tramadol va tapentadol, which act as monoamine uptake inhibitors also act as mild and potent agonistlar (respectively) of the m-opioid retseptorlari.[253] Both drugs produce og'riqsizlantirish even when nalokson, an opioid antagonist, is administered.[254]
Some minor opium alkaloidlar and various substances with opioid action are also found elsewhere, including molecules present in kratom, Korydalis va Salvia divinorum plants and some species of poppy aside from Papaver somniferum. There are also strains which produce copious amounts of thebaine, an important raw material for making many semi-synthetic and synthetic opioids. Of all of the more than 120 poppy species, only two produce morphine.
Amongst analgesics there are a small number of agents which act on the central nervous system but not on the opioid receptor system and therefore have none of the other (narcotic) qualities of opioids although they may produce euphoria by relieving pain—a euphoria that, because of the way it is produced, does not form the basis of habituation, physical dependence, or addiction. Foremost amongst these are nefopam, orfenadrin va ehtimol feniltoloksamin yoki boshqasi antigistaminlar. Trisiklik antidepressantlar have painkilling effect as well, but they're thought to do so by indirectly activating the endogenous opioid system. Paracetamol is predominantly a centrally acting analgesic (non-narcotic) which mediates its effect by action on descending serotoninergic (5-hydroxy triptaminergic) pathways, to increase 5-HT release (which inhibits release of pain mediators). It also decreases cyclo-oxygenase activity. It has recently been discovered that most or all of the therapeutic efficacy of paracetamol is due to a metabolite, AM404, which enhances the release of serotonin and inhibits the uptake of anandamid.[iqtibos kerak ]
Other analgesics work peripherally (ya'ni, not on the brain or spinal cord). Research is starting to show that morphine and related drugs may indeed have peripheral effects as well, such as morphine gel working on burns. Recent investigations discovered opioid receptors on peripheral sensory neurons.[255] A significant fraction (up to 60%) of opioid analgesia can be mediated by such peripheral opioid receptors, particularly in inflammatory conditions such as arthritis, traumatic or surgical pain.[256] Inflammatory pain is also blunted by endogenous opioid peptides activating peripheral opioid receptors.[257]
It was discovered in 1953,[iqtibos kerak ] that humans and some animals naturally produce minute amounts of morphine, codeine, and possibly some of their simpler derivatives like heroin and dihidromorfin, in addition to endogenous opioid peptides. Some bacteria are capable of producing some semi-synthetic opioids such as gidromorfon va gidrokodon when living in a solution containing morphine or codeine respectively.
Ko'pchilik alkaloidlar and other derivatives of the opium poppy are not opioids or narcotics; the best example is the smooth-muscle relaxant papaverin. Noscapine is a marginal case as it does have CNS effects but not necessarily similar to morphine, and it is probably in a category all its own.
Dekstrometorfan (the stereoisomer of levometorfan, a semi-synthetic opioid agonist) and its metabolite dekstrorfan have no opioid analgesic effect at all despite their structural similarity to other opioids; instead they are potent NMDA antagonistlari va sigma 1 and 2 -receptor agonists and are used in many retseptsiz sotiladigan cough suppressants.
Salvinorin A is a unique selective, powerful ĸ-opioid receptor agonist. It is not properly considered an opioid nevertheless, because:
- chemically, it is not an alkaloid; va
- it has no typical opioid properties: absolutely no anxiolytic or cough-suppressant effects. It is instead a powerful gallyutsinogen.
| Opioid peptidlar | Skeletal molecular images |
|---|---|
| Adrenorfin |  |
| Amidorfin |  |
| Kasomorfin | |
| DADLE | |
| DAMGO |  |
| Dermorfin | |
| Endomorfin |  |
| Morfitseptin |  |
| Nosiseptin |  |
| Oktreotid |  |
| Opiorphin | 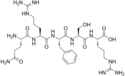 |
| TRIMU 5 |  |
Endogen opioidlar
Opioid-peptidlar that are produced in the body include:
b-endorfin bilan ifodalanadi Pro-opiomelanokortin (POMC) cells in the boshq yadrosi, ichida miya sopi and in immune cells, and acts through m-opioid retseptorlari. β-endorphin has many effects, including on jinsiy xatti-harakatlar va ishtaha. β-endorphin is also secreted into the circulation from pituitary kortikotroplar va melanotropes. a-neo-endorfin is also expressed in POMC cells in the arcuate nucleus.
met-enkefalin is widely distributed in the CNS and in immune cells; [met]-enkephalin is a product of the proenkephalin gene, and acts through μ and b-opioid retseptorlari. leu-enkephalin, also a product of the proenkephalin gene, acts through δ-opioid receptors.
Dinorfin acts through κ-opioid receptors, and is widely distributed in the CNS, including in the orqa miya va gipotalamus, including in particular the boshq yadrosi and in both oksitotsin va vazopressin neyronlari supraoptik yadro.
Endomorfin acts through μ-opioid receptors, and is more potent than other endogenous opioids at these receptors.
Opium alkaloids and derivatives
Afyun alkaloidlari
Fenantrenlar naturally occurring in (afyun ):
Preparations of mixed opium alkaloidlar, shu jumladan papaveretum, are still occasionally used.
Esters of morphine
- Diatsetilmorfin (morphine diacetate; heroin)
- Nikomorfin (morphine dinicotinate)
- Dipropanoylmorfin (morphine dipropionate)
- Diatsetildihidromorfin
- Asetilpropionilmorfin
- Desomorfin
- Metildesorfin
- Dibenzoylmorfin
Ethers of morphine
Semi-synthetic alkaloid derivatives
- Buprenorfin
- Etorfin
- Gidrokodon
- Gidromorfon
- Oksikodon (sold as OxyContin)
- Oksimorfon
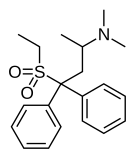
Sintetik opioidlar
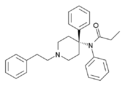
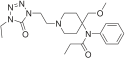
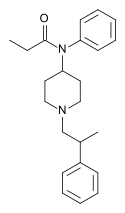
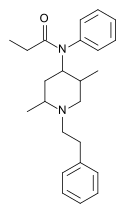
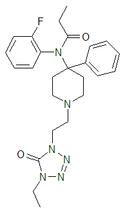
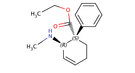
Anilidopiperidinlar
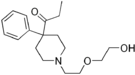
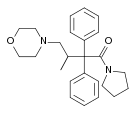
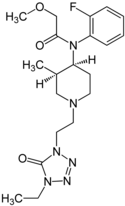
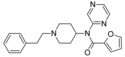
Phenylpiperidines
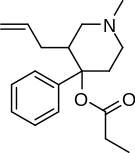
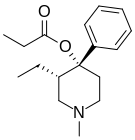
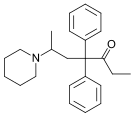
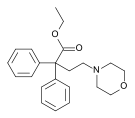
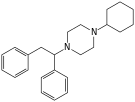
Diphenylpropylamine derivatives
- Propoksifen
- Dekstropropoksifen
- Dekstromoramid
- Bezitramid
- Piritramid
- Metadon
- Dipipanon
- Levomethadyl Acetate (LAAM)
- Difenoksin
- Difenoksilat
- Loperamid (does cross the blood-brain barrier but is quickly pumped into the non-central nervous system by P-Glycoprotein. Mild opiate withdrawal in animal models exhibits this action after sustained and prolonged use including rhesus monkeys, mice, and rats.)
Benzomorphan derivatives
- Dezosin —agonist/antagonist
- Pentazotsin —agonist/antagonist
- Fenazotsin
Oripavin hosilalari
- Buprenorfin —partial agonist
- Dihidroetorfin
- Etorfin
Morphinan derivatives
- Butorfanol —agonist/antagonist
- Nalbufin —agonist/antagonist
- Levorfanol
- Levometorfan
- Racemethorphan
Boshqalar
Allosterik modulyatorlar
Oddiy allosterik modulyatorlar do not belong to the opioids, instead they are classified as opioidergiya.
Opioid antagonistlari
- Nalmefen
- Nalokson
- Naltrekson
- Metilnaltrekson (Methylnaltrexone is only peripherally active as it does not cross the blood-brain barrier in sufficient quantities to be centrally active. As such, it can be considered the antithesis of loperamid.)
- Naloksegol (Naloxegol is only peripherally active as it does not cross the blood-brain barrier in sufficient quantities to be centrally active. As such, it can be considered the antitheses of loperamid.)
Tables of opioids
Table of morphinan opioids
| Table of morphinan opioids: click to | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table of non-morphinan opioids
| Table of non-morphinan opioids: click to | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Shuningdek qarang
Adabiyotlar
- ^ Ogura T, Egan TD (2013). "15-bob - opioid agonistlar va antagonistlar". Anesteziya uchun farmakologiya va fiziologiya: asoslari va klinik qo'llanilishi. Filadelfiya, Pensilvaniya: Elsevier / Sonders. ISBN 978-1-4377-1679-5.
- ^ a b Hemmings HC, Egan TD (2013). Anesteziya uchun farmakologiya va fiziologiya: asoslari va klinik qo'llanilishi: Expert Consult - Onlayn va chop etish. Elsevier sog'liqni saqlash fanlari. p. 253. ISBN 978-1437716795.
Opiat farmakologiyada klassik ravishda afyundan olingan dori degan ma'noni anglatadi. Opioid, zamonaviyroq atama, opioid retseptorlari (antagonistlarni ham o'z ichiga olgan) bilan bog'laydigan tabiiy va sintetik barcha moddalarni belgilash uchun ishlatiladi.
- ^ a b Stromgaard K, Krogsgaard-Larsen P, Madsen U (2009). Dori-darmonlarni loyihalash va kashf qilish bo'yicha darslik, to'rtinchi nashr. CRC Press. ISBN 9781439882405.
- ^ Walzer C (2014). "52 Nondomestic Equities". G'arbiy G, Xerd D, Kalkett N (tahrir). Hayvonot bog'i hayvonlar va yovvoyi tabiatni immobilizatsiya qilish va behushlik. Kanada veterinariya jurnali. 51 (2-nashr). Ames, AQSh: Jon Uili va Sons. 723, 727 betlar. doi:10.1002/9781118792919. ISBN 9781118792919. PMC 2871358. Olingan 8 iyul 2019.
- ^ "Karfentanil". www.drugbank.ca. Olingan 8 iyul 2019.
- ^ Sterken J, Troubleyn J, Gasthuys F, Maes V, Diltoer M, Verborgh C (oktyabr 2004). "Katta hayvonlarning immobilonini ataylab dozasini oshirib yuborish". Evropa shoshilinch tibbiy yordam jurnali. 11 (5): 298–301. doi:10.1097/00063110-200410000-00013. PMID 15359207.
- ^ Lembke A (2016). Giyohvand moddalar sotuvchisi, tibbiyot fanlari doktori: Shifokorlarni qanday aldashdi, bemorlarni ilmoqqa tortishdi va nega to'xtatish juda qiyin. Jons Xopkins universiteti matbuoti. ISBN 978-1421421407.
- ^ "Giyohvand moddalar: retsept bo'yicha opioidlar". NIDA. Iyun 2019. Arxivlandi asl nusxasidan 2019 yil 12 iyunda. Olingan 5 iyul 2019.
- ^ "FDA opioid analgetiklari, retsept bo'yicha buyurilgan opioid yo'tal mahsulotlari va benzodiazepin yorlig'i bilan birgalikda jiddiy xatarlar va birgalikda foydalanish natijasida o'lim bilan bog'liq kuchli ogohlantirishlarni talab qiladi". FDA. 2016 yil 31-avgust. Olingan 1 sentyabr 2016.
- ^ Parthvi R, Agrawal A, Khanijo S, Tsegaye A, Talwar A (2019 yil may-iyun). "O'tkir dozada dozani oshirib yuborish: shoshilinch tibbiy yordam bo'limida va juda muhim tibbiy yordam bo'limida boshqaruv strategiyalari to'g'risida yangilanish". Amerika terapiya jurnali. 26 (3): e380-e387. doi:10.1097 / MJT.0000000000000681. PMID 28952972. S2CID 24720660.
- ^ "Noqonuniylikning holati va trend tahlili [sic] Giyohvand moddalar bozori " (PDF). Giyohvand moddalar bo'yicha jahon hisoboti 2015 yil. Olingan 26 iyun 2015.
