O'z joniga qasd qilishga yordam berish - Assisted suicide
| O'z joniga qasd qilish |
|---|
O'z joniga qasd qilishga yordam berish, shuningdek, nomi bilan tanilgan o'lishga yordam berdi, bo'ladi o'z joniga qasd qilish boshqa odam yordamida amalga oshiriladi.[1] Bu atama odatda quyidagilarni anglatadi shifokorning yordami bilan o'z joniga qasd qilish (PAS) yordam beradi, bu o'z joniga qasd qilish shifokor yoki boshqa tibbiy yordam ko'rsatuvchi. Shaxsning ahvoli shu joy uchun o'z joniga qasd qilish to'g'risidagi qonunlar bo'yicha shifokorga tegishli ekanligi aniqlangandan so'ng, shifokorning yordami odatda yozish bilan cheklanadi retsept o'ldiradigan dozada dorilar uchun.
Ko'pgina yurisdiktsiyalarda odamning o'z joniga qasd qilishda o'lishiga yordam berish a jinoyat.[2] O'z joniga qasd qilishni vrachlar tomonidan qonuniylashtirilishini qo'llab-quvvatlovchi odamlar, o'z ixtiyori bilan o'limga yordam bergan odamlarni jinoiy ta'qibdan ozod qilishni istaydilar. qotillik yoki shunga o'xshash jinoyatlar. Shifokorlar yordami bilan o'z joniga qasd qilish ba'zi mamlakatlarda, ma'lum sharoitlarda, shu jumladan qonuniydir Kanada, Belgiya, Gollandiya, Lyuksemburg, Kolumbiya, Shveytsariya va Qo'shma Shtatlarning qismlari va Avstraliya (Viktoriya).[3] Ushbu shtatlarning yoki mamlakatlarning aksariyatida yuridik yordam olish uchun shifokor yordami bilan o'z joniga qasd qilishni istagan shaxslar ma'lum mezonlarga, shu jumladan o'lik kasallik, ular ekanligini isbotlash sog'lom aql, ixtiyoriy ravishda va o'lishni xohlashlarini bir necha bor bildirish va o'ldiradigan o'ldiradigan dozani o'zlari qabul qilish.
Terminologiya

O'z joniga qasd qilish bu o'zini o'ldirish harakati. O'z joniga qasd qilishga yordam berish bu boshqa shaxsning o'z joniga qasd qilishda o'lishiga, masalan, asbob-uskunalar yoki jihozlar bilan ta'minlash kabi moddiy yordam berishidir Shifokor yordami bilan o'z joniga qasd qilish shifokorni (shifokorni) "bila turib va qasddan odamga o'z joniga qasd qilish uchun zarur bo'lgan bilim yoki vositalarni yoki ikkalasini berishni, shu jumladan o'ldiradigan dori dozalari to'g'risida maslahat berishni, bunday o'ldiradigan dozalarni tayinlashni yoki dori-darmonlarni etkazib berishni o'z ichiga oladi".[5]
O'z joniga qasd qilish yordami bilan farqlanadi Evtanaziya, ba'zan deb nomlanadi rahmdillik bilan o'ldirish, bu erda o'layotgan odam to'g'ridan-to'g'ri o'z o'limiga olib kelmaydi, balki odamni keyingi azoblarni boshdan kechirish uchun o'ldiriladi. Evtanaziya yoki bo'lmasdan sodir bo'lishi mumkin rozilik, va ixtiyoriy, ixtiyoriy yoki majburiy bo'lmagan deb tasniflanishi mumkin. Azob chekayotgan va rozi bo'lgan odamni o'ldirish deyiladi ixtiyoriy evtanaziya. Bu hozirda ba'zi hududlarda qonuniy.[6] Agar shaxs rozilik berolmasa, u shunday deb nomlanadi ixtiyoriy bo'lmagan evtanaziya. O'lishni istamaydigan yoki rozilik berishga qodir bo'lgan va roziligi so'ralmagan odamni o'ldirish jinoyat hisoblanadi. beixtiyor evtanaziya va qotillik sifatida qaralmoqda.
O'lim huquqi odamlar o'z joniga qasd qilish, evtanaziya yoki hayotni saqlab qoladigan tibbiy muolajadan bosh tortish orqali o'lishga haqli ekanligiga ishonishdir.
O'z joniga qasd qilishga yordam berish
O'z joniga qasd qilishning ba'zi himoyachilari, shifokorlar yordami bilan o'z joniga qasd qilish to'g'risida gap ketganda, "yordam bilan o'z joniga qasd qilish" va "o'z joniga qasd qilish" so'zlariga qarshi turishadi va "yordam berish bilan o'lish" iborasini afzal ko'rishadi. Buning sababi, munozarani tez-tez kasal bo'lmagan va yordam olish huquqiga ega bo'lmagan shaxslar tomonidan amalga oshirilgan o'z joniga qasd qilishdan uzoqlashtirishdir. Ularning fikricha, ushbu holatlar "o'z joniga qasd qilish" so'ziga shu qadar salbiy ta'sir ko'rsatdiki, bu jabr ko'rgan odam tinch o'limni qidirib topgan vaziyatga hech qanday aloqasi yo'q.[7][8]
Shifokor yordami bilan o'z joniga qasd qilish
Qo'llab-quvvatlash
Uchun argumentlar
Yordam bilan o'limni qo'llab-quvvatlovchi dalillarga bemorlarning avtonomiyasini hurmat qilish, o'lik bemorlarga hayotni qo'llab-quvvatlashda va tashqarida teng munosabatda bo'lish, rahm-shafqat, shaxsiy erkinlik va oshkoralik kiradi.[9] Agar o'lim yaqinlashganda (yarim yil yoki undan kam) bemorlar o'limga yordam berish usulini tanlashlari mumkin, chunki u odamning chidab bo'lmas o'lim jarayoni deb bilishini qisqartirishi mumkin. Og'riq, asosan, shifokorning yordami bilan o'z joniga qasd qilishni izlashning asosiy sababi sifatida qayd etilmaydi. Qo'shma Shtatlarda;[3] Oregon shtati aholisi tomonidan 2015 yilda "Qadr bilan o'lim" to'g'risidagi qonundan foydalangan holda tez-tez aytib o'tilgan uchta hayotiy muammolar quyidagilar: hayotni zavqlantiradigan tadbirlarda qatnashish qobiliyatining pasayishi (96,2%), yo'qotish muxtoriyat (92,4%) va yo'qotish qadr-qimmat (75.4%).[10]
Oregon statistikasi
Oregon shtatidagi xospis opa-singillari va ijtimoiy ishchilarni o'rganish shuni ko'rsatdiki, barbituratlar uchun o'ldiradigan retsept so'ramagan xospis bemorlari orasida og'riq, depressiya, xavotir, haddan tashqari ochlik va o'lish jarayonidan qo'rqish alomatlari ko'proq sezilgan. shifokor o'limga yordam berdi.[11]
Xospisdan foydalanish tartibi to'g'risidagi palliativ tibbiyot jurnalining hisobotida ta'kidlanishicha, Oregon xospisdan foydalanishning eng yuqori kvartilida ham, xospisdan foydalanishning eng past kvartilida ham bo'lgan. Xuddi shunday tendentsiya Vermontda ham topilgan, u erda 2013 yilda o'lishga yordam berish huquqi berilgan (AiD).[12]
2016 yil fevral oyida Oregon shtati 2015 yilgi raqamlari to'g'risida hisobot chiqardi. 2015 yil davomida shtatda 218 kishi bor edi, ular o'z hayotlarini tugatish uchun o'limga olib keladigan dorilarni qabul qilishdi va qabul qilishdi. Ushbu 218 kishidan 132 o'ta xavfli bemor oxir-oqibat giyohvand moddalarni iste'mol qilish to'g'risida qaror qabul qildi va natijada ularning o'limi yuz berdi. Oregon shtatidagi sog'liqni saqlash bo'limining so'roviga ko'ra, ishtirokchilarning aksariyati, 78% 65 yoshdan katta va asosan Kavkaz, 93,1%. O'z hayotini tugatishni tanlagan o'lik kasallarning 72 foizida saraton kasalligi aniqlangan. Oregon shtatining 2015 yilgi so'rovida ular o'lim paytida tibbiy yordam ko'rsatishda davolanadigan kasallardan, hayotni tugatish bilan bog'liq eng katta tashvishlar nima ekanligini so'rashdi: ushbu odamlarning 96,2 foizi bir vaqtlar o'tkazilgan tadbirlarda ishtirok etish qobiliyatini yo'qotganligini eslatib o'tdilar. ularni hayotdan zavqlantirdi, 92,4% avtonomiyani yo'qotish yoki o'zlarining fikrlari yoki harakatlaridan mustaqilligini va 75,4% o'z qadr-qimmatini yo'qotishini ta'kidladilar.[13]
Vashington shtati statistikasi
Vashingtonda shifokorlar buyurgan o'ldiradigan dori-darmonlarni iste'mol qilish natijasida kelib chiqadigan o'limning o'sish tendentsiyasi qayd etilgan: 2009 yilda 64 o'limdan 2015 yilda 202 o'limga qadar.[14] O'lganlar orasida 72% terminal saratonga, 8% neyrodejenerativ kasalliklarga chalingan (shu jumladan ALS).[14]
AQSh so'rovnomalari
1947 yildan beri Gallup tomonidan o'tkazilgan so'rovnomalar, "Agar odam davolanmaydigan kasallikka chalinganida, bemor va uning oilasi talab qilsa, shifokorlarga bemorning hayotini qandaydir og'riqsiz vositalar bilan tugatishga ruxsat berish kerak deb o'ylaysizmi?" 1947 yildagi 37 foizdan taxminan 1990 yildan 2005 yilgacha davom etadigan taxminan 75 foizli platoga ko'tarilgan amaliyotni qo'llab-quvvatlashni namoyish eting. Ovoz berish savoli shu tarzda o'zgartirilganda, davolanib bo'lmaydigan kasallikdan farqli o'laroq, "qattiq og'riq" paydo bo'ldi, "qonuniylashtirish" "shifokorlar tomonidan amalga oshirilgan ixtiyoriy evtanaziya o'rniga, odatda shifokorlarga ruxsat berishdan va" bemorning o'z joniga qasd qilishidan "farqli o'laroq, jamoatchilik ko'magi sezilarli darajada pastroq bo'lib, taxminan 10-15% gacha bo'lgan.[3]
National Journal and Regence Foundation tomonidan o'tkazilgan so'rov natijalariga ko'ra, oregonliklar ham, vashingtonliklar ham "umrini tugatish" terminologiyasini mamlakatning qolgan qismiga qaraganda ko'proq yaxshi bilishgan va har ikkala shtat aholisi palliativ va xospis atamalarini biroz ko'proq bilishadi. g'amxo'rlik.[15]
"Palliativ tibbiyot" jurnalidan o'tkazilgan so'rov natijalariga ko'ra, o'limni yordamni tanlagan bemorlarning oilaviy yordamchilari bemorga g'amxo'rlik qilishda ijobiy ma'noga ega bo'lishlari va bemorning o'limini qabul qilishga tayyor bo'lishlarini so'ramagan bemorlarning oilaviy tarbiyachilariga qaraganda ko'proq ekanligi aniqlandi. o'limga yordam berdi.[16]
Xavfsizlik choralari
Amaldagi ko'plab o'lim qonunlarida suiiste'mol qilinishni oldini olish uchun nazorat va tergov jarayonlarini ta'minlashga qaratilgan qoidalar mavjud. Bunga muvofiqlik va malakaviy jarayonlar, tibbiy guruh tomonidan majburiy davlat hisoboti va tibbiy kengash nazorati kiradi. Oregon va boshqa shtatlarda, ikkita shifokor va ikkita guvoh, odamning o'ldiradigan retsepti bo'yicha so'rovi majburlanmagan yoki asossiz ta'sir ostida emasligini tasdiqlashlari kerak.