- ^ "Hisobot III: Opiatga bog'liqlikni davolash uchun FDA tomonidan tasdiqlangan dorilar: samaradorlik va iqtisodiy samaradorlik bo'yicha adabiyotlar sharhlari, davolash ilmiy-tadqiqot instituti". Giyohvandlikka qarshi dori-darmonlardan foydalanishni rivojlantirish: Opioidga qaramlikni davolash uchun ta'siri. p. 41.
- ^ Tetrault JM, Butner JL (sentyabr 2015). "Opioidning tibbiy bo'lmagan retsepti va retsepti bo'yicha opioiddan foydalanish buzilishi: sharh". Yale Biology and Medicine jurnali. 88 (3): 227–33. PMC 4553642. PMID 26339205.
- ^ Tarabar AF, Nelson LS (2003 yil aprel). "Qo'shma Shtatlarda bolalar tomonidan geroinning qayta tiklanishi va suiiste'mol qilinishi". Pediatriyadagi dolzarb fikrlar. 15 (2): 210–5. doi:10.1097/00008480-200304000-00013. PMID 12640281. S2CID 21900231.
- ^ Grey E (2014 yil 4-fevral). "AQShda arzon dozalar toshqini tufayli geroin mashhurlikka erishmoqda".. TIME.com. Olingan 12 fevral 2016.
- ^ Maltoni M (2008 yil yanvar). "Opioidlar, og'riq va qo'rquv". Onkologiya yilnomalari. 19 (1): 5–7. doi:10.1093 / annonc / mdm555. PMID 18073220.
[A] qator tadqiqotlar, shuningdek, bemorlarning 40-70 foizida og'riqni nazorat qilishning etarli emasligi haqida xabar berishdi, natijada epidemiyaning yangi turi paydo bo'ldi, bu "muvaffaqiyatsiz og'riqni nazorat qilish" ning oldini olishda bir qator to'siqlar tufayli yuzaga keldi. saraton kasalligini etarli darajada boshqarish .... Saraton kasalligi opioidlarni suiiste'mol qilish va giyohvandlikka qarshi olib borilgan urushning begunoh qurboniga aylanish xavfini tug'diradi, agar ikki xil foydalanish (terapevtik yoki terapevtik) normalari aniq ajratilmagan bo'lsa. Bundan tashqari, sog'liqni saqlash sohasi mutaxassislari me'yoriy tekshiruvdan xavotirda bo'lishlari mumkin va shu sababli opioid terapiyasini ishlatmasliklari mumkin.
- ^ McCarberg BH (mart 2011). "Birlamchi tibbiy yordamda og'riqni boshqarish: opioidni suiiste'mol qilish, suiiste'mol qilish va chalg'itishni kamaytirish strategiyasi". Aspiranturadan keyingi tibbiyot. 123 (2): 119–30. doi:10.3810 / pgm.2011.03.2270. PMID 21474900. S2CID 25935364.
- ^ a b v Offermanns S (2008). Molekulyar farmakologiya entsiklopediyasi. 1 (2 nashr). Springer Science & Business Media. p. 903. ISBN 9783540389163.
Qattiq ma'noda afyun afyundan olinadigan dorilar bo'lib, ular tarkibiga tabiiy mahsulotlar morfin, kodein, tebain va ulardan olingan ko'plab yarim sintetik kongenerlar kiradi. Keng ma'noda afyunlar peptid bo'lmagan tuzilishga ega morfinga o'xshash dorilar. Eski opiyatlar endilikda opioidlar retseptorlari ta'sirida morfinga o'xshash effekt hosil qiluvchi har qanday moddaga (endogen yoki sintetik, peptid yoki peptid bo'lmagan) tegishli bo'lgan opioidlar atamasi bilan tobora ko'proq almashtirilmoqda.
- ^ Freye E (2008). "II qism. Opioidlarning ta'sir mexanizmi va klinik ta'sirlari". Tibbiyotdagi opioidlar: Har xil klinik og'riqli holatlarda ta'sir qilish tartibi va analjeziklardan foydalanish bo'yicha keng qamrovli tadqiq.. Springer Science & Business Media. p. 85. ISBN 9781402059476.
Opiat - bu ko'knori sharbatidan olingan giyohvand moddalarni (tabiiy va yarim sintetik) tavsiflash uchun ishlatiladigan o'ziga xos atama. Masalan, morfin afyun, ammo metadon (umuman sintetik dori) emas. Opioid - bu o'z ta'sirini opioid retseptorlari bilan biriktirish natijasida hosil bo'lgan va nalakson bilan raqobatdosh ravishda antagonist bo'lgan tabiiy, yarim sintetik va sintetik dorilarni o'z ichiga olgan umumiy atama. Shu nuqtai nazardan opioid atamasi opioid agonistlari, opioid antagonistlari, opioid peptidlari va opioid retseptorlarini anglatadi.
- ^ Devies PS, D'Arcy YM (26 sentyabr 2012). Saraton kasalligini davolash bo'yicha ixcham klinik qo'llanma: hamshiralar uchun dalillarga asoslangan yondashuv. Springer nashriyot kompaniyasi. ISBN 9780826109743.
- ^ "21 AQSh kodeksi § 802 - ta'riflar". LII / Huquqiy axborot instituti. Olingan 12 fevral 2016.
- ^ "NARCOTIC ta'rifi". www.merriam-webster.com. Olingan 12 fevral 2016.
- ^ Satoskar RS, Rege N, Bhandarkar SD (2015). Farmakologiya va farmakoterapiya. Elsevier sog'liqni saqlash fanlari. ISBN 9788131243718.
- ^ Ebert MH, Kerns RD (2010). Xulq-atvor va psixofarmakologik og'riqni boshqarish. Kembrij universiteti matbuoti. ISBN 9781139493543.
- ^ Mur RA, Wiffen PJ, Derry S, Maguire T, Roy YM, Tyrrell L (2015 yil noyabr). "O'tkir og'riqlar uchun retseptsiz (OTC) og'iz orqali analjeziklar - Cochrane sharhlariga umumiy nuqtai". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 11 (11): CD010794. doi:10.1002 / 14651858.CD010794.pub2. PMC 6485506. PMID 26544675.
- ^ a b Fleisher GR, Lyudvig S (2010). Pediatriyada shoshilinch tibbiy yordam darsligi. Lippincott Uilyams va Uilkins. p. 61. ISBN 9781605471594.
- ^ Aleksandr GC, Kruszewski SP, Vebster DW (2012 yil noyabr). "Bemorlarning xavfsizligi va sog'lig'ini himoya qilish uchun opioid retseptini qayta ko'rib chiqish". JAMA. 308 (18): 1865–6. doi:10.1001 / jama.2012.14282. PMID 23150006.
- ^ Mohamadi A, Chan JJ, Lian J, Rayt CL, Marin AM, Rodriguez EK va boshq. (2018 yil avgust). "Travma yoki jarrohlikdan so'ng xavf omillari va uzoq muddatli opioidni iste'mol qilish darajasi: tizimli tahlil va meta- (regressiya) tahlil". Suyak va qo'shma jarrohlik jurnali. Amerika jildi. 100 (15): 1332–1340. doi:10.2106 / JBJS.17.01239. PMID 30063596. S2CID 51891341.
- ^ Devis, Kori S.; Liberman, Emi Judd; Ernandes-Delgado, Ektor; Suba, Karli (2019 yil 1-yanvar). "Qo'shma Shtatlarda o'tkir og'riqlar uchun opioidlarni tayinlashni yoki tarqatishni cheklaydigan qonunlar: milliy tizimli huquqiy tekshiruv". Giyohvandlik va alkogolga qaramlik. 194: 166–172. doi:10.1016 / j.drugalcdep.2018.09.022. ISSN 1879-0046. PMID 30445274.
- ^ Franklin GM (sentyabr 2014). "Surunkali saraton bo'lmagan og'riq uchun opioidlar: Amerika Nevrologiya Akademiyasining pozitsiyasi". Nevrologiya. 83 (14): 1277–84. doi:10.1212 / WNL.0000000000000839. PMID 25267983.
- ^ a b Okie S (2010 yil noyabr). "Opioid toshqini, o'lim oqimining ko'tarilishi". Nyu-England tibbiyot jurnali. 363 (21): 1981–5. doi:10.1056 / NEJMp1011512. PMID 21083382. S2CID 7092234.
Okie istiqbollariga javoblar: Rich JD, Green TC, McKenzie MS (fevral 2011). "Opioidlar va o'lim". Nyu-England tibbiyot jurnali. 364 (7): 686–687. doi:10.1056 / NEJMc1014490. PMID 21323559. - ^ a b Dowell D, Haegerich TM, Chou R (2016 yil aprel). "Surunkali og'riqlarga qarshi opioidlarni buyurish bo'yicha CDC qo'llanmasi - Amerika Qo'shma Shtatlari, 2016 yil". JAMA. 315 (15): 1624–45. doi:10.1001 / jama.2016.1464. PMC 6390846. PMID 26977696.
- ^ McNicol E, Strassels SA, Goudas L, Lau J, Carr DB (yanvar 2005). McNicol ED (tahrir). "NSAID yoki paratsetamol, yakka o'zi yoki opioidlar bilan birgalikda, saraton kasalligi uchun". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (1): CD005180. doi:10.1002 / 14651858.CD005180. PMID 15654708. (Orqaga tortildi, qarang doi:10.1002 / 14651858.cd005180.pub2. Agar bu tortib olingan qog'ozga qasddan keltirilgan bo'lsa, uni o'zgartiring
{{Orqaga olindi}}bilan{{Orqaga olindi| qasddan = ha}}.) - ^ a b Migrenni davolash uchun opioidlardan foydalanish va haddan tashqari foydalanish haqida ma'lumot uchun qarang Amerika Nevrologiya Akademiyasi (2013 yil fevral), "Shifokorlar va bemorlar so'rashlari kerak bo'lgan beshta narsa", Aql bilan tanlash: ning tashabbusi ABIM Foundation, Amerika Nevrologiya Akademiyasi, olingan 1 avgust 2013, qaysi havola
- Silberstein SD (2000 yil sentyabr). "Amaliyot parametri: O'chokli bosh og'rig'i uchun dalillarga asoslangan ko'rsatmalar (dalillarga asoslangan tahlil): Amerika Nevrologiya Akademiyasining Sifat standartlari kichik qo'mitasining hisoboti". Nevrologiya. 55 (6): 754–62. doi:10.1212 / WNL.55.6.754. PMID 10993991.
- Evers S, Afra J, Fres A, Goadsby PJ, Linde M, May A, Sandor PS (sentyabr 2009). "O'chokli dori-darmonlarni davolash bo'yicha EFNS yo'riqnomasi - EFNS ishchi guruhining qayta ko'rib chiqilgan hisoboti". Evropa nevrologiya jurnali. 16 (9): 968–81. doi:10.1111 / j.1468-1331.2009.02748.x. PMID 19708964.
- Klinik tizimlarni takomillashtirish instituti (2011), Bosh og'rig'i, diagnostikasi va davolash, Klinik tizimlarni takomillashtirish instituti, dan arxivlangan asl nusxasi 2013 yil 29 oktyabrda, olingan 18 dekabr 2013
- ^ Rassom JT, Crofford LJ (2013 yil mart). "Fibromiyalgiya sindromida surunkali opioiddan foydalanish: klinik tadqiq". Klinik revmatologiya jurnali. 19 (2): 72–7. doi:10.1097 / RHU.0b013e3182863447. PMID 23364665.
- ^ McNicol ED, Midbari A, Eisenberg E (avgust 2013). "Neyropatik og'riq uchun opioidlar". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 8 (8): CD006146. doi:10.1002 / 14651858.CD006146.pub2. PMC 6353125. PMID 23986501.
- ^ a b v Amerika bosh og'rig'i jamiyati (Sentyabr 2013), "Shifokorlar va bemorlar so'rashlari kerak bo'lgan beshta narsa", Aql bilan tanlash: ning tashabbusi ABIM Foundation, Amerika bosh og'rig'i jamiyati, dan arxivlangan asl nusxasi 2013 yil 3-dekabrda, olingan 10 dekabr 2013, qaysi havola
- Bigal ME, Lipton RB (aprel, 2009). "Opioiddan ortiqcha foydalanish va surunkali migren rivojlanishi". Og'riq. 142 (3): 179–82. doi:10.1016 / j.pain.2009.01.013. PMID 19232469. S2CID 27949021.