Ushbu kafolatlar orasida yashash va yashash huquqini tasdiqlash kiradi. Bemor ikkita shifokor bilan uchrashishi kerak va ular davom ettirishdan oldin ular tashxislarni tasdiqlashlari kerak; ba'zi hollarda, ular bemorning o'zi qaror qabul qiladimi yoki yo'qligini aniqlash uchun ular psixiatrik baholashni ham o'z ichiga oladi. Keyingi qadamlar - ikkita og'zaki so'rov, keyingi so'rovni yuborishdan oldin kamida 15 kun kutish muddati. Ikki xil odam guvoh bo'lishi kerak bo'lgan yozma so'rov, ulardan biri oila a'zosi bo'la olmaydi, so'ngra bemorning shifokori yana bir kutish davri o'tkaziladi, unda ular giyohvand moddalarni iste'mol qilish huquqiga egami yoki yo'qmi ("Qadr bilan o'lim") .
Ushbu kafolatlar ish beradimi-yo'qligi haqidagi bahslar muxoliflar va tarafdorlar o'rtasida muhokama qilinadi.
Diniy pozitsiyalar
Unitar universalizm
1988 yildagi umumiy qarorga binoan "Unitar universalistlar o'lim holatida o'z taqdirini o'zi belgilash huquqini himoya qilish va tegishli xavfsizlik choralari bilan kasal bo'lgan bemorlarning o'z o'lim vaqtini tanlash huquqini hurmat qilish uchun harakat qilganlarni fuqarolik yoki jinoiy jazodan ozod qilish.[17]
Qarama-qarshilik
Tibbiy axloq
Axloq qoidalari
Ning eng so'nggi versiyasi Amerika tibbiyot assotsiatsiyasi Axloq kodeksida shifokor yordami bilan o'z joniga qasd qilish taqiqlangan. Bu shifokor yordami bilan o'z joniga qasd qilishni taqiqlaydi, chunki u "shifokorning davolovchi roliga mutlaqo mos kelmaydi" va uni "nazorat qilish qiyin yoki imkonsiz bo'lib, jiddiy ijtimoiy xavf tug'dirishi mumkin".[18]
Gippokrat qasamyodi
Ba'zi shifokorlar[19] shifokor yordami bilan o'z joniga qasd qilishning aksi ekanligini eslatib qo'ying Gippokrat qasamyodi, bu tarixiy ravishda shifokorlar tomonidan berilgan qasam. Unda "agar so'ralsa, men hech kimga o'lik dori berolmayman va bunday maslahat bermayman" deb yozilgan.[20][21] Ammo asl qasamyod ko'p marotaba o'zgartirilgan va ommabop e'tiqodga xilof ravishda, aksariyat zamonaviy tibbiyot maktablari tomonidan talab qilinmaydi va uni qabul qilmoqchi bo'lgan shaxslarga hech qanday qonuniy majburiyatlar yuklanmaydi.[22] Bugungi kunda odatdagi abort kabi Gippokrat qasamyodi tomonidan taqiqlangan protseduralar mavjud.[23]
Jeneva deklaratsiyasi
The Jeneva deklaratsiyasi tomonidan 1948 yilda tuzilgan Gippokrat qasamyodining qayta ko'rib chiqilishi Jahon tibbiyot birlashmasi amalga oshirilgan majburiy (majburiy bo'lmagan) evtanaziya, evgenika va boshqa tibbiy jinoyatlarga javoban Natsistlar Germaniyasi. Unda "Men inson hayotiga bo'lgan hurmatimni saqlab qolaman" degan so'zlar mavjud.[24]
Xalqaro tibbiy axloq kodeksi
The Xalqaro tibbiy axloq kodeksi, oxirgi marta 2006 yilda qayta ko'rib chiqilgan "Shifokorlar bemorlar oldidagi vazifalari" bo'limiga "Shifokor har doim inson hayotini hurmat qilish majburiyatini yodda tutishi kerak" kiradi.[25]
Marbellaning bayonoti
Marbella bayonoti 1992 yilda Ispaniyaning Marbella shahrida bo'lib o'tgan 44-Butunjahon tibbiyot assambleyasi tomonidan qabul qilingan bo'lib, unda "shifokorlar yordami bilan o'z joniga qasd qilish, ixtiyoriy evtanaziya singari, axloqqa zid va tibbiyot tomonidan mahkum etilishi kerak".[26]
Surunkali kasalliklarga chalingan odamlarga kengayish xavotirlari
PASga qarshi bo'lgan sog'liqni saqlash sohasi mutaxassislari orasida tashvish, bu protsedura aholining zaif qatlamlariga ta'sir qilishi mumkin. Ushbu dalil "nomi bilan tanilgansilliq qiyalik ".[27] Ushbu dalil o'ta xavfli kasallar uchun PAS tashkil etilgandan so'ng, u boshqa zaif jamoalarga, ya'ni nogironlarga o'tadi va demografik yoki ijtimoiy-iqtisodiy holatiga qarab o'zini kamroq munosib his qiladiganlar foydalanishi mumkin degan xavotirni o'z ichiga oladi. Bundan tashqari, aholining zaif qatlamlari bevaqt o'lim xavfiga ko'proq duch kelishadi, chunki "bemorlar ularning haqiqiy roziligisiz PASga duchor bo'lishlari mumkin".[28]
Diniy pozitsiyalar
Katoliklik
Rim-katolik cherkovi inson hayotiga oid axloqiy qarorlar o'z vijdoniga va e'tiqodiga qarab qabul qilinishi kerakligini tan oladi.[29] Katolik urf-odatlarida aytilishicha, birovning azoblanishidan xavotirlanish ixtiyoriy evtanaziya bilan harakat qilish maqsadga muvofiqligini hal qilish uchun etarli sabab emas. Ga ko'ra Katolik cherkovining katexizmi, "Xudo barcha hayotning yaratuvchisi va muallifidir." Ushbu e'tiqod tizimida Xudo inson hayotini yaratgan, shuning uchun Xudo hayotni qachon tugatishiga hakamdir.[29] Rim-katolik cherkovi nuqtai nazaridan, o'z hayotini yoki boshqasining hayotini ataylab tugatish axloqan noto'g'ri va katolik ta'limotiga qarshi chiqadi. Bundan tashqari, o'z hayotini tugatish, u odamni va uning yaqinlarini hayotda qolgan vaqtdan mahrum qiladi va qolganlar uchun ulkan qayg'u va qayg'uga sabab bo'ladi.[30]
Papa Frensis[31] katolik cherkovining hozirgi hukmron shaxsidir. U o'lim ulug'vor voqea ekanligini va uni Xudodan boshqa hech kim hal qilmasligi kerakligini tasdiqlaydi. Papa Frensis hayotni himoya qilish uning muqaddasligini himoya qilishni anglatadi, deb ta'kidlamoqda.[32] Rim-katolik cherkovi o'z izdoshlariga evtanaziyani qabul qilish mumkin emasligini o'rgatadi, chunki bu gunoh sifatida qabul qilinadi, chunki bu o'nta amrga ziddir, "Siz o'ldirmang. (Siz o'ldirmaysiz)" Beshinchi amrga binoan, o'z joniga qasd qilish harakati inson hayotining qadr-qimmatiga va Xudoga bo'lgan hurmatiga ziddir.[33]
Katolik cherkovi vrachlar yordami bilan o'z joniga qasd qilishning alternativi sifatida va og'riqni engillashtirish maqsadida, kasal bo'lgan bemorlarga o'zlarining oilalari va tarbiyachilarining mehri va rahm-shafqatini olayotganda din va Yaratgan bilan tinchlik o'rnatishga e'tibor berishni taklif qiladi.[30] Bundan tashqari, Rim-katolik cherkovi o'lik kasallarga o'z joniga qasd qilish o'rniga, psixologik va ma'naviy azoblarni davolash paytida jismoniy og'riq bilan shug'ullanadigan palyativ yordam ko'rsatishni tavsiya qiladi.[34]
Yahudiylik
Hayotni saqlab qolish - bu eng katta qadriyatlardan biri Yahudiylik, o'z joniga qasd qilish va o'z joniga qasd qilish holatlari paydo bo'lishi Injil va Rabbin adabiyoti.[35] O'rta asr hokimiyati ushbu choralarning qonuniyligi va qanday cheklangan sharoitlarda qo'llanilishi mumkinligi haqida bahslashmoqda. Keyinchalik yahudiylik dinidagi qabul qilingan me'yoriy amaliyotning aksariyat ravvinlar hokimiyatining xulosasi shuki, o'z joniga qasd qilish va o'z joniga qasd qilishga o'z joniga qasd qilish xatti-harakatlari hatto davolanib bo'lmaydigan og'riq bilan jazolanishi mumkin emas.[36]
Oxirgi kun avliyolari Iso Masihning cherkovi
Oxirgi kun avliyolari Iso Masihning cherkovi (LDS cherkovi) evtanaziyaga qarshi. Evtanaziyada, jumladan, "o'z joniga qasd qilishda" ishtirok etgan har bir kishi, Xudoning amrlarini buzgan deb hisoblanadi.[37] Ammo cherkov odam o'ta xavfli kasallikning so'nggi bosqichida bo'lganida, qiyin qarorlar qabul qilinishi mumkinligini tushunadi. Cherkovning ta'kidlashicha, "o'lim muqarrar bo'lganda, o'limga baraka va abadiy mavjudotning maqsadli qismi sifatida qarash kerak. A'zolar o'lik hayotni asossiz vositalar bilan uzaytirish majburiyatini his qilmasliklari kerak.[38]
Neytrallik
Tibbiy mutaxassislar vakili bo'lgan tashkilotlarni muxolifat pozitsiyasiga emas, balki o'limga yordam berishda neytral pozitsiyani egallashga chaqiriqlar bo'lgan. Buning sababi shundaki, bu tibbiyot mutaxassislari va keng jamoatchilikning fikrlarini yaxshiroq aks ettiradi va ushbu organlarning munozaralarga ortiqcha ta'sir ko'rsatishini oldini oladi.[39][40][41]
Buyuk Britaniya Qirollik hamshiralik kolleji 2009 yil iyul oyida o'limga yordam berish bo'yicha neytral pozitsiyaga o'tish uchun ovoz berdi.[42]
The Kaliforniya tibbiyot birlashmasi 2015 yilda u erda o'lishga yordam beradigan qonun loyihasini kiritish kerakmi yoki yo'qmi degan munozaralar paytida uzoq vaqtdan beri davom etib kelayotgan muxolifatini tashladi, qisman saraton kasalligiga chalingan Bretan Meynard.[43] The Kaliforniya umrining oxiri to'g'risida qonun o'sha yili qonun bilan imzolandi.