- Bigal ME, Serrano D, Buse D, Scher A, Stewart WF, Lipton RB (sentyabr 2008). "O'tkir migrenli dorilar va epizodikdan surunkali migrengacha evolyutsiyasi: uzunlamasına populyatsiyaga asoslangan tadqiqot". Bosh og'rig'i. 48 (8): 1157–68. doi:10.1111 / j.1526-4610.2008.01217.x. PMID 18808500.
- Scher AI, Stewart WF, Ricci JA, Lipton RB (2003 yil noyabr). "Populyatsiyaga asoslangan tadqiqotda surunkali kunlik bosh og'rig'ining paydo bo'lishi va remissiyasi bilan bog'liq omillar". Og'riq. 106 (1–2): 81–9. doi:10.1016 / S0304-3959 (03) 00293-8. PMID 14581114. S2CID 29000302.
- Katsarava Z, Schneeweiss S, Kurth T, Kroener U, Fritsche G, Eikermann A va boshq. (2004 yil mart). "Epizodik migren bilan og'rigan bemorlarda bosh og'rig'ining surunkali holati va predikatorlari". Nevrologiya. 62 (5): 788–90. doi:10.1212 / 01.WNL.0000113747.18760.D2. PMID 15007133. S2CID 20759425.
- ^ Manchikanti L, Helm S, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV (iyul 2012). "Qo'shma Shtatlarda opioid epidemiyasi". Og'riq shifokori. 15 (3 ta qo'shimcha): ES9-38. PMID 22786464.
- ^ Chou R, Ballantyne JK, Fanciullo GJ, Fine PG, Miaskovskiy C (fevral 2009). "Surunkali saraton bo'lmagan og'riqlarda opioidlardan foydalanish bo'yicha tadqiqot bo'shliqlari: Amerika Pain Society va American Pain Medicine Academy klinik amaliyot qo'llanmasiga oid dalillarni ko'rib chiqish natijalari". Og'riq jurnali. 10 (2): 147–59. doi:10.1016 / j.jpain.2008.10.007. PMID 19187891.
- ^ "Og'riq". Painjournalonline.com. 1 sentyabr 2015 yil. Olingan 7 yanvar 2016.
- ^ Kissin I (2015 yil 28-sentyabr). "Surunkali noaniq og'riqni uzoq muddatli opioid bilan davolash: tasdiqlanmagan samaradorlik va beparvo qilingan xavfsizlik?". Og'riq tadqiqotlari jurnali. 6: 513–29. doi:10.2147 / JPR.S47182. PMC 3712997. PMID 23874119.
- ^ Dhalla IA, Gomes T, Mamdani MM, Juurlink DN (yanvar 2012). "Opioidlar saraton bo'lmagan og'riqlarda steroid bo'lmagan yallig'lanishga qarshi dorilarga qarshi". Kanadalik oilaviy shifokor. 58 (1): 30. PMC 3264005. PMID 22267615.
- ^ Marret E, Beloeil H, Leyj S (mart 2009). "[Opioid bo'lmagan analjeziklarning operatsiyadan keyingi opioidlar bilan birlashtirilishining afzalliklari va xavfi qanday?]". Annales Françaises d'Anesthésie et de Reanimatsiya. 28 (3): e135-51. doi:10.1016 / j.annfar.2009.01.006. PMID 19304445.
- ^ Franceschi F, Iacomini P, Marsiliani D, Cordischi C, Antonini EF, Alesi A va boshq. (2013 yil avgust). "Turli xil kelib chiqadigan og'riqlarni davolashda asetaminofen-kodein kombinatsiyasining xavfsizligi va samaradorligi" (PDF). Tibbiyot va farmakologiya fanlari uchun Evropa sharhi. 17 (16): 2129–35. PMID 23893177.
- ^ Chung KF, Widdicombe J (2008). Yo'talning farmakologiyasi va terapevtikasi. Berlin: Springer. p. 248. ISBN 9783540798422.
- ^ Bolser DC, Davenport PW (2007 yil fevral). "Kodein va yo'tal: samarasiz oltin standart". Allergiya va klinik immunologiya bo'yicha hozirgi fikr. 7 (1): 32–6. doi:10.1097 / ACI.0b013e3280115145. PMC 2921574. PMID 17218808.
- ^ a b Goldman RD (2010 yil dekabr). "Bolalardagi o'tkir yo'tal uchun kodein". Kanadalik oilaviy shifokor. 56 (12): 1293–4. PMC 3001921. PMID 21156892.
- ^ Pol IM (2012 yil fevral). "Bolalarda yuqori nafas yo'llarining infektsiyalari sababli o'tkir yo'talni davolash usullari". O'pka. 190 (1): 41–4. doi:10.1007 / s00408-011-9319-y. PMID 21892785. S2CID 23865647.
- ^ Verlee L, Verheij TJ, Hopstaken RM, Prins JM, Salomé PL, Bindels PJ (2012). "[" O'tkir yo'tal "NHG amaliyoti qo'llanmasining qisqacha mazmuni]" ". Genereskunde uchun Nederlands Tijdschrift. 156: A4188. PMID 22917039.
- ^ Matthys H, Bleicher B, Bleicher U (1983). "Dekstrometorfan va kodein: surunkali yo'tal bilan og'rigan bemorlarda antitussiv faollikni ob'ektiv baholash". Xalqaro tibbiy tadqiqotlar jurnali. 11 (2): 92–100. doi:10.1177/030006058301100206. PMID 6852361. S2CID 30521239.
- ^ Van Amburg JA. "Yo'talni davolash usullari ish beradimi?". Medscape. Olingan 10 aprel 2016.
- ^ Bolser DC (fevral, 2010). "Yo'talni farmakologik boshqarish". Shimoliy Amerikaning otorinolaringologik klinikalari. 43 (1): 147-55, xi. doi:10.1016 / j.otc.2009.11.008. PMC 2827356. PMID 20172264.
- ^ Vebster LR (oktyabr 2015). "Opioid ta'sirida ich qotishi". Og'riq dori. 16 Qo'shimcha 1: S16-21. doi:10.1111 / pme.12911. PMID 26461071.
- ^ "Matbuot e'lonlari - FDA opioid ta'sirida ich qotishi uchun Movantikni tasdiqlaydi". www.fda.gov. Olingan 18 fevral 2016.
- ^ Gallagher R (2011 yil iyul). "O'tkir kasallikda nafas qisilishi uchun opioidlardan foydalanish". CMAJ. 183 (10): 1170. doi:10.1503 / cmaj.110024. PMC 3134725. PMID 21746829.
- ^ Wiseman R, Rowett D, Allcroft P, Abernethy A, Currow DC (mart 2013). "Surunkali refrakter dispniya - dalillarga asoslangan boshqarish". Avstraliya oilaviy shifokori. 42 (3): 137–40. PMID 23529525.
- ^ a b v d e f g h Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E (may 2006). "Surunkali saraton bo'lmagan og'riq uchun opioidlar: samaradorlik va yon ta'sirining meta-tahlili". CMAJ. 174 (11): 1589–94. doi:10.1503 / cmaj.051528. PMC 1459894. PMID 16717269.
- ^ Baumann S (2009). "Keksa yoshdagi kattalardagi og'riqni davolashda parvarish qilish usuli". Medsurg hamshirasi. 18 (2): 77-82, viktorina 83. PMID 19489204.
- ^ Buckeridge D, Huang A, Hanley J, Kelome A, Reidel K, Verma A va boshq. (Sentyabr 2010). "Katta yoshdagi opioiddan foydalanish bilan bog'liq shikastlanish xavfi". Amerika Geriatriya Jamiyati jurnali. 58 (9): 1664–70. doi:10.1111 / j.1532-5415.2010.03015.x. PMID 20863326.
- ^ Schneider JP (2010). "Mushak-skelet tizimining surunkali og'rig'ida opioid analjeziklaridan oqilona foydalanish". J Muskuloskel Med. 27: 142–148.
- ^ Sanger N, Bhatt M, Singhal N, Ramsden K, Baptist-Mohseni N, Panesar B va boshq. (Mart 2019). "O'tkir bel og'rig'i uchun retsept bo'yicha opioidlar bilan bog'liq salbiy natijalar: tizimli tahlil va meta-tahlil". Og'riq shifokori. 22 (2): 119–138. PMID 30921976.
- ^ Fuggle N, Kurtis E, Shou S, Qoshiqchi L, Bruyer O, Ntani G va boshq. (Aprel 2019). "Osteoartritdagi opioidlarning xavfsizligi: tizimli tahlil va meta-tahlil natijalari". Giyohvand moddalar va qarish. 36 (Qo'shimcha 1): 129–143. doi:10.1007 / s40266-019-00666-9. PMC 6509215. PMID 31073926.
- ^ Monnelly VJ, Hamilton R, Chappell FM, Mactier H, Boardman JP (iyul 2019). "Homiladorlik davrida opioidga bog'liqlik uchun metadonni parvarishlash bo'yicha retseptdan keyin bolalik davridagi neyro rivojlanish: tizimli tahlil va meta-tahlil". Rivojlantiruvchi tibbiyot va bolalar nevrologiyasi. 61 (7): 750–760. doi:10.1111 / dmcn.14117. PMC 6617808. PMID 30511742.
- ^ Volf K (2002 yil avgust). "Metadonning haddan tashqari dozasini tavsifi: klinik mulohazalar va ilmiy dalillar". Giyohvand moddalarning terapevtik monitoringi. 24 (4): 457–70. doi:10.1097/00007691-200208000-00001. PMID 12142628. S2CID 5652295.
- ^ Teichtahl H, Vang D (2007 yil noyabr). "Opioidni surunkali qo'llash bilan uyqusiz nafas olish". Giyohvand moddalar xavfsizligi bo'yicha mutaxassislarning fikri. 6 (6): 641–9. doi:10.1517/14740338.6.6.641. PMID 17967153. S2CID 24688704.
- ^ Giyohvand moddalarni baholash va tadqiqotlar markazi (2013 yil 23-avgust). "Postmarket bemorlar va provayderlar uchun dori xavfsizligi to'g'risida ma'lumot - sog'liqni saqlash xodimlari uchun metadon gidroxlorid uchun ma'lumot". AQSh oziq-ovqat va farmatsevtika idorasi. Olingan 24 fevral 2016.
Metadonning yarim yemirilish davri (8-59 soat) analjezik ta'siridan (4-8 soat) uzoqroq.
- ^ Stephens E (2015 yil 23-noyabr). "Opioid toksikligi". Medscape. Olingan 24 fevral 2016.
CDC, metadon 1999-2010 yillarda Qo'shma Shtatlarda opioid bilan bog'liq o'limning 31,4% ga hissa qo'shganligini xabar qildi. Metadon, shuningdek, bitta dori bilan bog'liq bo'lgan opioid bilan bog'liq o'limlarning 39,8% ni tashkil etdi. Metadon bilan bog'liq dozani oshirib yuboradigan o'lim darajasi ko'p dori va bir martalik o'lim orasida opioid bilan bog'liq boshqa o'limlarga qaraganda ancha yuqori edi.
- ^ a b v d Noble M, Treadwell JR, Tregear SJ, Coates VH, Wiffen PJ, Akafomo C, Schoelles KM (yanvar 2010). Noble M (tahrir). "Surunkali saraton bo'lmagan og'riqlarni uzoq muddatli opioid bilan davolash". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (1): CD006605. doi:10.1002 / 14651858.CD006605.pub2. PMC 6494200. PMID 20091598.
- ^ "Qo'shma Shtatlarda giyohvand moddalarni haddan tashqari oshirib yuborishda o'lim, 1999–2016" (PDF). CDC. Olingan 23 dekabr 2017.
- ^ a b v d e Dozani oshirib yuborish o'lim darajasi. By Giyohvandlik bo'yicha Milliy institut (NIDA).
- ^ Fentanil. 17-rasmdan 4-rasm. AQSh DEA (Giyohvandlikka qarshi kurash boshqarmasi ).
- ^ Pradhan AA, Walwyn V, Nozaki C, Filliol D, Erbs E, Matifas A va boshq. (2010 yil dekabr). "Bivioid retseptorlarini in vivo jonli ravishda ligand tomonidan olib o'tilishi: og'riq qoldiruvchi bag'rikenglik tomon ikki yo'l". Neuroscience jurnali. 30 (49): 16459–68. doi:10.1523 / JNEUROSCI.3748-10.2010. PMC 3086517. PMID 21147985.