2017 yil dekabr oyida Massachusets tibbiyot jamiyati (MMS) shifokorlarning yordami bilan o'z joniga qasd qilishga qarshi bo'lgan qarshiliklarini bekor qilish va betaraflik pozitsiyasini qabul qilish uchun ovoz berdi.[44]
2018 yil oktyabr oyida Amerika oilaviy shifokorlar akademiyasi (AAFP) muxolifat taraflaridan betaraflik pozitsiyasini qabul qilishga ovoz berdi. Bu tomonidan olingan pozitsiyaga ziddir Amerika tibbiyot assotsiatsiyasi (AMA), kim bunga qarshi.[45]
2019 yil yanvar oyida inglizlar Qirollik shifokorlar kolleji a'zolarining uchdan ikki qismi, yordam beriladigan o'lishni qonuniylashtirishni qo'llab-quvvatlashi yoki qarshi bo'lishi kerak deb o'ylamaguncha, betaraflik pozitsiyasini qabul qilishini e'lon qildi.[46]
Sog'liqni saqlash xodimlarining munosabati
O'z joniga qasd qilish va ixtiyoriy evtanaziya jarayonida shifokorlar muayyan rol o'ynashi kerakligi keng tan olingan ("shifokorning yordami bilan o'z joniga qasd qilish" nomidan ham ko'rinib turibdi), ko'pincha ularni masalaning birinchi o'ringa qo'yadi. Bir necha o'n yillik fikr-mulohazalar shuni ko'rsatadiki, AQSh va Evropaning bir qator mamlakatlaridagi shifokorlar PASni legallashtirishni keng jamoatchilikka qaraganda kamroq qo'llab-quvvatlaydilar.[47] AQShda, "1970-yillardan beri Amerika jamoatchiligining uchdan ikki qismi" qonuniylashtirishni qo'llab-quvvatlagan bo'lsa-da, shifokorlar o'rtasida o'tkazilgan so'rovlar "kamdan-kam hollarda harakatni yarmini qo'llab-quvvatlaydi".[47] Shu bilan birga, quyidagi jadvallarda ko'rsatilgandek, shifokor va boshqa sog'liqni saqlash sohasidagi professional fikrlar shifokorlar yordami bilan o'z joniga qasd qilish masalasida juda xilma-xil.
| O'qish | Aholisi | PAS-ga yordam berishga tayyor | PAS-ga yordam berishni xohlamayman | ||
|---|---|---|---|---|---|
| Kanada tibbiyot birlashmasi, 2011 yil[48] | Kanada tibbiyot birlashmasi (n = 2,125) | 16% | 44% | ||
| Koen, 1994 (NEJM)[49] | Vashington shtati shifokorlari (n = 938) | 40% | 49% | ||
| Li, 1996 yil (NEJM)[50] | Oregon shtati shifokorlari (n = 2,761) | 46% | 31% | ||
| O'qish | Aholisi | PAS qonuniy bo'lishi foydasiga | PAS qonuniy bo'lishi tarafdori emas | ||
|---|---|---|---|---|---|
| Medscape axloqiy hisoboti, 2014 yil[51] | AQShda joylashgan shifokorlar | 54% | 31% | ||
| Seal, 2009 yil[47] | Birlashgan Qirollik shifokorlari (n = 3,733) | 35% | 62.2% | ||
| Koen, 1994 (NEJM)[49] | Vashington shtati shifokorlari (n = 938) | 53% | 39% | ||
Pasga bo'lgan munosabat sog'liqni saqlash kasbiga qarab ham farq qiladi; 3733 tibbiyot shifokorlari o'rtasida o'tkazilgan keng qamrovli tadqiqotlar Palliativ yordam bo'yicha Milliy Kengash, Yoshga oid tashvishlar, Xospislarga yordam berish, Makmillan saraton kasalligini qo'llab-quvvatlash, Motor neyron kasalliklari assotsiatsiyasi, MS jamiyati va Syu Rayder Care tomonidan ko'ngilli evtanaziya va PASga qarshi chiqish ekanligini ko'rsatdi. Palliativ yordam va keksa yoshdagi parvarish bo'yicha mutaxassislar orasida eng yuqori ko'rsatkichdir, qonunning o'zgarishiga qarshi palliativ yordam mutaxassislarining 90% dan ortig'i.[47]
1997 yilda Glazgo Universitetining tibbiyotdagi huquq va axloq instituti tomonidan o'tkazilgan tadqiqotda farmatsevtlar (72%) va anestezistlar (56%) odatda PASni qonuniylashtirish tarafdori ekanligi aniqlandi. Farmatsevtlar tibbiyot shifokorlaridan ikki barobar ko'proq "agar bemor o'z hayotini tugatishga qaror qilgan bo'lsa, shifokorlarga qonun bilan yordam berishlari kerak" degan fikrni ma'qullashdi.[52] 2017 yil yanvar oyida NPR tomonidan chop etilgan hisobotda shuni ko'rsatadiki, shifokorlarga Qo'shma Shtatlar ichida o'z joniga qasd qilishni qonuniylashtirgan munitsipalitetlarda qatnashishdan saqlanish uchun imkon beradigan himoya choralari hozirda ushbu amaliyotni amalga oshirish huquqiga ega bo'lganlar tomonidan kirish etishmasligini keltirib chiqaradi.[53]
Birlashgan Qirollikda o'tkazilgan so'rovnoma shuni ko'rsatdiki, umumiy amaliyot shifokorlarining 54 foizi yordam beradigan o'lish to'g'risidagi qonunlarni kiritishga tarafdor yoki betarafdir.[54] Shunga o'xshash so'rovnoma Shifokorlar.net.uk nashr etilgan BMJ shifokorlarning 55 foizi buni qo'llab-quvvatlashini aytdi.[55] Aksincha BMA, Buyuk Britaniyadagi shifokorlar vakili, bunga qarshi.[56]
2000 yilda Shimoliy Irlandiyadagi barcha umumiy amaliyot shifokorlari o'rtasida o'tkazilgan anonim, maxfiy pochta so'rovi shuni ko'rsatdiki, umumiy shifokorlarning 70% dan ortig'i shifokorlar yordami bilan o'z joniga qasd qilish va ixtiyoriy ravishda faol evtanaziyaga qarshi bo'lgan.[57]
Qonuniylik
Ixtiyoriy evtanaziya qonuniylashtirildi Gollandiya (2002 yilda), Belgiya (2002 yilda), Lyuksemburg (2008 yilda),[58] va Kanada (2016 yilda).[59] Shifokorlar yordami bilan o'z joniga qasd qilish Kanada, Niderlandiya, Lyuksemburg, Shveytsariya, Avstraliyaning Viktoriya shtati va Qo'shma Shtatlarning ayrim joylarida qonuniydir. Qo'shma Shtatlarda o'limga duchor bo'lgan qonunlar yoki sud qarorlari mavjud bo'lib, ular davolanishi mumkin bo'lgan kattalar uchun cheklangan Oregon, Montana,[eslatma 1][60] Vashington, Vermont, Meyn (2020 yil 1-yanvar), Nyu-Jersi, Gavayi, Kaliforniya, Kolorado va Vashington[61] Qonunlar bemorning davolovchi shifokori aqliy qobiliyatini tasdiqlashini talab qiladi. Oregon Qo'shma Shtatlarning birinchi shtati bo'lib, unga yordam berish orqali o'z joniga qasd qilishni qonuniylashtirdi, unga xalq ovozi bilan erishildi. Ushbu qonun Oregon shtatidagi saylovchilar tomonidan ikki marta qabul qilingan fuqarolarning tashabbusi edi. Birinchi marta 1994 yil noyabr oyida bo'lib o'tgan umumiy saylovlarda u 51% dan 49% gacha bo'lgan farq bilan o'tgan edi. Buyruq Amalga oshirilgan qonun 1997 yil 27 oktyabrda bekor qilinmaguncha kechiktirildi. 1997 yil noyabr oyida umumiy saylov byulletenida Qonunni bekor qilish chorasi ko'rildi. Saylovchilar Qonunni 60% dan 40% gacha ushlab turishni tanladilar.[62]
Avstraliya
O'z joniga qasd qilish bilan bog'liq qonunlar Avstraliya bu masala davlat hukumatlari va hududlar bo'yicha esa federal hukumat. Viktoriya shtatida hozirda shifokorlar yordami bilan o'z joniga qasd qilish qonuniy hisoblanadi[63] va G'arbiy Avstraliya.[64] Boshqa barcha shtatlar va hududlarda u noqonuniy bo'lib qolmoqda.