- ^ Kollars JP, Larson MD (mart 2005). "Opioidlarning miotik ta'siriga chidamlilik". Anesteziologiya. 102 (3): 701. doi:10.1097/00000542-200503000-00047. PMID 15731628.
- ^ Santillan R, Maestre JM, Hurle MA, Florez J (iyul 1994). "Morfin bilan surunkali davolangan saraton kasalligida opiat analjeziyasini nimodipin bilan kuchaytirish: dastlabki hisobot". Og'riq. 58 (1): 129–32. doi:10.1016/0304-3959(94)90192-9. PMID 7970835. S2CID 35138704.
- ^ Santillan R, Hurle MA, Armijo JA, de los Mozos R, Flóres J (may 1998). "Morfin dozasini oshirishni talab qiladigan saraton kasalligida Nimodipin bilan kuchaytirilgan opiat analjeziyasi: er-xotin ko'r, platsebo nazorati ostida o'tkazilgan tadqiqot". Og'riq. 76 (1–2): 17–26. doi:10.1016 / S0304-3959 (98) 00019-0. PMID 9696455. S2CID 30963675.
- ^ Smit FL, Dombrowski DS, Dewey WL (1999 yil fevral). "Sichqonlarda hujayra ichidagi kaltsiyni morfinga chidamliligiga jalb qilish". Farmakologiya, biokimyo va o'zini tutish. 62 (2): 381–8. doi:10.1016 / S0091-3057 (98) 00168-3. PMID 9972707. S2CID 37434490.
- ^ Makkarti RJ, Kroin JS, Tuman KJ, Penn RD, Ivankovich AD (aprel 1998). "Kalamushlarga magniy sulfat va morfinni intratekal qo'shib yuborish orqali antinotsitseptiv kuch va bag'rikenglikning susayishi". Anesteziya va og'riqsizlantirish. 86 (4): 830–6. doi:10.1097/00000539-199804000-00028. PMID 9539610.
- ^ Morrison AP, Hunter JM, Halpern SH, Banerji A (may 2013). "Lipofil opioidli va bo'lmagan holda lokal anestezikaning mavjudligi yoki yo'qligida intratekal magneziumning ta'siri: tizimli tahlil va meta-tahlil". Britaniya behushlik jurnali. 110 (5): 702–12. doi:10.1093 / bja / aet064. PMID 23533255.
- ^ Larson AA, Kovach KJ, Spartz AK (Noyabr 2000). "Intratekal Zn2 + morfin antinotsitseptsiyasi va o'tkir bag'rikenglikning rivojlanishini susaytiradi". Evropa farmakologiya jurnali. 407 (3): 267–72. doi:10.1016 / S0014-2999 (00) 00715-9. PMID 11068022.
- ^ Vong CS, Cherng CH, Luk HN, Ho ST, Tung CS (fevral 1996). "NMDA retseptorlari antagonistlarining kalamushlarda morfin bardoshligini inhibe qilishga ta'siri: mu-opioid retseptorlari bilan bog'lanish". Evropa farmakologiya jurnali. 297 (1–2): 27–33. doi:10.1016/0014-2999(95)00728-8. PMID 8851162.
- ^ Malec D, Mandryk M, Fidecka S (2008 yil mart-aprel). "Sichqonlarda morfin va pentazotsin ta'sirida antinotsitseptsiyada memantin va ketaminning o'zaro ta'siri" (PDF). Farmakologik hisobotlar. 60 (2): 149–55. PMID 18443375.
- ^ McCleane GJ (2003). "Xoletsistokinin antagonisti proglumid dihidrokodeinning og'riq qoldiruvchi ta'sirini kuchaytiradi". Og'riqning klinik jurnali. 19 (3): 200–1. doi:10.1097/00002508-200305000-00008. PMID 12792559. S2CID 29229782.
- ^ Watkins LR, Kinscheck IB, Mayer DJ (aprel 1984). "Opiat analjeziyasining kuchayishi va proglumid bilan morfinga chidamliligining aniq o'zgarishi". Ilm-fan. 224 (4647): 395–6. Bibcode:1984Sci ... 224..395W. doi:10.1126 / science.6546809. PMID 6546809.
- ^ Tang J, Chou J, Iadarola M, Yang XY, Kosta E (iyun 1984). "Proglumid kalamushlarda morfinga nisbatan chidamliligini oldini oladi va kamaytiradi". Neyrofarmakologiya. 23 (6): 715–8. doi:10.1016/0028-3908(84)90171-0. PMID 6462377. S2CID 33168040.
- ^ Ledeboer A, Xatchinson MR, Uotkins LR, Jonson KV (2007 yil iyul). "Ibudilast (AV-411). Neyropatik og'riq va opioidni olib tashlash sindromi uchun yangi terapevtik nomzod". Tergov narkotiklari bo'yicha mutaxassislarning fikri. 16 (7): 935–50. doi:10.1517/13543784.16.7.935. PMID 17594181. S2CID 22321634.
- ^ Islom MM (2019). "Avstraliyada yangi foydalanuvchilar orasida retsept bo'yicha beriladigan opioidlar va benzodiazepinlarni tarqatish sxemasi va ehtimoli: retrospektiv kohort tadqiqotlari". BMJ ochiq. 9 (12): e030803. doi:10.1136 / bmjopen-2019-030803. PMC 6955558. PMID 31892646.
- ^ a b v d Doyl D, Xenks G, Cherni I, Kalman K, nashr. (2004). Oksford Palliativ tibbiyot darsligi (3-nashr). Oksford universiteti matbuoti. ISBN 978-0198566984.
- ^ Hermann D, Klages E, Welzel H, Mann K, Croissant B (iyun 2005). "Opioidni olib tashlash simptomlarida opioid bo'lmagan dorilarning past samaradorligi". Giyohvandlik biologiyasi. 10 (2): 165–9. doi:10.1080/13556210500123514. PMID 16191669.
- ^ Jigarrang TK (mart 2013). "Ibogaine moddalarga qaramlikni davolashda". Giyohvand moddalarni suiste'mol qilish bo'yicha hozirgi sharhlar. 6 (1): 3–16. doi:10.2174/15672050113109990001. PMID 23627782.
- ^ Duceppe, Mark-Aleksandr; Perreault, Mark M.; Frenette, Anne Julie; Burri, Liza D.; Riko, Filipp; Lavoie, Enni; Gélinas, Céline; Mehta, Sangeeta; Dagenais, Maryse; Uilyamson, Devid R. (aprel, 2019). "Og'ir kasallikka chalingan yangi tug'ilgan chaqaloqlarda, bolalar va kattalarda opioidlar va benzodiazepinlardan yatrogenik ajralish chastotasi, xavf omillari va simptomatologiyasi: Klinik tadqiqotlarni tizimli ko'rib chiqish". Klinik farmatsiya va terapiya jurnali. 44 (2): 148–156. doi:10.1111 / jcpt.12787. ISSN 1365-2710. PMID 30569508.
- ^ Bannvart B (sentyabr 2012). "Opioidli analjeziklarni suiiste'mol qiluvchi vositalar o'z maqsadlariga erishishda muvaffaqiyatli bo'ladimi?". Giyohvand moddalar. 72 (13): 1713–23. doi:10.2165/11635860-000000000-00000. PMID 22931520. S2CID 26082561.
- ^ Schneider JP, Matthews M, Jamison RN (oktyabr 2010). "Suiiste'mol qiluvchi va tahqirlashga chidamli opioid formulalari: retsept bo'yicha opioidni suiiste'mol qilishda ularning ahamiyati qanday?". CNS dorilar. 24 (10): 805–10. doi:10.2165/11584260-000000000-00000. PMID 20839893. S2CID 17830622.
- ^ Xu Y, Jonson A (2013). "Saraton bo'lmagan og'riqlarga qarshi opioidli terapiya farmakogenomikasi: samaradorligi, noxush hodisalari va xarajatlari". Og'riqni o'rganish va davolash. 2013: 943014. doi:10.1155/2013/943014. PMC 3791560. PMID 24167729.
- ^ Brush DE (2012 yil dekabr). "Surunkali og'riqni davolash uchun uzoq muddatli opioid terapiyasining asoratlari: opioid ta'siridan kelib chiqqan giperaljeziya paradoksi". Tibbiy toksikologiya jurnali. 8 (4): 387–92. doi:10.1007 / s13181-012-0260-0. PMC 3550256. PMID 22983894.
- ^ Malik Z, Baik D, Schey R (fevral, 2015). "Kannabinoidlarning ko'ngil aynish va gijjalar va ichki og'riqlarni boshqarishda ahamiyati". Gastroenterologiya bo'yicha joriy hisobotlar. 17 (2): 429. doi:10.1007 / s11894-015-0429-1. PMID 25715910. S2CID 32705478.
- ^ Abrams DI, Guzman M (iyun 2015). "Saraton kasalligini davolashda nasha". Klinik farmakologiya va terapiya. 97 (6): 575–86. doi:10.1002 / cpt.108. PMID 25777363.
- ^ "UCSF tadqiqotlari tibbiy marixuana bemorlarga afyun bilan og'riqni kamaytirishga yordam berishi mumkinligini aniqladi". San-Fransisko UC. Olingan 4 mart 2016.
- ^ Abrams DI, Couey P, Shade SB, Kelly ME, Benowitz NL (dekabr 2011). "Surunkali og'riq paytida kannabinoid-opioidning o'zaro ta'siri". Klinik farmakologiya va terapiya. 90 (6): 844–51. doi:10.1038 / clpt.2011.188. PMID 22048225.
- ^ Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E (may, 2019). "Operatsiya ichidagi opioidlarning analjezik ta'siri va opioidsiz behushlik: tizimli tahlil va meta-tahlil". Anesteziya. 74 (5): 651–662. doi:10.1111 / ana.14582. PMID 30802933. S2CID 73469631.
- ^ Busse, Jeyson V.; Vang, Li; Kamaleldin, Mostafa; Kreygi, Samanta; Riva, Jon J.; Montoya, Luis; Mulla, Sohail M.; Lopes, Luciane C.; Vogel, Nikol; Chen, Erik; Kirmayr, Karin (2018 yil 18-dekabr). "Surunkali saraton bo'lmagan og'riq uchun opioidlar: tizimli tahlil va meta-tahlil". JAMA. 320 (23): 2448–2460. doi:10.1001 / jama.2018.18472. ISSN 0098-7484. PMC 6583638. PMID 30561481.
- ^ Reissig JE, Rybarczyk AM (aprel 2005). "Surunkali og'riq paytida opioid ta'sirida sedatsiyani farmakologik davolash". Farmakoterapiya yilnomalari. 39 (4): 727–31. doi:10.1345 / aph.1E309. PMID 15755795. S2CID 39058371.
- ^ Corey PJ, Heck AM, Weathermon RA (dekabr 1999). "Opioid ta'sirida tinchlantirishga qarshi amfetaminlar". Farmakoterapiya yilnomalari. 33 (12): 1362–6. doi:10.1345 / aph.19024. PMID 10630837. S2CID 23733242.
- ^ Sog'liqni saqlashda dori vositalari va texnologiyalar bo'yicha Kanada agentligi (2014 yil 26-iyun). "Kabızlığın oldini olish yoki boshqarish uchun dioktil sulfosüksinat yoki dokusat (kaltsiy yoki natriy): Klinik samaradorligini qayta ko'rib chiqish". PMID 25520993.
- ^ McCarberg BH (iyul 2013). "Opioid ta'sirida ich qotishining umumiy ko'rinishi va davolashi". Aspiranturadan keyingi tibbiyot. 125 (4): 7–17. doi:10.3810 / pgm.2013.07.2651. PMID 23782897. S2CID 42872181.
- ^ a b v d e Kumar L, Barker C, Emmanuel A (2014). "Opioid ta'sirida ich qotishi: patofiziologiya, klinik oqibatlar va boshqarish". Gastroenterologiya tadqiqotlari va amaliyoti. 2014: 141737. doi:10.1155/2014/141737. PMC 4027019. PMID 24883055.
- ^ a b Alguire PC, Amerika shifokorlar kolleji, ichki kasalliklar bo'yicha xizmat ko'rsatuvchi direktorlar (2009). Klerklik talabalari uchun ichki kasalliklar uchun zarur bo'lgan narsalar 2. ACP tugmachasini bosing. 272– betlar. ISBN 978-1-934465-13-4.
- ^ a b v Elliott JA, Smit XS (2016 yil 19 aprel). O'tkir og'riqni boshqarish bo'yicha qo'llanma. CRC Press. 89– betlar. ISBN 978-1-4665-9635-1.
- ^ Nishie, Kenichi; Yamamoto, Shuxey; Yamaga, Takayoshi; Horigome, Naoto; Xanaoka, Masayuki (2019 yil may). "Opioid kelib chiqadigan konstipatsiyani davolash uchun periferik ta'sir qiluvchi m-opioid antagonisti: Tizimli ko'rib chiqish va meta-tahlil". Gastroenterologiya va gepatologiya jurnali. 34 (5): 818–829. doi:10.1111 / jgh.14586. ISSN 1440-1746. PMID 30597600.
- ^ Poulsen JL, Brok C, Olesen AE, Nilsson M, Drewes AM (noyabr 2015). "Opioid ta'sirida ichak disfunktsiyasini davolashda rivojlanayotgan paradigmalar". Gastroenterologiyaning terapevtik yutuqlari. 8 (6): 360–72. doi:10.1177 / 1756283X15589526. PMC 4622283. PMID 26557892.
- ^ Devis MP, Goforth HW (2016). "Opioid retseptorlari antagonisti bo'lgan oksikodon: sharh". Opioidlarni boshqarish jurnali. 12 (1): 67–85. doi:10.5055 / jom.2016.0313. PMID 26908305.
- ^ Candy B, Jons L, Vickerstaff V, Larkin PJ, Stone P (iyun 2018). "Saratonga chalingan va palyatif yordam ko'rsatadigan odamlarda opioid ta'sirida ichak disfunktsiyasining mu-opioid antagonistlari". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 6: CD006332. doi:10.1002 / 14651858.CD006332.pub3. PMC 6513061. PMID 29869799.
- ^ Luthra P, Burr NE, Brenner DM, Ford AC (may 2018). "Opioid kelib chiqadigan ich qotishini davolash uchun farmakologik terapiya samaradorligi: tizimli tahlil va tarmoqdagi meta-tahlil" (PDF). Ichak. 68 (3): 434–444. doi:10.1136 / gutjnl-2018-316001. PMID 29730600. S2CID 13677764.
- ^ Esmadi M, Ahmad D, Xyulett A (mart 2019). "Opioid ta'sirida ich qotib qolishni davolashda naldemedinning samaradorligi: meta-tahlil". Gastrointestinal va jigar kasalliklari jurnali. 28 (1): 41–46. doi:10.15403 / jgld.2014.1121.281. har qanday. PMID 30851171.
- ^ Dorn S, Lembo A, Cremonini F (sentyabr 2014). "Opioid bilan bog'liq ichak disfunktsiyasi: epidemiologiya, patofiziologiya, diagnostika va dastlabki terapevtik usul". Amerika Gastroenterologiya qo'shimchalari jurnali. 2 (1): 31–7. doi:10.1038 / ajgsup.2014.7. PMID 25207610.
- ^ Yost CS (2006). "Doksapram nafas olish stimulyatoriga yangi ko'rinish". CNS giyohvand moddalarni ko'rib chiqish. 12 (3–4): 236–49. doi:10.1111 / j.1527-3458.2006.00236.x. PMC 6506195. PMID 17227289.
- ^ Tan ZM, Liu JH, Dong T, Li JX (2006 yil avgust). "[Og'riqsiz sun'iy abortda propofol va doksapram bilan kombinatsiyalangan maqsadli boshqariladigan remifentanil infuziyasining klinik kuzatuvi]". Nan Fang Yi Ke da Xue Xue Xue Bao = Janubiy tibbiyot universiteti jurnali. 26 (8): 1206–8. PMID 16939923.
- ^ Manzke T, Guenther U, Ponimaskin E.G., Haller M, Dutschmann M, Shvartsaxer S, Rixter DW (2003 yil iyul). "5-HT4 (a) retseptorlari opioid ta'sirida nafas olish depressiyasini og'riqsizlantirishni yo'qotmasdan oldini oladi". Ilm-fan. 301 (5630): 226–9. Bibcode:2003Sci ... 301..226M. doi:10.1126 / science.1084674. PMID 12855812. S2CID 13641423.
- ^ Vang X, Dergacheva O, Kamendi H, Gorini C, Mendelovits D (avgust 2007). "5-gidroksitriptamin 1A / 7 va 4fa retseptorlari miya sopi kardiorespiratuar funktsiyasining opioid ta'sirida inhibisyonini differentsial ravishda oldini oladi". Gipertenziya. 50 (2): 368–76. doi:10.1161 / HYPERTENSIONAHA.107.091033. PMID 17576856.
- ^ Ren J, Poon BY, Tang Y, Funk GD, Greer JJ (dekabr 2006). "Ampakinlar kalamushlarda nafas olish tushkunligini engillashtiradi". Amerika nafas olish va tanqidiy tibbiyot jurnali. 174 (12): 1384–91. doi:10.1164 / rccm.200606-778OC. PMID 16973981.
- ^ Cozowicz, Crispiana; Chung, Frensis; Doufas, Anthony G.; Nagappa, Mahesh; Memtsoudis, Stavros G. (oktyabr 2018). "Obstruktiv uyqu apnesi bo'lgan bemorlarda o'tkir og'riqni boshqarish bo'yicha opioidlar: tizimli tahlil". Anesteziya va og'riqsizlantirish. 127 (4): 988–1001. doi:10.1213 / ANE.000000000000353549. ISSN 1526-7598. PMID 29958218.
- ^ Gupta, Kapil; Nagappa, Mahesh; Prasad, Arun; Abramyan, Lyusin; Vong, Jan; Vaynarten, Tobi N.; Chung, Frensis (2018 yil 14-dekabr). "Jarrohlik bemorlarida opioid ta'siridagi nafas olish depressiyasining xavf omillari: tizimli tahlil va meta-tahlillar". BMJ ochiq. 8 (12): e024086. doi:10.1136 / bmjopen-2018-024086. ISSN 2044-6055. PMC 6303633. PMID 30552274.
- ^ Wilson GR, Reisfield GM (2003). "Morfin giperaljeziyasi: voqea haqida hisobot". Amerikalik xospis va palliativ yordam jurnali. 20 (6): 459–61. doi:10.1177/104990910302000608. PMID 14649563. S2CID 22690630.
- ^ Vella-Brincat J, Macleod AD (2007). "Opioidlarning palliativ yordam ko'rsatadigan bemorlarning markaziy asab tizimiga salbiy ta'siri". Og'riq va palliativ yordam farmakoterapiyasi jurnali. 21 (1): 15–25. doi:10.1080 / J354v21n01_05. PMID 17430825. S2CID 17757207.
- ^ Mercadante S, Arcuri E (2005). "Giperaljeziya va opioidni almashtirish". Amerikalik xospis va palliativ yordam jurnali. 22 (4): 291–4. doi:10.1177/104990910502200411. PMID 16082916. S2CID 39647898.
- ^ Fine PG (2004). "Opioid tushunchalari: opioidga bog'liq giperaljeziya va opioidning aylanishi". Og'riq va palliativ yordam farmakoterapiyasi jurnali. 18 (3): 75–9. doi:10.1080 / J354v18n03_08. PMID 15364634. S2CID 45555785.
- ^ Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L (2011). "Opioid ta'sirida yuzaga keladigan giperaljeziyani kompleks ko'rib chiqish". Og'riq shifokori. 14 (2): 145–61. PMID 21412369.
- ^ Tompkins DA, Kempbell CM (aprel 2011). "Opioid bilan bog'liq giperaljeziya: klinik jihatdan ahamiyatli yoki begona tadqiqot hodisasi?". Hozirgi og'riq va bosh og'rig'i haqida hisobotlar. 15 (2): 129–36. doi:10.1007 / s11916-010-0171-1. PMC 3165032. PMID 21225380.
- ^ Diaz JL, Zamanillo D, Corbera J, Baeyens JM, Maldonado R, Perikas MA va boshq. (Sentyabr 2009). "Selektiv sigma-1 (sigma1) retseptorlari antagonistlari: neyropatik og'riqni davolash uchun paydo bo'lgan maqsad". Tibbiy kimyo markaziy asab tizimining agentlari. 9 (3): 172–83. doi:10.2174/1871524910909030172. PMID 20021351.
- ^ Mitra S (2018). "Opioid bilan bog'liq giperaljeziya: patofiziologiya va klinik oqibatlari". Opioidlarni boshqarish jurnali. 4 (3): 123–30. doi:10.5055 / jom.2008.0017. PMID 18717507.
- ^ Baron R (2009). "Neyropatik og'riq: Klinik istiqbol". Sensor asab. Eksperimental farmakologiya bo'yicha qo'llanma. 194. 3-30 betlar. doi:10.1007/978-3-540-79090-7_1. ISBN 978-3-540-79089-1. PMID 19655103.
- ^ Candiotti KA, Gitlin MC (2010 yil iyul). "Opioid bilan bog'liq nojo'ya ta'sirlarning saraton kasalligidan mo''tadil va og'ir surunkali davolanishga ta'sirini ko'rib chiqish: tapentadol, echimga qadam?". Hozirgi tibbiy tadqiqotlar va fikrlar. 26 (7): 1677–84. doi:10.1185/03007995.2010.483941. PMID 20465361. S2CID 9713245.
- ^ a b Fountas A, Chai ST, Kourkouti C, Karavitaki N (oktyabr 2018). "ENDOKRINOLOGIYA MEXANIZMALARI: Opioidlarning endokrinologiyasi". Evropa Endokrinologiya jurnali. 179 (4): R183-R196. doi:10.1530 / EJE-18-0270. PMID 30299887.
- ^ Brennan MJ (2013 yil mart). "Opioid terapiyasining endokrin funktsiyaga ta'siri". Amerika tibbiyot jurnali. 126 (3 ta qo'shimcha 1): S12-8. doi:10.1016 / j.amjmed.2012.12.001. PMID 23414717.
- ^ Colameco S, Coren JS (yanvar 2009). "Opioid bilan bog'liq endokrinopatiya". Amerika Osteopatik Assotsiatsiyasi jurnali. 109 (1): 20–5. PMID 19193821.
- ^ Smit XS, Elliott JA (2012 yil iyul). "Opioid ta'sirida androgen etishmovchiligi (OPIAD)". Og'riq shifokori. 15 (3 ta qo'shimcha): ES145-56. PMID 22786453.
- ^ Brede E, Mayer TG, Gatchel RJ (2012 yil fevral). "Ish jarohatlarida fanlararo funktsional tiklanishdan keyin 1 yil o'tgach, ish joyini saqlab qolmaslik prognozi". Jismoniy tibbiyot va reabilitatsiya arxivlari. 93 (2): 268–74. doi:10.1016 / j.apmr.2011.08.029. PMID 22289236.
- ^ Volinn E, Fargo JD, Fine PG (2009 yil aprel). "Nonspesifik bel og'rig'iga qarshi opioid terapiyasi va surunkali ish yo'qotish natijalari". Og'riq. 142 (3): 194–201. doi:10.1016 / j.pain.2008.12.017. PMID 19181448.
- ^ a b v Amerika kasbiy va atrof-muhit tibbiyoti kolleji (2014 yil fevral), "Shifokorlar va bemorlar so'rashlari kerak bo'lgan beshta narsa", Aql bilan tanlash: ning tashabbusi ABIM Foundation, Amerika kasb-hunar va atrof-muhit tibbiyoti kolleji, olingan 24 fevral 2014, qaysi havola
- Vays MS, Bowden K, Branco F va boshq. (2011). "Opioidlar bo'yicha ko'rsatma". Hegmann KT-da (tahrir). Kasbiy tibbiyot bo'yicha ko'rsatmalar: sog'liqdagi umumiy muammolarni baholash va boshqarish va ishchilarning funktsional tiklanishi (onlayn mart 2014) (3-nashr). Elk Grove Village, IL: Amerika kasb-hunar va atrof-muhit tibbiyoti kolleji. p. 11. ISBN 978-0615452272.
- ^ Cherubino P, Sarzi-Puttini P, Zuccaro SM, Labianca R (fevral, 2012). "Bemorning muhim kichik guruhlarida surunkali og'riqni boshqarish". Giyohvand moddalarni klinik tekshirish. 32 Qo'shimcha 1: 35-44. doi:10.2165/11630060-000000000-00000. PMID 23389874. S2CID 47576095.