Viktoriya qonunchiligiga ko'ra, bemorlar tibbiy amaliyotchilarga ixtiyoriy ravishda yordam berish to'g'risida so'rashlari mumkin, vrachlar, shu jumladan vijdonan voz kechganlar, vijdonan qarshi bo'lmagan tegishli o'qitilgan hamkasblariga murojaat qilishlari kerak.[65] Sog'liqni saqlash amaliyotchilari suhbatni boshlash yoki bemorga tezkor ravishda yordam berish uchun o'lishni taklif qilishlari bilan cheklangan.
Ixtiyoriy evtanaziya qonuniy edi Shimoliy hudud ostida qisqa vaqt davomida "Terminal kasal" to'g'risidagi qonunning huquqlari 1995 yil Ushbu qonun Federal hukumat tomonidan bekor qilinmaguncha, u o'limga yordam berish to'g'risidagi qonunlarni qabul qilish uchun hududlarni bekor qildi. O'rtasida juda ko'p tortishuvlarga sabab bo'lgan "Evtanaziya mashinasi" birinchi bo'lib ixtiro qilingan ixtiyoriy yordam beradigan o'lik mashina ixtiro qilindi. Filipp Nitske Ushbu davrda ishlatilgan, hozirgi kunda London "s Ilmiy muzey.[66]
Belgiya
Evtanaziya to'g'risidagi qonun qonuniylashtirildi ixtiyoriy evtanaziya 2002 yilda Belgiyada,[67][68] ammo u vrach yordamidagi o'z joniga qasd qilishni qamrab olmagan.[69]
Kanada
O'z joniga qasd qilish Kanadada 1972 yilgacha jinoiy javobgarlik sifatida ko'rib chiqilgan. Kvebek viloyatida shifokorlar yordami bilan o'z joniga qasd qilish 2014 yil 5 iyundan beri qonuniy hisoblanadi.[70] Orqali butun mamlakat bo'ylab qonuniy deb e'lon qilindi Kanada Oliy sudi qaror Karter Kanadaga qarshi (Bosh prokuror) 2015 yil 6-fevral kuni.[71] Uzoq kechikishdan so'ng, jamoalar palatasi qonun loyihasini qabul qildi[72] 2016 yil iyun oyining o'rtalarida bu shifokorning yordami bilan o'z joniga qasd qilishga imkon beradi. 2015 yil 10 dekabrdan 2017 yil 30 iyungacha Kanadada tibbiy yordam bilan o'ldirilgan 2149 kishi hujjatlashtirilgan. Kanada sog'liqni saqlash tomonidan nashr etilgan tadqiqotlar, shifokorlar tomonidan boshqariladigan ixtiyoriy evtanaziyaga bo'lgan afzalliklarini aks ettiradi, bunda bemorlarni o'zlarini boshqarish samaradorligini oshirish va oldini olish xavotirlari keltirilgan.[73]
Xitoy
Xitoyda o'z joniga qasd qilish yordami Xitoy Xalq Respublikasi Jinoyat qonunining 232 va 233-moddalari bo'yicha noqonuniy hisoblanadi.[74] Xitoyda o'z joniga qasd qilish yoki beparvolik qotillik deb hisoblanadi va uch yildan etti yilgacha ozodlikdan mahrum qilish bilan jazolanishi mumkin.[75] 2011 yil may oyida Xitoyning Tszyansi provinsiyasidagi Longnan okrugi Xalq sudi tomonidan fermer Zhong Yichun Zeng Tsianxiangga o'z joniga qasd qilishda yordam bergani uchun ikki yillik qamoq jazosiga hukm qilindi. Zeng ruhiy kasallikka chalingan va bir necha bor Zhongdan o'z joniga qasd qilishda yordam berishini so'ragan. 2010 yil oktyabr oyida Zeng ortiqcha uyqu tabletkalarini ichdi va g'orda yotdi. Rejalashtirilganidek, 15 daqiqadan so'ng Zhong unga vafot etganligini tasdiqlash uchun qo'ng'iroq qilib, ko'mdi. Ammo, otopsi xulosasiga ko'ra, o'limning sababi haddan tashqari dozani emas, bo'g'ilishdan bo'lgan. Zhong jinoiy ehtiyotsizlikda aybdor deb topildi. 2011 yil avgust oyida Zhong sud hukmidan shikoyat qildi, ammo u rad etildi.[75]
1992 yilda shifokor saraton kasalligi bilan kasallangan bemorni o'ldiruvchi in'ektsiya yo'li bilan o'ldirishda ayblandi. Oxir-oqibat u oqlandi.[75]
Kolumbiya
1997 yil may oyida Kolumbiya Konstitutsiyaviy sudi 1980 yilgi Jinoyat kodeksining 326-moddasini qabul qilib, hayotini tugatishni so'ragan kasal bemorlarning ixtiyoriy evtanaziyasiga yo'l qo'ydi.[76] Ushbu qaror o'z muvaffaqiyatiga ixtiyoriy evtanaziyaga qarshi bo'lgan guruhning sa'y-harakatlari tufayli qarzdor. Uning a'zolaridan biri unga qarshi Kolumbiya Oliy sudiga da'vo arizasi bilan murojaat qilganida, sud 6 dan 3 gacha bo'lgan qarorni qabul qilib, "o'ta og'ir kasalning ixtiyoriy evtanaziya bilan shug'ullanish huquqlarini bayon qildi".[77]
2015 yil fevral oyida Oliy sud hukumatga shifokorlar uchun keng qamrovli ko'rsatmalar to'plamini yaratish, ularga qonun buzilishining oldini olishda yordam berish uchun 30 kun muhlat berdi, chunki texnik jihatdan qonuniy bo'lsa-da, ko'plab shifokorlar sud jarayonlariga duch kelishadi, bu erda ular barcha qonuniy talablar protseduradan oldin uchrashdi. Ushbu qonuniy choralardan qo'rqish ko'plab shifokorlarni qonuniyligiga qaramay, protsedurani bajarishdan bosh tortishiga olib keldi.[78]
Daniya
Daniyada o'z joniga qasd qilish yordami noqonuniy hisoblanadi. Passiv evtanaziya yoki davolanishni rad etish noqonuniy emas. So'rovlardan birida Daniya aholisining 71% ixtiyoriy evtanaziya va shifokorlar yordami bilan o'z joniga qasd qilishni qonuniylashtirish tarafdori ekanligi aniqlandi.[79]
Frantsiya
O'z joniga qasd qilish yordami Frantsiyada qonuniy emas. Ixtiyoriy evtanaziya va vrachlar yordami bilan o'z joniga qasd qilishni qonuniylashtirish to'g'risidagi qarama-qarshiliklar AQShda bo'lgani kabi katta emas, chunki mamlakat "yaxshi rivojlangan". xospis parvarish qilish dasturi ".[80] Biroq, 2000 yilda Vinsent Humbert bilan mavzu bo'yicha tortishuvlar paydo bo'ldi. "Yurish, ko'rish, gapirish, hidlash yoki tatib ko'rishga" qodir bo'lmagan avtohalokatdan so'ng u kitob yozish uchun o'ng bosh barmog'ining harakatidan foydalangan, Men o'lish huquqini so'rayman (Je vous demande le droit de mourir) unda u "qonuniy o'lish" istagini bildirgan.[80] Uning apellyatsiyasi rad etilgandan so'ng, onasi uni o'ldirishda yordam berib, unga barbiturat dozasini oshirib yuborgan va uni koma, ikki kundan keyin uni o'ldirgan. Garchi uning onasi o'g'lining o'limiga yordam bergani uchun hibsga olingan va keyinchalik oqlangan bo'lsa ham, ish yangi boshlandi qonunchilik tibbiyot "hayotni sun'iy qo'llab-quvvatlashdan boshqa hech qanday maqsadga xizmat qilmasa", uni "to'xtatib qo'yish yoki qabul qilmaslik" mumkinligini ta'kidlaydi.[81]
Germaniya
Birovni talablariga binoan o'ldirish har doim ham noqonuniy hisoblanadi Germaniya jinoyat kodeksi (216-band, "Jabrlanuvchining iltimosiga binoan o'ldirish; rahm-shafqat bilan o'ldirish").[82]
O'z joniga qasd qilishga yordam berish odatda qonuniydir. O'z joniga qasd qilishning o'zi qonuniy ekan, yordam yoki rag'batlantirish sheriklik va qo'zg'ash bilan bog'liq odatdagi huquqiy mexanizmlar bilan jazolanmaydi (Germaniya jinoyat qonunchiligi "sheriklik aksessuarlari" g'oyasiga amal qiladi, unda "boshqa odamni sodir etishga undovchi shaxsning motivlari o'z joniga qasd qilish yoki uning bajarilishiga yordam beradiganlar ahamiyatsiz ").[83] Shuningdek, o'z joniga qasd qilishda jinoyat kodeksida aniq taqiqlangan yordam ham yo'q. Biroq, ba'zi bir sabablarga ko'ra muayyan sharoitlarda qonuniy oqibatlar bo'lishi mumkin. Qurol qurollari, boshqariladigan moddalar savdosi va shu kabilar bilan ishlashni tartibga soluvchi qonunlardan tashqari (masalan, o'z joniga qasd qilish uchun zahar olayotganda), bu uch narsaga tegishli:
Bepul va manipulyatsiya qilingan iroda
Agar o'z joniga qasd qilgan shaxs o'z xohish-irodasi bilan harakat qilmasa, yordam uchun jinoyat kodeksida ko'zda tutilgan qotillik jinoyatlarining har qanday biri, masalan, "boshqa shaxs orqali harakat qilgani" uchun jazolanadi (nemis tilining 25-moddasi, 1-qismi) jinoiy kodeks,[84] odatda "mittelbare Täterschaft" deb nomlanadi). O'z xohish-irodasidan tashqari harakat o'z hayotini o'zi tugatish to'g'risidagi qaror bilan chiqarib tashlanmaydi; o'z joniga qasd qilgan kishi "oxirigacha o'z taqdirini o'zi hal qilib [...] va vaziyatni o'z qo'liga olgan" ekan, buni taxmin qilish mumkin.[83]
Biroq, kimdir manipulyatsiya qilingan yoki aldangan bo'lsa, irodani qabul qilib bo'lmaydi. Buning uchun nemis qonunchiligida klassik darslik namunasi deyiladi Sirius ishi bo'yicha Federal Adliya sudi 1983 yilda hukmronlik qilgan: Ayblanuvchi tanishini, agar u o'zini o'ldirsa, u yaxshi hayotga qaytishiga ishontirgan. U muvaffaqiyatsiz o'z joniga qasd qilishga urinib ko'rdi, ayblanuvchiga ayblov e'lon qilindi va oxir-oqibat qotillikka urinishda ayblandi.[85] (Shuningdek, ayblanuvchi tanishini yulduzdan qutlaganiga ishontirgan edi Sirius, shuning uchun ishning nomi).