- ^ White KT, Dillingham TR, Gonsales-Fernández M, Rotfild L (Dekabr 2009). "Surunkali noaniq og'riqli sindromlar uchun dorilar: ambulatoriya poliklinikasini boshqarish uchun tegishli nomzodlarni aniqlash mumkinmi?". Amerikalik jismoniy tibbiyot va reabilitatsiya jurnali. 88 (12): 995–1001. doi:10.1097 / PHM.0b013e3181bc006e. PMID 19789432. S2CID 43241757.
- ^ Kaye AM, Kaye AD, Lofton EC (2013). "Opioidlarni tayinlashda asosiy tushunchalar va avtoulovga vositachilik ta'sirining hozirgi tushunchalari". Ochsner jurnali. 13 (4): 525–32. PMC 3865831. PMID 24358001.
- ^ Orriols L, Delorme B, Gadegbeku B, Tricotel A, Contrand B, Laumon B va boshq. (2010 yil noyabr). Pirmohamed M (tahrir). "Retsept bo'yicha dori-darmonlar va yo'lda avtohalokatlar xavfi: Frantsiyaning ro'yxatga olish kitobiga asoslangan tadqiqot". PLOS tibbiyoti. 7 (11): e1000366. doi:10.1371 / journal.pmed.1000366. PMC 2981588. PMID 21125020.
- ^ Miller M, Styurmer T, Azrael D, Levin R, Sulaymon DH (mart 2011). "Opioidli analjeziklar va artrit bilan og'rigan kattalardagi sinish xavfi". Amerika Geriatriya Jamiyati jurnali. 59 (3): 430–8. doi:10.1111 / j.1532-5415.2011.03318.x. PMC 3371661. PMID 21391934.
- ^ Allegri N, Mennuni S, Rulli E, Vanakore N, Corli O, Floriani I va boshq. (Mart 2019). "Surunkali saraton kasalligi bilan og'rigan bemorlarda opioidlarni uzoq muddat foydalanishning neyropsikologik ta'sirini tizimli ko'rib chiqish va meta-tahlil". Og'riq amaliyoti. 19 (3): 328–343. doi:10.1111 / papr.12741. PMID 30354006. S2CID 53023743.
- ^ Higgins C, Smith BH, Matthews K (iyun 2019). "Surunkali opioid ta'siridan keyin klinik populyatsiyada opioid bilan bog'liq giperaljeziya dalillari: tizimli tahlil va meta-tahlil" (PDF). Britaniya behushlik jurnali. 122 (6): e114-e126. doi:10.1016 / j.bja.2018.09.019. PMID 30915985.
- ^ Yang, Devid Z.; Gunoh, Billi; Bekxuzen, Joshua; Xia, Dawei; Xaimova, Rebekka; Iliev, Iliya (2019 yil may - iyun). "Jarrohlik bo'lmagan sharoitda opioid ta'siridan kelib chiqqan giperaljeziya: tizimli ko'rib chiqish". Amerika terapiya jurnali. 26 (3): e397-e405. doi:10.1097 / MJT.0000000000000734. ISSN 1536-3686. PMID 29726847. S2CID 19181545.
- ^ a b v Gudin JA, Mogali S, Jons JD, Comer SD (iyul 2013). "Kombinatsiyalangan opioid, benzodiazepinlar va / yoki spirtli ichimliklarni iste'mol qilish xavfi, boshqaruvi va nazorati". Aspiranturadan keyingi tibbiyot. 125 (4): 115–30. doi:10.3810 / pgm.2013.07.2684. PMC 4057040. PMID 23933900.
- ^ Islom MM, Wollersheim D (2019). "Avstraliyada tarqatiladigan opioidlar va benzodiazepinlarni taqqoslash". PLOS ONE. 14 (8): e0221438. doi:10.1371 / journal.pone.0221438. PMC 6699700. PMID 31425552.
- ^ Islom MM, Vollersheim D (2020). "Avstraliyada retseptsiya qilingan opioidlar va benzodiazepinlarni bir vaqtda yuborish tendentsiyalari va o'zgarishlari: retrospektiv tahlil". Giyohvandlikning zamonaviy muammolari. 47 (2): 136–148. doi:10.1177/0091450920919443. S2CID 218780209.
- ^ Stuth EA, Stucke AG, Zuperku EJ (2012). "Anesteziya, sedativ va opioidlarning shamollatish nazoratiga ta'siri". Anesteziklar, sedativlar va opioidlarning ventilyatsiyani boshqarishga ta'siri. Kompleks fiziologiya. 2. 2281–2367 betlar. doi:10.1002 / cphy.c100061. ISBN 9780470650714. PMID 23720250.
- ^ Gowing L, Ali R, White JM (may 2017). "Opioidni olib tashlash uchun minimal sedasyon bilan opioid antagonistlari". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 5: CD002021. doi:10.1002 / 14651858.CD002021.pub4. PMC 6481395. PMID 28553701.
- ^ Bolton, Monika; Xodkinson, Aleks; Boda, Shivani; Kalıp, Alan; Panagioti, Mariya; Rods, Sara; Riste, Liza; van Marveyk, Xarm (2019 yil 15-yanvar). "Og'zaki naltreksonning platsebo randomizatsiyalangan boshqariladigan tekshiruvlarida qayd etilgan jiddiy nojo'ya hodisalar: tizimli tahlil va meta-tahlil. BMC tibbiyoti. 17 (1): 10. doi:10.1186 / s12916-018-1242-0. ISSN 1741-7015. PMC 6332608. PMID 30642329.
- ^ Grin, Jennifer Anne; Deve, Brent J.; Dol, Jyustin S.; Butler, Maykl B. (2019 yil aprel). "Kasalxonaga qadar opioidni haddan tashqari oshirib yuborishda parvarish qilishda" davolash va ozod qilish "amaliyotidan so'ng tiklanish toksikligi tufayli o'lim holatlari: muntazam ravishda qayta ko'rib chiqish". Favqulodda tibbiyot jurnali: EMJ. 36 (4): 219–224. doi:10.1136 / paydo bo'ldi-2018-207534. ISSN 1472-0213. PMID 30580317. S2CID 58607479.
- ^ Miller RD (2010). Millerning behushligi (7-nashr). Elsevier sog'liqni saqlash fanlari. ISBN 978-0-443-06959-8.
- ^ Morgan GE, Mixail MS, Murray MJ (2006). Klinik anesteziologiya (4-nashr). McGraw tepaligi. ISBN 978-0-07-110515-6.
- ^ Kestane DH, Vong CA, Tsen LC, Kee WD, Beilin Y, Mhyre J (2014). Kashtanning akusherlik behushligi: tamoyillari va amaliyoti. Elsevier sog'liqni saqlash fanlari. p. 468. ISBN 9780323113748.
Gidromorfonning lipidda eruvchanligi morfin va fentanil o'rtasida yotadi, ammo morfinga yaqinroq.
- ^ Musazzi UM, Matera C, Dallanoce C, Vacondio F, De Amici M, Vistoli G va boshq. (2015 yil iyul). "Mahalliy terini og'riqsizlantirish uchun opioidni tanlash to'g'risida: Tarkibi va teri o'tkazuvchanligi munosabatlari". Xalqaro farmatsevtika jurnali. 489 (1–2): 177–85. doi:10.1016 / j.ijpharm.2015.04.071. PMID 25934430.
- ^ Le Naour M, Lunzer MM, Pauers MD, Kalyujniy AE, Benniuort MA, Tomas MJ, Portoghese PS (Avgust 2014). "Yomon ta'sirga ega bo'lmagan analjeziklarni ishlab chiqish maqsadi sifatida taxminiy kappa opioid heteromerlari". Tibbiy kimyo jurnali. 57 (15): 6383–92. doi:10.1021 / jm500159d. PMC 4136663. PMID 24978316.
- ^ DeWire SM, Yamashita DS, Rominger DH, Liu G, Cowan CL, Graczyk TM va boshq. (2013 yil mart). "M-opioid retseptoridagi G oqsiliga asoslangan ligand kuchli og'riq qoldiruvchi vositadir, morfin bilan taqqoslaganda oshqozon-ichak va nafas olish funktsiyalari pasaygan". Farmakologiya va eksperimental terapiya jurnali. 344 (3): 708–17. doi:10.1124 / jpet.112.201616. PMID 23300227. S2CID 8785003.
- ^ a b v Takayama H, Ishikava H, Kurihara M, Kitajima M, Aimi N, Ponglux D va boshq. (2002 yil aprel). "Mitraginin bilan bog'liq indol alkaloidlarining sintezi va opioid agonik faolligi bo'yicha tadqiqotlar: boshqa opioid ligandlardan tizimli ravishda farq qiluvchi opioid agonistlarini kashf etish". Tibbiy kimyo jurnali. 45 (9): 1949–56. doi:10.1021 / jm010576e. PMID 11960505.
- ^ a b v d e f g h men j k l m n o p q r s t siz v w x y z aa ab ak reklama ae af ag ah ai aj ak al am an Raynor K, Kong H, Chen Y, Yasuda K, Yu L, Bell GI, Reisine T (fevral 1994). "Klonlangan kappa-, delta- va mu-opioid retseptorlarining farmakologik tavsifi". Molekulyar farmakologiya. 45 (2): 330–4. PMID 8114680.
- ^ a b v d e f g Filizola M, Villar HO, Loew GH (2001 yil yanvar). "Delta, mu va kappa opioid retseptorlarini o'ziga xos bo'lmagan tanib olishning molekulyar determinantlari". Bioorganik va tibbiy kimyo. 9 (1): 69–76. doi:10.1016 / S0968-0896 (00) 00223-6. PMID 11197347.
- ^ a b v d e f g h Tam SW (fevral 1985). "(+) - [3H] SKF 10,047, (+) - [3H] etilketotsiklazosin, mu, kappa, delta va fenitsiklidin bilan bog'lanish joylari dengiz cho'chqasining miya membranalarida". Evropa farmakologiya jurnali. 109 (1): 33–41. doi:10.1016/0014-2999(85)90536-9. PMID 2986989.
- ^ a b v d e f g h men Corbett AD, Paterson SJ, Kosterlitz HW (1993). Opioidlar. Eksperimental farmakologiya bo'yicha qo'llanma Handbuch der Experimentellen Pharmakologie davomi. Eksperimental farmakologiya bo'yicha qo'llanma. 104 / 1. 645-679 betlar. doi:10.1007/978-3-642-77460-7_26. ISBN 978-3-642-77462-1. ISSN 0171-2004.
- ^ a b v d e f g h men j k l m n o p q r s Codd EE, Shank RP, Schupsky JJ, Raffa RB (sentyabr 1995). "Serotonin va norepinefrinni qabul qilish markazga ta'sir qiluvchi analjeziklarning faolligini inhibe qiladi: tizimli determinantlar va antinotsitsepsiyadagi roli". Farmakologiya va eksperimental terapiya jurnali. 274 (3): 1263–70. PMID 7562497.
- ^ Frink MC, Hennies HH, Englberger V, Haurand M, Wilffert B (1996 yil noyabr). "Tramadolning kalamush miyasining neyrotransmitter tizimiga ta'siri". Arzneimittel-Forschung. 46 (11): 1029–36. PMID 8955860.
- ^ Potschka H, Friderichs E, Lyösher V (sentyabr 2000). "Tramadol, uning enantiyomerlari va uning M1 metabolitining epilepsiya sichqonchani yoqish modelidagi antikonvulsant va prokonvulsant ta'siri". Britaniya farmakologiya jurnali. 131 (2): 203–12. doi:10.1038 / sj.bjp.0703562. PMC 1572317. PMID 10991912.
- ^ Katsumata S, Minami M, Nakagava T, Ivamura T, Satoh M (noyabr 1995). "Dihidroetorfinni klonlangan mu-, delta- va kappa-opioid retseptorlarida farmakologik o'rganish". Evropa farmakologiya jurnali. 291 (3): 367–73. doi:10.1016/0922-4106(95)90078-0. PMID 8719422.
- ^ Bart G, Schluger JH, Borg L, Ho A, Bidlack JM, Kreek MJ (dekabr 2005). "Oddiy odam ko'ngillilarida sarum prolaktin Nalmefen tomonidan ko'tarilgan: qisman kappa opioid agonist faoliyati?". Nöropsikofarmakologiya. 30 (12): 2254–62. doi:10.1038 / sj.npp.1300811. PMID 15988468.
- ^ Wentland MP, Lou R, Lu Q, Bu Y, VanAlstine MA, Cohen DJ, Bidlack JM (yanvar 2009). "Karboksamido bilan almashtirilgan opioidlarning sintezi va opioid retseptorlari bilan bog'lanish xususiyatlari". Bioorganik va tibbiy kimyo xatlari. 19 (1): 203–8. doi:10.1016 / j.bmcl.2008.10.134. PMID 19027293.
- ^ a b Garagozlou P, Demirci H, Devid Klark J, Lameh J (yanvar 2003). "Klonlangan mu opioid retseptorlarini ifodalaydigan hujayralardagi opioid ligandlarning faolligi". BMC farmakologiyasi. 3: 1. doi:10.1186/1471-2210-3-1. PMC 140036. PMID 12513698.Garagozlou P, Demirci H, Klark JD, Lameh J (Noyabr 2002). "Delta opioid retseptorlarini ifodalaydigan HEK hujayralaridagi opioid ligandlarning faollashuv rejimlari". BMC nevrologiyasi. 3: 19. doi:10.1186/1471-2202-3-19. PMC 137588. PMID 12437765.Gharagozlou P, Hashemi E, DeLorey TM, Clark JD, Lameh J (yanvar 2006). "Kappa opioid retseptorlari tarkibidagi opioid ligandlarning farmakologik profillari". BMC farmakologiyasi. 6: 3. doi:10.1186/1471-2210-6-3. PMC 1403760. PMID 16433932.
- ^ Rot BL, Baner K, Westkaemper R, Siebert D, Rays KC, Steinberg S va boshq. (2002 yil sentyabr). "Salvinorin A: kuchli tabiiy tarkibida bo'lgan azotli kappa opioid selektiv agonisti". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 99 (18): 11934–9. Bibcode:2002 yil PNAS ... 9911934R. doi:10.1073 / pnas.182234399. PMC 129372. PMID 12192085.
- ^ Wentland MP, Lou R, Lu Q, Bu Y, Denhardt C, Jin J va boshq. (2009 yil aprel). "Opioid retseptorlari uchun yuqori darajadagi yangi ligandlar sintezi". Bioorganik va tibbiy kimyo xatlari. 19 (8): 2289–94. doi:10.1016 / j.bmcl.2009.02.078. PMC 2791460. PMID 19282177.
- ^ Gassaway MM, Rives ML, Kruegel AC, Javitch JA, Sames D (iyul 2014). "Tianeptin atipik antidepressant va neyro-tiklovchi vosita m-opioid retseptorlari agonistidir". Tarjima psixiatriyasi. 4 (7): e411. doi:10.1038 / tp.2014.30. PMC 4119213. PMID 25026323.
- ^ "Mintaqalar va global miqyosda giyohvand moddalarni iste'mol qilishning yillik tarqalishi, 2016 yil". Jahon giyohvand moddalar bo'yicha hisoboti 2018. Birlashgan Millatlar Tashkilotining Giyohvand moddalar va jinoyatchilik bo'yicha boshqarmasi. 2018 yil. Olingan 7 iyul 2018.
- ^ Volkow ND. "Amerikaning opioidlarga qaramligi: geroin va retsept bo'yicha giyohvandlik". DrugAbuse.GOV. Giyohvandlik bo'yicha Milliy institut. Olingan 30 aprel 2017.
- ^ "Giyohvand moddalar Stupéfiants Estupefacientes" (PDF). Xalqaro Narkotik moddalarni boshqarish kengashi. 2012 yil. Olingan 6 mart 2017.
- ^ "Opioidni iste'mol qilish to'g'risidagi ma'lumotlar | Og'riq va siyosatni o'rganish guruhi". Painpolicy.wisc.edu. Olingan 7 yanvar 2016.
- ^ Dell CA, Roberts G, Kilty J, Taylor K, Daschuk M, Hopkins C, Dell D (2012). "Kanadadagi birinchi millatlar orasida giyohvand moddalarni suiste'mol qilish bo'yicha retsept bo'yicha tadqiqot: sog'liqni saqlashni mustahkamlash doirasidan". Moddani suiiste'mol qilish. 6: 23–31. doi:10.4137 / SART.S9247. PMC 3411531. PMID 22879752.
- ^ "Ijtimoiy kam ta'minlangan Ontariyaliklarga doimiy ravishda va Kanada ko'rsatmalaridan yuqori dozalarda opioidlar buyuriladi". Ices.on.ca. 2011 yil 25-yanvar. Olingan 7 yanvar 2016.
- ^ a b "Suiiste'mol qilmaslik, muvozanatga erishish: opioid sog'liqni saqlash inqiroziga qarshi kurash" (PDF). Ontario shifokorlari va jarrohlari kolleji. 8 sentyabr 2010. Arxivlangan asl nusxasi (PDF) 2016 yil 7-iyun kuni. Olingan 6 mart 2017.
- ^ Backhaus I, Mannocci A, La Torre G (2019). "Dori-darmonlarga asoslangan zararli bo'lmagan surunkali og'riqni davolashni iqtisodiy baholash tadqiqotlarini tizimli ko'rib chiqish". Amaldagi farmatsevtika biotexnologiyasi. 20 (11): 910–919. doi:10.2174/1389201020666190717095443. PMID 31322067.
- ^ Mojtabai R (2018 yil may). "Ortga nazar tashlab qo'yilgan opioidlardan uzoq muddatli foydalanishning milliy tendentsiyalari". Farmakoepidemiologiya va dori vositalari xavfsizligi. 27 (5): 526–534. doi:10.1002 / pds.4278. PMID 28879660. S2CID 19047621.
- ^ Manglik A, Kruse AC, Kobilka TS, Thian FS, Mathiesen JM, Sunahara RK va boshq. (2012 yil mart). "Morfinan antagonisti bilan bog'langan b-opioid retseptorlari kristalli tuzilishi". Tabiat. 485 (7398): 321–6. Bibcode:2012 yil natur.485..321M. doi:10.1038 / nature10954. PMC 3523197. PMID 22437502.
Afyun dunyodagi eng qadimgi dorilardan biri bo'lib, uning morfin va kodein hosilalari og'ir og'riqni engillashtiradigan eng ko'p ishlatiladigan klinik dorilar qatoriga kiradi.
- ^ Colledge S, Conolly J (2007 yil 10-avgust). Janubiy-g'arbiy Osiyo va Evropada mahalliy o'simliklarning kelib chiqishi va tarqalishi. Walnut Creek, CA: Chap sohil uchun matbuot. 179–181 betlar. ISBN 978-1598749885. Olingan 28 avgust 2018.
- ^ Kunzig R, Tsar J (2002 yil 1-noyabr). "La Marmotta". Kashf eting. Olingan 28 avgust 2018.
- ^ Chevalier A, Marinova E, Pena-Chocarro L (2014 yil 1-aprel). O'simliklar va odamlar: Vaqt o'tishi bilan tanlov va xilma-xillik. Oxbow kitoblari. 97–99 betlar. ISBN 978-1842175149. Olingan 28 avgust 2018.
- ^ Kritikos PG, Papadaki SP (1967). "Ko'knor va afyun tarixi va ularning qadimgi O'rta er dengizi mintaqasida kengayishi". Giyohvand moddalar to'g'risidagi xabarnoma. XIX (4). Olingan 23 avgust 2018.
- ^ Sonnedecker G (1962). "Opiat giyohvandligi kontseptsiyasining paydo bo'lishi". Journal Mondial de Pharmacie. 3: 275–290.
- ^ a b v d e f Braunshteyn MJ (iyun 1993). "Opiat, opioid peptidlar va opioid retseptorlarining qisqacha tarixi" (PDF). Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 90 (12): 5391–3. Bibcode:1993 PNAS ... 90.5391B. doi:10.1073 / pnas.90.12.5391. PMC 46725. PMID 8390660.
- ^ a b v d Duarte DF (2005 yil fevral). "Uma breve história do ópio e dos opióides" (PDF). Revista Brasileira de Anestesiologia. 55 (1). doi:10.1590 / S0034-70942005000100015.
- ^ Rosso AM (2010). "Qadimgi davrlarda ko'knori va afyun: chora yoki giyohvandlikmi?". Xalqaro biotibbiyot. 1: 81–87. CiteSeerX 10.1.1.846.221.
- ^ Astyrakaki E, Papaioannou A, Askitopoulou H (yanvar 2010). "Gippokrat to'plamidagi behushlik, og'riq va og'riq qoldiruvchi vositalar". Anesteziya va og'riqsizlantirish. 110 (1): 188–94. doi:10.1213 / ane.0b013e3181b188c2. PMID 19861359. S2CID 25919738.
- ^ Türe H, Türe U, Gögüs FY, Valavanis A, Yasargil MG (sentyabr 2006). "987 The Art of Alleviating Pain in Greek Mythology". European Journal of Pain (Abstracts of Pain in Europe V 5th Congress of the European Federation of IASP Chapters (EFIC)). 10 (S1): S255b–S255. doi:10.1016/S1090-3801(06)60990-7.
Sedare dolorem opus divinum est – an old Latin inscription – means "alleviating pain is the work of the divine". This inscription is often attributed to either Hippocrates of Kos or Galen of Pergamum, but it is most likely an anonymous proverb
- ^ Osbaldeston TA (2000). Dioscorides (translation). Johannesburg, South Africa: Ibidis Press. pp. 607–611. ISBN 978-0-620-23435-1.
- ^ Heydari M, Hashempur MH, Zargaran A (2013). "Medicinal aspects of opium as described in Avicenna's Canon of Medicine". Acta Medico-Historica Adriatica. 11 (1): 101–12. PMID 23883087.
- ^ a b v Asthana SN (1954). "The Cultivation of the Opium Poppy in India". Giyohvand moddalar to'g'risidagi xabarnoma (3). Olingan 5 sentyabr 2018.
- ^ a b v Sigerist HE (1941). "Laudanum Paracelsus asarlarida" (PDF). Buqa. Tarix. Med. 9: 530–544. Olingan 5 sentyabr 2018.
- ^ a b v d e Hamilton GR, Baskett TF (April 2000). "In the arms of Morpheus the development of morphine for postoperative pain relief". Kanadalik behushlik jurnali. 47 (4): 367–74. doi:10.1007/BF03020955. PMID 10764185.
- ^ a b Farooqui A (December 2016). "The Global Career of Indian Opium and Local Destinies" (PDF). Almanack (14): 52–73. doi:10.1590/2236-463320161404. Olingan 5 sentyabr 2018.
- ^ a b Deming S (2011). "The Economic Importance of Indian Opium and Trade with China on Britain's Economy, 1843–1890" (PDF). Economic Working Papers. 25 (Bahor). Olingan 5 sentyabr 2018.
- ^ a b v d e f g h men j k Rinde M (2018). "Opioidlarning halokatli qaytishi". Distillashlar. 4 (2): 12–23. Olingan 23 avgust 2018.
- ^ Mills JH (2016). Review of 'Opium and Empire in Southeast Asia: Regulating Consumption in British Burma'. Tarixdagi sharhlar. Cambridge imperial and post-colonial studies series. Palgrave Makmillan. doi:10.14296/RiH/2014/2010. ISBN 9780230296466. Olingan 5 sentyabr 2018.
- ^ Krishnamurti C, Rao SC (November 2016). "The isolation of morphine by Serturner". Hindistonning behushlik jurnali. 60 (11): 861–862. doi:10.4103/0019-5049.193696. PMC 5125194. PMID 27942064.
- ^ Courtwright DT (2009). Forces of habit drugs and the making of the modern world (1 nashr). Kembrij, Mass.: Garvard universiteti matbuoti. 36-37 betlar. ISBN 9780674029903.
- ^ Atanasov AG, Waltenberger B, Pferschy-Wenzig EM, Linder T, Wawrosch C, Uhrin P, et al. (Dekabr 2015). "Discovery and resupply of pharmacologically active plant-derived natural products: A review". Biotexnologiya yutuqlari. 33 (8): 1582–1614. doi:10.1016/j.biotechadv.2015.08.001. PMC 4748402. PMID 26281720.
- ^ Kotwal A (March 2005). "Innovation, diffusion and safety of a medical technology: a review of the literature on injection practices". Ijtimoiy fan va tibbiyot. 60 (5): 1133–47. doi:10.1016/j.socscimed.2004.06.044. PMID 15589680.