Manipulyatsiyadan tashqari, jinoyat kodeksida shaxs o'z xohish-irodasi bilan harakat qilmaslikning uchta sharti ko'rsatilgan:
- agar kishi 14 yoshga to'lmagan bo'lsa
- agar shaxsda "Germaniya Jinoyat kodeksining 20-§ qismida sanab o'tilgan ruhiy kasalliklardan biri bo'lsa"[83]
- favqulodda holat sharoitida harakat qiladigan shaxs.
Bunday sharoitda, hatto og'zaki nutq bilan aytganda, odam o'z xohish-irodasi bilan harakat qilmoqda, deb aytsa ham, qotillik uchun hukm qilinishi mumkin.
Qutqarish vazifasi beparvo qilingan
Germaniya jinoyat qonuni har kimni favqulodda vaziyatda boshqalarni qutqarishga ma'lum chegaralar ichida kelishga majbur qiladi (Germaniya Jinoyat kodeksining 323-moddasi, "Yengil qutqaruvga yo'l qo'ymaslik").[86] Bu shuningdek a qutqarish vazifasi inglizchada. Ushbu qoidaga ko'ra, o'z joniga qasd qilish holatida bo'lgan odamni topishda, o'z joniga qasd qilishga yordam beradigan tomon sudlanishi mumkin behushlik, ular mavzuni jonlantirish uchun qo'llaridan kelgan hamma narsani qilmaydilar.[83] Boshqacha qilib aytadigan bo'lsak, agar kimdir o'z joniga qasd qilishda odamga yordam bersa, tark etadi, lekin qaytib kelib, odamni hushsiz holda topsa, ularni qayta tiklashga harakat qilish kerak.[83]
Ushbu mulohaza yuridik olimlar tomonidan, masalan, o'z joniga qasd qilishning bir qismi bo'lgan hayotga tahdid soluvchi holat favqulodda holat emasligi haqida bahs yuritilmoqda. Ushbu mudofaaga tayanadiganlar uchun Federal Adliya sudi ilgari favqulodda vaziyat deb hisoblagan.
Yo'qotish bilan qotillik
Nemis qonunchiligi boshqalarni farovonligi uchun kafil (Garantenstellung) lavozimiga qo'yadi, masalan. ota-onalar, turmush o'rtoqlar, shifokorlar va politsiya xodimlari. Bunday odamlar o'zlarini o'z joniga qasd qilishning oldini olish uchun qo'llaridan kelganicha harakat qilishlari mumkin. agar bunday qilmasalar, ular tashlab qo'yilgan qotillikda aybdor.
Shveytsariyaga sayohat
1998 yildan 2018 yilgacha Germaniyaning taxminan 1250 fuqarosi (boshqa millat sonidan deyarli uch baravar ko'p) sayohat qilgan Dignitas yilda Tsyurix, Shveytsariya o'z joniga qasd qilish uchun, bu 1918 yildan beri qonuniydir.[87][88] Shveytsariya norezident chet elliklar uchun o'z joniga qasd qilishga yordam beradigan kam sonli mamlakatlardan biri.[89]
Shifokor yordami bilan o'z joniga qasd qilish
Shifokorlar yordami bilan o'z joniga qasd qilish rasmiy ravishda 2020 yil 26 fevralda Germaniyaning yuqori sudi "professional yordam bilan o'z joniga qasd qilish" taqiqini olib tashlaganida rasmiylashtirildi.[90]
Islandiya
O'z joniga qasd qilish noqonuniy hisoblanadi.[91]
Irlandiya
O'z joniga qasd qilish noqonuniy hisoblanadi. "Evtanaziya ham, yordamga qasd qilish ham Irlandiya qonunchiligiga binoan noqonuniy hisoblanadi. Shartlarga qarab evtanaziya odam o'ldirish yoki qotillik sifatida qabul qilinadi va umrbod qamoq jazosi bilan jazolanadi".[92]
Lyuksemburg
Ixtiyoriy evtanaziya va vrachlar yordami bilan o'z joniga qasd qilishni qonuniylashtirish bo'yicha yana bir bor qirollik roziligini olmaganidan so'ng, 2008 yil dekabrida Lyuksemburg parlamenti mamlakat konstitutsiyasiga ushbu hokimiyatni monarxdan tortib olish uchun o'zgartirish kiritdi. Lyuksemburgning Buyuk gersogi.[93] Ixtiyoriy evtanaziya va shifokor yordami bilan o'z joniga qasd qilish mamlakatda 2009 yil aprel oyida qonuniylashtirildi.[94]
Nederlandiya
Niderlandiya dunyodagi birinchi mamlakat bo'lib, ixtiyoriy evtanaziyani rasmiy ravishda qonuniylashtirdi.[95] Shifokor yordami bilan o'z joniga qasd qilish ixtiyoriy evtanaziya bilan bir xil sharoitda qonuniy hisoblanadi. Shifokorlar yordami bilan o'z joniga qasd qilishga 2001 yil qonuni bo'yicha ruxsat berildi, unda bunday yordamni ko'rsatish uchun zarur bo'lgan aniq tartib va talablar ko'rsatilgan. Niderlandiyada o'z joniga qasd qilish tibbiy uslubga asoslanib amalga oshiriladi, bu faqat "chidab bo'lmas darajada umidsiz azob chekayotgan bemorlarning shifokorlari" degan ma'noni anglatadi.[96] o'z joniga qasd qilish to'g'risida so'rovni qondirishga ruxsat beriladi. Niderlandiya 12 yoshdan katta odamlarga zarurat tug'ilganda, o'z joniga qasd qilishga qodir.
Yangi Zelandiya
Yordam berilgan o'z joniga qasd qilish Yangi Zelandiya bo'yicha majburiy referendumdan so'ng dekriminallashtirildi Hayotni tugatish to'g'risidagi qonun 2019 yil. Biroq, qonunchilik 2021 yil 6-noyabrda kuchga kirgunga qadar bir yilga kechikishni nazarda tutadi. 1961 yilgi Jinoyatlar to'g'risidagi qonunning 179-bo'limiga binoan, "o'z joniga qasd qilishga ko'mak berish" noqonuniy hisoblanadi va bu oxirigacha belgilangan doiradan tashqarida qoladi. hayotni tanlash to'g'risidagi qonun.
Janubiy Afrika
Janubiy Afrikada ixtiyoriy evtanaziyani qonuniylashtirish va shifokorlar yordami bilan o'z joniga qasd qilishni muhokama qilish bilan kurashmoqda. Mamlakatning aksariyat qismini qamrab olgan sog'liqni saqlash tizimining rivojlanmaganligi sababli, "Janubiy Afrika qonun komissiyasining a'zosi Uillem Doktorlar Butunjahon Kongressidagi evtanaziya bo'yicha simpoziumda" Uillem Landman ko'plab janubiy afrikalik shifokorlar bunga tayyor bo'lishlarini ta'kidladilar. mamlakatda qonuniylashtirilgandan so'ng ixtiyoriy evtanaziya harakatlarini amalga oshirish.[97] Uning fikriga ko'ra, mamlakatda shifokorlar etishmasligi sababli, "Janubiy Afrikada evtanaziyani [qonuniylashtirish] erta va amaliyotga tatbiq etish qiyin bo'lar edi [...]".[97]
2015 yil 30 aprelda Oliy sud in Pretoriya advokat Robin Stransham-Fordga shifokorga ayblov tahdidisiz o'z hayotini olib ketishda yordam berishiga imkon beradigan buyruq berdi. 2016 yil 6 dekabrda Oliy Apellyatsiya sudi Oliy sud qarorini bekor qildi.[98]
Shveytsariya
Ba'zi hollarda bemorga o'lishda yordam berish noqonuniy bo'lsa ham, boshqa biron bir jinoyat sodir etilmagan holatlar mavjud.[99] Shveytsariya Jinoyat kodeksining tegishli qoidasi[100] "g'arazli sabablarga ko'ra kimnidir o'z joniga qasd qilishga undagan yoki bunga yordam beradigan shaxs, agar o'z joniga qasd qilish sodir etilgan yoki unga urinish qilingan bo'lsa, ozodlikdan mahrum qilish jazosiga hukm qilinadi."Zuxtaus) 5 yilgacha ozodlikdan mahrum qilish yokiGefangnis)."
A person brought to court on a charge could presumably avoid conviction by proving that they were "motivated by the good intentions of bringing about a requested death for the purposes of relieving "azob " rather than for "selfish" reasons.[101] In order to avoid conviction, the person has to prove that the deceased knew what he or she was doing, had capacity to make the decision, and had made an "earnest" request, meaning they asked for death several times. The person helping also has to avoid actually doing the act that leads to death, lest they be convicted under Article 114: Killing on request (Tötung auf Verlangen) -A person who, for decent reasons, especially compassion, kills a person on the basis of his or her serious and insistent request, will be sentenced to a term of imprisonment (Gefängnis). For instance, it should be the suicide subject who actually presses the syringe or takes the pill, after the helper had prepared the setup.[102] This way the country can criminalise certain controversial acts, which many of its people would oppose, while legalising a narrow range of assistive acts for some of those seeking help to end their lives.
Switzerland is one of only a handful of countries in the world which permits assisted suicide for non-resident foreigners,[89] causing what some critics have described as o'z joniga qasd qilish turizmi. Between 1998 and 2018 around 1'250 German citizens (almost three times the number of any other nationality) travelled to Dignitas yilda Tsyurix, Shveytsariya for an assisted suicide. During the same period over 400 British citizens also opted to end their life at the same clinic.[87][88]
2011 yil may oyida, Tsyurix saylovchilarga (i) o'z joniga qasd qilishni to'g'ridan-to'g'ri taqiqlash kerakmi yoki yo'qligini so'ragan referendum o'tkazdi; va (ii) Dignitas va boshqa yordamchi o'z joniga qasd qilish provayderlari xorijdagi foydalanuvchilarni qabul qilmasliklari kerakmi. Tsyurix saylovchilari ikki shveytsariyalik evtanaziyaga qarshi lobbichilik qilganiga qaramay, ikkala taqiqni ham rad etishdi ijtimoiy konservativ siyosiy partiyalar Shveytsariyaning Evangelist Xalq partiyasi va Federal Democratic Union. To'g'ridan-to'g'ri taqiqlash to'g'risidagi taklif 84 foiz saylovchilar tomonidan rad etildi, 78 foiz chet el foydalanuvchilari talab qilsa xizmatlarni ochiq holda saqlashga ovoz berishdi.[103]
In Switzerland non-physician-assisted suicide is legal, the assistance mostly being provided by volunteers, whereas in Belgium and the Netherlands, a physician must be present. In Switzerland, the doctors are primarily there to assess the patient's decision capacity and prescribe the lethal drugs. Additionally, unlike cases in the United States, a person is not required to have a terminal illness but only the capacity to make decisions. About 25% of people in Switzerland who take advantage of assisted suicide do not have a terminal illness but are simply old or "tired of life".[104]
Publicized cases
2006 yil yanvar oyida britaniyalik shifokor Anne Tyorner Tsyurix klinikasida davolanib bo'lmaydigan degenerativ kasallikka chalinganligi sababli o'z hayotini qurbon qildi. Uning hikoyasi Bi-bi-si tomonidan xabar qilingan va keyinchalik, 2009 yilda televizion filmga aylangan A Short Stay in Switzerland yulduzcha Julie Uolters.
2009 yil iyulda Britaniyalik dirijyor Sir Edward Downes va uning rafiqasi Joan Tsyurix tashqarisidagi o'z joniga qasd qilish klinikasida "o'z xohishiga ko'ra" vafot etgan. Ser Edvard o'lik kasal emas edi, ammo uning rafiqasida tez rivojlanayotgan saraton kasalligi aniqlandi.[105]
2010 yil mart oyida PBS FRONTLINE TV program in the United States showed a documentary called "The Suicide Tourist" which told the story of Professor Craig Ewert, his family, and Dignitas, and their decision to commit assisted suicide using natriy pentobarbital in Switzerland after he was diagnosed and suffering with ALS (Lou Gerigning kasalligi).[106]
In June 2011, The BBC televised the assisted suicide of Peter Smedley, a canning factory owner, who was suffering from motor neurone disease. The programme – Sir Terry Pratchett's Choosing To Die – told the story of Peter's journey to the end where he used The Dignitas Clinic, a voluntary euthanasia clinic in Switzerland, to assist him in carrying out the taking of his own life.The programme shows Peter eating chocolates to counter the unpalatable taste of the liquid he drinks to end his own life. Moments after drinking the liquid, Peter begged for water, gasped for breath and became red, he then fell into a deep sleep where he snored heavily while holding his wife's hand. Minutes later, Peter stopped breathing and his heart stopped beating.
Urugvay
Assisted suicide, while criminal, does not appear to have caused any convictions, as article 37 of the Penal Code (effective 1934) states: "The judges are authorized to forego punishment of a person whose previous life has been honorable where he commits a homicide motivated by compassion, induced by repeated requests of the victim."[107]
Birlashgan Qirollik
Angliya va Uels
Deliberately assisting a suicide is illegal.[108] 2003 yildan 2006 yilgacha Lord Joffe made four attempts to introduce bills that would have legalised physician-assisted suicide in England & Wales—all were rejected by the UK Parliament.[109] In the meantime the Director of Public Prosecutions has clarified the criteria under which an individual will be prosecuted in England and Wales for assisting in another person's suicide.[110] These have not been tested by an appellate court as yet[111]2014 yilda Lord Falconer of Thoroton tabled an Assisted Dying Bill in the House of Lords which passed its Second Reading but ran out of time before the General Election. During its passage peers voted down two amendments which were proposed by opponents of the Bill. In 2015 Labour MP Rob Marris introduced another Bill, based on the Falconer proposals, in the House of Commons. The Second Reading was the first time the House was able to vote on the issue since 1997. A Populus poll had found that 82% of the British public agreed with the proposals of Lord Falconer's Assisted Dying Bill.[112] However, in a free vote on 11 September 2015, only 118 MPs were in favour and 330 against, thus defeating the bill.[113]
Shotlandiya
Unlike the other jurisdictions in the United Kingdom, suicide was not illegal in Scotland before 1961 (and still is not) thus no associated offences were created in imitation. Depending on the actual nature of any assistance given to a suicide, the offences of qotillik yoki aybdor qotillik might be committed or there might be no offence at all; the nearest modern prosecutions bearing comparison might be those where a culpable homicide conviction has been obtained when drug addicts have died unintentionally after being given "hands on" non-medical assistance with an injection. Modern law regarding the assistance of someone who intends to die has a lack of certainty as well as a lack of relevant case law; this has led to attempts to introduce statutes providing more certainty.
Independent MSP Margo MacDonald's "End of Life Assistance Bill" was brought before the Scottish Parliament to permit physician-assisted suicide in January 2010. The Katolik Church and the Shotlandiya cherkovi, the largest denomination in Scotland, opposed the bill. The bill was rejected by a vote of 85–16 (with 2 abstentions) in December 2010.[114][115]
The Assisted Suicide (Scotland) Bill was introduced on 13 November 2013 by the late Margo MacDonald MSP and was taken up by Patrik Harvi MSP on Ms MacDonald's death. The Bill entered the main committee scrutiny stage in January 2015 and reached a vote in Parliament several months later; however the bill was again rejected.
Shimoliy Irlandiya
Health is a hal qilingan modda in the United Kingdom and as such it would be for the Shimoliy Irlandiya assambleyasi to legislate for assisted dying as it sees fit. As of 2018, there has been no such bill tabled in the Assembly.
O'layotgan koalitsiyaga yordam
A coalition of assisted dying organizations working in favour of legal recognition of the right to die was formed in early 2019.[116]
Qo'shma Shtatlar
1 In some states assisted suicide is protected through court ruling even though specific legislation allowing it does not exist.
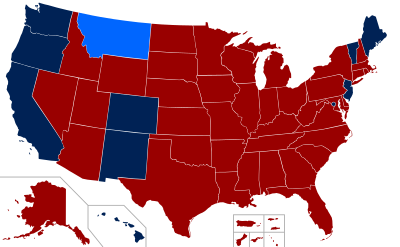
Assisted death is legal in the American states of Kaliforniya (orqali Kaliforniya umrining oxiri to'g'risida qonun of 2015, enacted June 2016),[117] Kolorado (End of Life Options Act of 2016), Gavayi (Death with Dignity Act of 2018), Oregon (orqali Oregon Death with Dignity Act, 1994),[118] Vashington (Vashington qadr-qimmati to'g'risidagi qonunda of 2008), Vashington shahar (District of Columbia Death with Dignity Act of 2016), Nyu-Jersi (New Jersey Dignity in Dying Bill of Rights Act of 2019), Meyn[119] (eff. 1 January 2020 - Maine Death with Dignity Act of 2019) and Vermont (Patient Choice and Control at End of Life Act of 2013). Yilda Montana, the Montana Supreme Court ruled in Baxter va Montana (2009) that it found no law or public policy reason that would prohibit physician-assisted dying.[60] Oregon and Washington specify some restrictions. It was briefly legal in Nyu-Meksiko from 2014, but this verdict was overturned in 2015. Meyn is the most recent state that has legalized physician-assisted suicide, with a bill passed by the state assembly in June and approved by the Governor on 12 June 2019. The law went into legal effect on 1 January 2020.