- ^ Mosher CJ (2013). Drugs and Drug Policy: The Control of Consciousness Alteration. SAGE nashrlari. p. 123. ISBN 9781483321882.
- ^ Fisher GL (2009). Encyclopedia of substance abuse prevention, treatment, & recovery. Los-Anjeles: SAGE. p. 564. ISBN 9781452266015.
- ^ a b Trickey E (4 January 2018). "Inside the Story of America's 19th-Century Opiate Addiction". Smithsonian. Olingan 6 sentyabr 2018.
- ^ Schechter NL (1993). Pain in Infants, Children, and Adolescents. Uilyams va Uilkins. ISBN 9780683075885. Olingan 6 sentyabr 2018.
- ^ Hicks RD (2011). "Frontline Pharmacies". Kimyoviy meros jurnali. Kimyoviy meros jamg'armasi. Olingan 29 oktyabr 2018.
- ^ a b Booth M (12 June 1999). Opium : a history (1-AQSh nashri). Sent-Martin matbuoti. ISBN 978-0312206673.
- ^ Wisniak J (March 2013). "Pierre-Jean Robiquet". Educación Química. 24: 139–149. doi:10.1016/S0187-893X(13)72507-2. Olingan 9-noyabr 2019.
- ^ Filan K (2011). The power of the poppy : harnessing nature's most dangerous plant ally. Park Street Press. p. 69. ISBN 9781594773990. Olingan 30 oktyabr 2018.
- ^ "Felix Hoffmann". Fan tarixi instituti. 2016 yil iyun. Olingan 21 mart 2018.
- ^ Cooper R, Deakin JJ (22 February 2016). Botanika mo''jizalari: dunyoni o'zgartirgan o'simliklar kimyosi. CRC Press. p. 137. ISBN 9781498704281.
- ^ Sneader W (November 1998). "Geroin topildi" (PDF). Lanset. 352 (9141): 1697–9. doi:10.1016 / S0140-6736 (98) 07115-3. PMID 9853457. S2CID 1819676.
Bayer geroin ismini 1898 yil iyun oyida ro'yxatdan o'tkazdi.
- ^ a b v d e Newton DE (2016). Youth substance abuse : a reference handbook. Santa Barbara, Kaliforniya: ABC-CLIO. 41-60 betlar. ISBN 9781440839832. Olingan 30 oktyabr 2018.
- ^ Crow JM (3 January 2017). "Addicted to the cure". Kimyo olami. Olingan 30 oktyabr 2018.
- ^ Metadon masalalari: Opiat giyohvandligini rivojlanayotgan jamoat metadon davolash. CRC Press. 2003. p. 13. ISBN 9780203633090. Arxivlandi asl nusxasidan 2015 yil 23 dekabrda.
- ^ "Fact Sheet: Fentanyl and Synthetic Opioids" (PDF). Giyohvand moddalar siyosati alyansi. 2016 yil sentyabr. Olingan 30 oktyabr 2018.
- ^ "Laws Learn about the laws concerning opioids from the 1800s until today". The National Alliance of Advocates for Buprenorphine Treatment. Olingan 30 oktyabr 2018.
- ^ White WL. "The Early Criminalization of Narcotic Addiction" (PDF). William White Papers. Olingan 30 oktyabr 2018.
- ^ Mars S (2003). "Peer pressure and imposed consensus: the making of the 1984 Guidelines of Good Clinical Practice in the Treatment of Drug Misuse". Clio Medica. 75 (2): 149–83. doi:10.1258/jrsm.96.2.99. PMC 539406. PMID 16212730.
- ^ a b Jacobs H (26 May 2016). "This one-paragraph letter may have launched the opioid epidemic". Business Insider. Olingan 30 oktyabr 2018.
- ^ Portenoy RK, Foley KM (May 1986). "Chronic use of opioid analgesics in non-malignant pain: report of 38 cases". Og'riq. 25 (2): 171–86. doi:10.1016/0304-3959(86)90091-6. PMID 2873550. S2CID 23959703.
- ^ a b v Meldrum ML (August 2016). "The Ongoing Opioid Prescription Epidemic: Historical Context". Amerika sog'liqni saqlash jurnali. 106 (8): 1365–6. doi:10.2105/AJPH.2016.303297. PMC 4940677. PMID 27400351.
- ^ Quinones S (2015). Dreamland : the true tale of America's opiate epidemic. Bloomsbury Press. ISBN 9781620402511.
- ^ Dowell D, Haegerich TM, Chou R (March 2016). "CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016". MMWR. Tavsiyalar va hisobotlar. 65 (1): 1–49. doi:10.15585/mmwr.rr6501e1. PMID 26987082.
- ^ FDA launches public education campaign to encourage safe removal of unused opioid pain medicines from homes, PM FDA 25 April 2019, retrieved 10 May 2019
- ^ "opioid: definition of opioid in Oxford dictionary (American English) (US)". www.oxforddictionaries.com. Olingan 14 fevral 2016.
Opioid: 1950s: from opium + -oid.
- ^ Wikler A, Martin WR, Pescor FT, Eades CG (October 1963). "Factors regulating oral consumption of an opioid (Etonitazene) by morphine-addicted rats". Psixofarmakologiya. 5: 55–76. doi:10.1007/bf00405575. PMID 14082382. S2CID 38073529.
In this paper, the term, 'opioid', is used in the sense originally proposed by DR. GEORGE H. ACHESON (personal communication) to refer to any chemical compound with morphine-like activities.
- ^ Martin WR (1967 yil dekabr). "Opioid antagonists". Farmakologik sharhlar. 19 (4): 463–521. PMID 4867058.
- ^ Mehdi B (2008). "Opioid analgesics and antagonists". In Seth SD, Seth V (eds.). Textbook of Pharmacology. Elsevier India. p. III.137. ISBN 9788131211588.
- ^ "Epidemic: Responding to America's Prescription Drug Abuse Crisis" (PDF). Oq uy. 2011. Arxivlangan asl nusxasi (PDF) 2012 yil 3 martda.
- ^ "First Do No Harm: Responding to Canada's Prescription Drug Crisis" (PDF). 2013 yil mart. Olingan 8 mart 2017.
- ^ "UK: Task Force offers ideas for opioid addiction solutions". Delhidailynews.com. 11 Iyun 2014. Arxivlangan asl nusxasi 2017 yil 6-iyun kuni. Olingan 7 yanvar 2016.
- ^ Kite A (29 April 2018). "Every state but Missouri has opioid drug tracking. Why are senators against it?". Kansas City Star. Olingan 5 noyabr 2018.
- ^ Rutkow L, Turner L, Lucas E, Hwang C, Alexander GC (March 2015). "Most primary care physicians are aware of prescription drug monitoring programs, but many find the data difficult to access". Sog'liqni saqlash. 34 (3): 484–92. doi:10.1377/hlthaff.2014.1085. PMID 25732500.
- ^ Perrone M (20 December 2015). "Painkiller politics: Effort to curb prescribing under fire". Associated Press. Philly.com. Olingan 7 yanvar 2016.
- ^ Von Korff M, Dublin S, Walker RL, Parchman M, Shortreed SM, Hansen RN, Saunders K (January 2016). "The Impact of Opioid Risk Reduction Initiatives on High-Dose Opioid Prescribing for Patients on Chronic Opioid Therapy". Og'riq jurnali. 17 (1): 101–10. doi:10.1016/j.jpain.2015.10.002. PMC 4698093. PMID 26476264.
- ^ Achenbach J, Wagner J, Bernstein L. "Trump says opioid crisis is a national emergency, pledges more money and attention". Vashington Post. Olingan 11 avgust 2017.
- ^ "Feasibility Study on Opium Licensing in Afghanistan for the Production of Morphine and Other Essential Medicines". ICoS. 2005 yil sentyabr.
- ^ "Assuring Availability of Opioid Analgesics" (PDF). Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasi (PDF) 2009 yil 1 dekabrda.
- ^ Ghelardini C, Di Cesare Mannelli L, Bianchi E (2015). "The pharmacological basis of opioids". Clinical Cases in Mineral and Bone Metabolism. 12 (3): 219–21. doi:10.11138/ccmbm/2015.12.3.219. PMC 4708964. PMID 26811699.
The opioid effects transcending analgesia include sedation, respiratory depression, constipation and a strong sense of euphoria.
- ^ Barrett SP, Meisner JR, Stewart SH (November 2008). "What constitutes prescription drug misuse? Problems and pitfalls of current conceptualizations" (PDF). Giyohvand moddalarni suiste'mol qilish bo'yicha hozirgi sharhlar. 1 (3): 255–62. doi:10.2174/1874473710801030255. PMID 19630724. Arxivlandi asl nusxasi (PDF) 2010 yil 15 iyunda.
- ^ McCabe SE, Boyd CJ, Teter CJ (June 2009). "Subtypes of nonmedical prescription drug misuse". Giyohvandlik va alkogolga qaramlik. 102 (1–3): 63–70. doi:10.1016/j.drugalcdep.2009.01.007. PMC 2975029. PMID 19278795.
- ^ "Prescription Opioid Overdose Data | Drug Overdose | CDC Injury Center". www.cdc.gov. 31 avgust 2018 yil. Olingan 17 yanvar 2017.
- ^ Rot, Bryan L.; Baner, Karen; Westkaemper, Richard; Siebert, Daniel; Rice, Kenner C.; Shtaynberg, SeAnna; Ernsberger, Pol; Rothman, Richard B. (3 September 2002). "Salvinorin A: A potent naturally occurring nonnitrogenous κ opioid selective agonist". Amerika Qo'shma Shtatlari Milliy Fanlar Akademiyasi materiallari. 99 (18): 11934–11939. Bibcode:2002PNAS...9911934R. doi:10.1073/pnas.182234399. ISSN 0027-8424. PMC 129372. PMID 12192085.
- ^ "Esters of Morphine". Birlashgan Millatlar Tashkilotining Giyohvand moddalar va jinoyatchilik bo'yicha boshqarmasi. 1953. Olingan 10 mart 2012.
- ^ "Esters of Morphine Opioids". eOpiates. 2014 yil 28-may. Olingan 12 fevral 2016.[doimiy o'lik havola ]
- ^ Raffa RB, Buschmann H, Christoph T, Eichenbaum G, Englberger W, Flores CM, et al. (2012 yil iyul). "Mechanistic and functional differentiation of tapentadol and tramadol". Farmakoterapiya bo'yicha mutaxassislarning fikri. 13 (10): 1437–49. doi:10.1517/14656566.2012.696097. PMID 22698264. S2CID 24226747.
- ^ Rojas-Corrales MO, Gibert-Rahola J, Micó JA (1998). "Tramadol induces antidepressant-type effects in mice". Hayot fanlari. 63 (12): PL175-80. doi:10.1016/S0024-3205(98)00369-5. PMID 9749830.
- ^ Stein C, Schäfer M, Machelska H (August 2003). "Attacking pain at its source: new perspectives on opioids". Tabiat tibbiyoti. 9 (8): 1003–8. doi:10.1038/nm908. PMID 12894165. S2CID 25453057.
- ^ Stein C, Lang LJ (February 2009). "Peripheral mechanisms of opioid analgesia". Farmakologiyadagi hozirgi fikr. 9 (1): 3–8. doi:10.1016/j.coph.2008.12.009. PMID 19157985.
- ^ Busch-Dienstfertig M, Stein C (July 2010). "Opioid receptors and opioid peptide-producing leukocytes in inflammatory pain--basic and therapeutic aspects". Miya, o'zini tutish va immunitet. 24 (5): 683–94. doi:10.1016/j.bbi.2009.10.013. PMID 19879349. S2CID 40205179.
- ^ Odell LR, Skopec J, Makkluski A (mart 2008). "Isolation and identification of unique marker compounds from the Tasmanian poppy Papaver somniferum N. Implications for the identification of illicit heroin of Tasmanian origin". Xalqaro sud ekspertizasi. 175 (2–3): 202–8. doi:10.1016 / j.forsciint.2007.07.002. PMID 17765420.
Tashqi havolalar
- Opioid Withdrawal Symptoms —Information about Opioid and opiate withdrawal issues
- World Health Organization guidelines for the availability and accessibility of controlled substances
- CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016
- Reference list to the previous publication
- Links to all language versions of the previous publication
- Video: Opioid side effects (Vimeo) (YouTube) —A short educational film about the practical management of opioid side effects.