Oregon requires a physician to prescribe drugs and they must be self-administered. In order to be eligible, the patient must be diagnosed by an attending physician as well as by a consulting physician, with a terminal illness that will cause the death of the individual within six months. The law states that, in order to participate, a patient must be: 1) 18 years of age or older, 2) a resident of Oregon, 3) capable of making and communicating health care decisions for him/herself, and 4) diagnosed with a terminal illness that will lead to death within six months. It is up to the attending physician to determine whether these criteria have been met.[62] It is required the patient orally request the medication at least twice and contribute at least one (1) written request. The physician must notify the patient of alternatives; such as palliative care, hospice and pain management. Lastly the physician is to request but not require the patient to notify their next of kin that they are requesting a prescription for a lethal dose of medication. Assuming all guidelines are met and the patient is deemed competent and completely sure they wish to end their life, the physician will prescribe the drugs.[120]
The law was passed in 1997. As of 2013, a total of 1,173 people had DWDA prescriptions written and 752 patients had died from ingesting drugs prescribed under the DWDA.[121] In 2013, there were approximately 22 assisted deaths per 10,000 total deaths in Oregon.[121]
Washington's rules and restrictions are similar, if not exactly the same, as Oregon's. Not only does the patient have to meet the above criteria, they also have to be examined by not one, but two doctors licensed in their state of residence. Both doctors must come to the same conclusion about the patient's prognosis. If one doctor does not see the patient fit for the prescription, then the patient must undergo psychological inspection to tell whether or not the patient is in fact capable and mentally fit to make the decision of assisted death or not.[120]
In May 2013, Vermont became the fourth state in the union to legalize medical aid-in-dying. Vermont's House of Representatives voted 75–65 to approve the bill, Patient Choice and Control at End of Life Act. This bill states that the qualifying patient must be at least 18, a Vermont resident and suffering from an incurable and irreversible disease, with less than six months to live. Also, two physicians, including the prescribing doctor must make the medical determination.[122]
In January 2014, it seemed as though New Mexico had inched closer to being the fifth state in the United States to legalize physician-assisted suicide via a court ruling.[123] "This court cannot envision a right more fundamental, more private or more integral to the liberty, safety and happiness of a New Mexican than the right of a competent, terminally ill patient to choose aid in dying," wrote Judge Nan G. Nash of the Second District Court in Albuquerque. The NM attorney general's office said it was studying the decision and whether to appeal to the State Supreme Court. However, this was overturned on 11 August 2015 by the New Mexico Court of Appeals, in a 2-1 ruling, that overturned the Bernalillo County District Court Ruling. The Court gave the verdict: "We conclude that aid in dying is not a fundamental liberty interest under the New Mexico Constitution".[124]
In November 2016, the citizens of Kolorado approved Proposition 106, the Colorado End of Life Options Act, with 65% in favor. This made it the third state to legalize medical aid-in-dying by a vote of the people, raising the total to six states.
The punishment for participating in physician-assisted death (PAD) varies throughout many states. The state of Wyoming does not "recognize common law crimes and does not have a statute specifically prohibiting physician-assisted suicide". In Florida, "every person deliberately assisting another in the commission of self-murder shall be guilty of manslaughter, a felony of the second degree".[125]
States currently considering physician-assisted suicide laws[iqtibos kerak ]
Alyaska, Arizona, Konnektikut, Delaver, Indiana, Ayova, Kanzas, Massachusets shtati, Michigan, Minnesota, Missuri, Nebraska, Nyu-Xempshir, Nyu York, Shimoliy Karolina, Ogayo shtati, Oklaxoma, Pensilvaniya, Rod-Aylend, Tennessi, Yuta va Viskonsin.
Washington vs. Glucksberg[muvofiq? ]
In Washington, physician-assisted suicide did not become legal until 2008.[126] In 1997, four Washington physicians and three terminally ill patients brought forth a lawsuit that would challenge the ban on medical aid in dying that was in place at the time. This lawsuit was first part of a district court hearing, where it ruled in favor of Glucksberg,[127] which was the group of physicians and terminally ill patients. The lawsuit was then affirmed by the To'qqizinchi davr.[128] Thus, it was taken to the Supreme Court, and there the Supreme Court decided to grant Washington sertifikat. Eventually, the Supreme Court decided, with a unanimous vote, that medical aid in dying was not a protected right under the constitution as of the time of this case.[129]
Bretan Meynard
A highly publicized case in the United States was the death of Bretan Meynard in 2014. After being diagnosed with terminal miya saratoni, Maynard decided that instead of suffering with the side effects the cancer would bring, she wanted to choose when she would die. She was residing in California when she was diagnosed, where assisted death was not legal. She and her husband moved to Oregon where assisted death was legal, so she could take advantage of the program. Before her death, she started the Brittany Maynard fund, which works to legalize the choice of ending one's life in cases of a terminal illness. Her public advocacy motivated her family to continue to try and get assisted death laws passed in all 50 states.[130]
Ommaviy madaniyat
- Filmlar
- Soylent Yashil
- O'lim huquqi bormi?
- Tour de Force
- How to Die in Oregon
- Men sendan oldin
- Asal
- Million Dollar Chaqaloq
- Ichkarida dengiz
- Guzaarish
- O'z joniga qasd qiluvchi sayyoh
- The Suicide Plan
- Hemlok jamiyati
- Devid Geylning hayoti
- Siz Jekni bilmayapsiz
- Paddlton
- Darvinga oxirgi taksi
- Stricken
Televizor
In the American television series Uy, physician-assisted suicide is mentioned multiple times. In "Ma'lum bo'lgan noma'lum narsalar ", Doktor Uilson, an oncologist, reveals he indirectly provided a patient dying from cancer the code to increase his morphine level to a lethal amount leading to the patient's death. In "Qazish ", O'n uchta reveals she assisted her brother in his suicide who was suffering from advanced symptoms of Xantington kasalligi and that was she was sent to prison for overprescribing. Xuddi shu epizodda, Uy promises to assist her in killing herself once her own Huntington's symptoms get too bad.
Epizodida Emmerdeyl there is a case of assisted suicide. One of the characters of the series, Jekson Uolsh, remains quadriplegic because of an accident and he has been told he will never walk again. He has expressed his desire to die, and his mate Aaron Dingl reluctantly helps him committing suicide.
Yulduzli trek mentions at least three times a case of assisted suicide. In a movie, Star Trek V: Oxirgi chegara, it is revealed that Leonard Makkoy helped his father commit suicide because of a terminal illness. It has been revealed that, some time later, there had been found a cure, and this caused McCoy a psychological pain he will have for many decades. Epizodida Yulduzli sayohat: Voyager, "Death Wish", there was a member of the Q Continuum who wanted to commit suicide because of the sufferance he'd experienced from his state of immortality. Q, inspired by this person's courage and coherence, later helped him commit suicide. Epizodida Yulduzli trek: Pikard, Icheb deb so'radi To'qqizdan etti to kill him in order to end the suffering that he had endured throughout his life.
Shuningdek qarang
- Betty and George Coumbias
- Bioetika
- Qasddan odam o'ldirish
- Evtanaziya qurilmasi
- Jek Kevorkyan
- O'lim huquqi bormi? (2008 film)
- Bretan Meynard
- Philip Nitschke
- Senitsid
- You don't know Jack (2010, film)
- Ixtiyoriy yordam bilan o'lish to'g'risidagi qonun 2017 (Viktoriya)
- Politsiya tomonidan o'z joniga qasd qilish
- A Short Stay in Switzerland (2009 yil film)
Izohlar
- ^ Qarang Baxter va Montana
Adabiyotlar
- ^ Davis, Nicola (15 July 2019). "Euthanasia and assisted dying rates are soaring. But where are they legal?". Guardian. Olingan 7 fevral 2020.
- ^ Patients Rights Council (6 January 2017). "Qo'shma Shtatlarda o'z joniga qasd qilish to'g'risidagi qonunlar". Arxivlandi asl nusxasidan 2017 yil 11 sentyabrda. Olingan 18 noyabr 2017.
- ^ a b v Emanuel, Ezekiel J.; Onwuteaka-Philipsen, Bregje D.; Urwin, John W.; Cohen, Joachim (5 July 2016). "Attitudes and Practices of Euthanasia and Physician-Assisted Suicide in the United States, Canada, and Europe". JAMA. 316 (1): 79–90. doi:10.1001/jama.2016.8499. PMID 27380345.
- ^ Hedberg, M.D., MPH., Katrina (6 March 2003). "Five Years of Legal Physician-Assisted Suicide in Oregon". Nyu-England tibbiyot jurnali. 348 (10): 961–964. doi:10.1056/NEJM200303063481022. PMID 12621146.CS1 maint: bir nechta ism: mualliflar ro'yxati (havola)
- ^ "EUTHANASIA AND ASSISTED SUICIDE (UPDATE 2007)" (PDF). Kanada tibbiyot birlashmasi. 2007. Arxivlangan asl nusxasi (PDF) 2011 yil 19 dekabrda.
- ^ "What are euthanasia and assisted suicide?". Bugungi tibbiy yangiliklar. Bugungi tibbiy yangiliklar. Olingan 12 may 2020.
- ^ "ASSISTED DYING NOT ASSISTED SUICIDE". O'limda qadr-qimmat. Olingan 21 dekabr 2018.
- ^ "Why medically assisted dying is not suicide". Dying with Dignity Canada. Olingan 21 dekabr 2018.
- ^ Starks, PhD., MPH., Helene. "Physician Aid-in-Dying". Physician Aid-in-Dying: Ethics in Medicine. Vashington universiteti tibbiyot maktabi. Olingan 29 aprel 2019.CS1 maint: bir nechta ism: mualliflar ro'yxati (havola)
- ^ "OREGON DEATH WITH DIGNITY ACT: 2015 DATA SUMMARY" (PDF). Oregon.gov. Oregon shtatidagi sog'liqni saqlash boshqarmasi. Olingan 4 oktyabr 2016.
- ^ Ganzini, Linda; Harvath, Theresa A.; Jackson, Ann; Goy, Elizabeth R.; Miller, Lois L.; Delorit, Molly A. (22 August 2002). "Experiences of Oregon Nurses and Social Workers with Hospice Patients Who Requested Assistance with Suicide". Nyu-England tibbiyot jurnali. 347 (8): 582–588. doi:10.1056/NEJMsa020562. PMID 12192019.
- ^ Wang, Shi-Yi; Aldridge, Melissa D.; Gross, Kari P.; Kanavan, Mureen; Cherlin, Emili; Johnson-Hurzeler, Rosemary; Bradley, Elizabeth (September 2015). "Geographic Variation of Hospice Use Patterns at the End of Life". Journal of Palliative Medicine. 18 (9): 771–780. doi:10.1089/jpm.2014.0425. PMC 4696438. PMID 26172615.
- ^ "OREGON DEATH WITH DIGNITY ACT: 2015 DATA SUMMARY" (PDF). Oregon shtati. Oregon shtatining sog'liqni saqlash bo'limi. Olingan 29 aprel 2019.
- ^ a b Vashington Sog'liqni saqlash vazirligi
- ^ "Living Well at the End of Life Poll" (PDF). The National Journal. 2010 yil fevral. Olingan 4 oktyabr 2016.
- ^ Ganzini, Linda; Goy, Elizabeth R.; Dobscha, Steven K.; Prigerson, Holly (December 2009). "Mental Health Outcomes of Family Members of Oregonians Who Request Physician Aid in Dying". Journal of Pain and Symptom Management. 38 (6): 807–815. doi:10.1016/j.jpainsymman.2009.04.026. PMID 19783401.
- ^ "The Right to Die with Dignity: 1988 General Resolution". Unitar universalistlar assotsiatsiyasi. 2011 yil 24-avgust. Olingan 4 oktyabr 2016.
- ^ Lagay, F (1 January 2003). "Physician-Assisted Suicide: The Law and Professional Ethics". AMA axloq jurnali. 5 (1). doi:10.1001/virtualmentor.2003.5.1.pfor1-0301. PMID 23267685.
- ^ Kass, Leon R. (1989). "Neither for love nor money: why doctors must not kill" (PDF). Jamiyat manfaatlari. 94: 25–46. PMID 11651967.
- ^ "The Internet Classics Archive - The Oath by Hippocrates". mit.edu.
- ^ "Hippocratic oath". Britannica entsiklopediyasi.
- ^ "Yunon tibbiyoti - Gippokrat qasamyodi". Tibbiyot tarixi. 2012 yil 7-fevral.
- ^ Oxtoby, Kathy (14 December 2016). "Is the Hippocratic oath still relevant to practising doctors today?". BMJ: i6629. doi:10.1136/bmj.i6629.
- ^ "WMA DECLARATION OF GENEVA". www.wma.net. 2017 yil 6-noyabr. Olingan 2 yanvar 2018.
- ^ "WMA International Code of Medical Ethics". wma.net. 1 October 2006. Archived from asl nusxasi 2012 yil 25 avgustda. Olingan 17 iyul 2014.
- ^ "WMA Statement on Physician-Assisted Suicide". wma.net. 1 May 2005. Archived from asl nusxasi 2014 yil 25 iyulda. Olingan 17 iyul 2014.
- ^ Ross Douthat (6 September 2009). "A More Perfect Death". The New York Times.
- ^ Mayo, David J.; Gunderson, Martin (July 2002). "Vitalism Revitalized: Vulnerable Populations, Prejudice, and Physician-Assisted Death". Xastings markazi hisoboti. 32 (4): 14–21. doi:10.2307/3528084. JSTOR 3528084. PMID 12362519.
- ^ a b Donovan, G. Kevin (1 December 1997). "Decisions at the End of Life: Catholic Tradition". Christian Bioethics. 3 (3): 188–203. doi:10.1093/cb/3.3.188. PMID 11655313.
- ^ a b Harvey, Kathryn (2016). "Mercy and Physician-Assisted Suicide" (PDF). Ethics & Medics. 41 (6): 1–2.
- ^ "Pope Francis Biography".
- ^ Cherry, Mark J. (6 February 2015). "Pope Francis, Weak Theology, and the Subtle Transformation of Roman Catholic Bioethics". Christian Bioethics. 21 (1): 84–88. doi:10.1093/cb/cbu045.
- ^ "Roman Catholicism". Britannica entsiklopediyasi. Olingan 7 dekabr 2016.
- ^ Yao, Teresa (2016). "Can We Limit a Right to Physician-Assisted Suicide?". Har chorakda milliy katolik bioetikasi. 16 (3): 385–392. doi:10.5840/ncbq201616336.
- ^ Samuel 1:31:4–5, Daat Zekeinim Baalei Hatosfot Genesis 9:5.
- ^ Steinberg, Dr. Abraham (1988). Entsiklopediya Hilchatit Refuit. Jerusalem: Shaarei Zedek Hospital. p. Vol. 1 Pg. 15.
- ^ "Handbook 2: Administering the Church – 21.3 Medical and Health Policies". Oxirgi kun avliyolari Iso Masihning cherkovi.
- ^ "Euthanasia and Prolonging Life". LDS News.
- ^ Godlee, Fiona (8 February 2018). "Assisted dying: it's time to poll UK doctors". BMJ: k593. doi:10.1136/bmj.k593.
- ^ "'Neutrality' on assisted suicide is a step forward". Hemşirelik Times. 2009 yil 31-iyul. Olingan 30 dekabr 2018.
- ^ Gerada, C. (2012). "The case for neutrality on assisted dying — a personal view". The British Journal of General Practice. 62 (605): 650. doi:10.3399/bjgp12X659376. PMC 3505400. PMID 23211247.
- ^ "RCN Position statement on assisted dying" (PDF). Qirollik hamshiralik kolleji.
- ^ "California Medical Association drops opposition to doctor-assisted suicide". Reuters. 2015 yil 20-may. Olingan 21 dekabr 2018.
- ^ "Massachusetts Medical Society adopts several organizational policies at Interim Meeting". Massachusetts Medical Society. Olingan 17 oktyabr 2018.
- ^ "COD Addresses Medical Aid in Dying, Institutional Racism". AAFP.
- ^ "Doctors to be asked if they would help terminally ill patients die". Xronika jonli. Olingan 14 yanvar 2019.
- ^ a b v d Seal C (2009 yil aprel). "Legalisation of euthanasia or physician-assisted suicide: survey of doctors' attitudes". Palliat Med. 23 (3): 205–12. doi:10.1177/0269216308102041. PMID 19318460. S2CID 43547476.
- ^ Canadian Medical Association (2011). "Physician view on end-of-life issues vary widely: CMA survey" (PDF). Olingan 16 oktyabr 2017.
- ^ a b Cohen, Jonathan (1994). "Attitudes toward Assisted Suicide and Euthanasia among Physicians in Washington State". Nyu-England tibbiyot jurnali. 331 (2): 89–94. doi:10.1056/NEJM199407143310206. PMID 8208272.
- ^ Lee, Melinda (1996). "Legalizing Assisted Suicide — Views of Physicians in Oregon". Nyu-England tibbiyot jurnali. 334 (5): 310–15. doi:10.1056/nejm199602013340507. PMID 8532028.
- ^ Kane, MA, Leslie. "Medscape Ethics Report 2014, Part 1: Life, Death, and Pain". Medscape. Olingan 4 oktyabr 2016.
- ^ McLean, S. (1997). Sometimes a Small Victory. Institute of Law and Ethics in Medicine, University of Glasgow.
- ^ "Legalizing Aid in Dying Doesn't Mean Patients Have Access To It". Milliy radio. Olingan 18 noyabr 2017.
- ^ "Jamoatchilik fikri - o'lishda qadr-qimmat". Olingan 4 avgust 2018.
- ^ "Shifokorlarning aksariyati hozirda qo'llab-quvvatlanmoqda. 7 fevral 2018 yil. Olingan 4 avgust 2018.
- ^ "Shifokor yordami bilan o'lish - BMA".
- ^ McGlade, K J; Slaney, L; Bunting, B P; Gallagher, A G (October 2000). "Voluntary euthanasia in Northern Ireland: general practitioners' beliefs, experiences, and actions". The British Journal of General Practice. 50 (459): 794–797. PMC 1313819. PMID 11127168.
- ^ Ponthus, Julien (20 February 2008). "Lyuksemburg parlamenti evtanaziya to'g'risidagi qonunni qabul qildi". Reuters.
- ^ Dehaas, Josh (15 January 2016). "Oliy sud Parlamentga vrachlar yordami bilan o'lish to'g'risidagi qonunni 4 oyga uzaytirdi". CTV yangiliklari.
- ^ a b Baxterga qarshi davlat, 2009 yil MT 449, 224 P.3d 1211, 354 Mont. 234 (2009).
- ^ "D.C. vrach yordamidagi o'z joniga qasd qilish to'g'risidagi qonun kuchga kiradi". Washington Times. 2017 yil 18-fevral. Olingan 16 aprel 2018.
- ^ a b "Frequently Asked Questions – About the Death With Dignity Act". Oregon shtatidagi sog'liqni saqlash boshqarmasi.
- ^ "Voluntary euthanasia is now legal in Victoria".
- ^ "Voluntary euthanasia becomes law in WA in emotional scenes at Parliament". Avstraliya teleradioeshittirish korporatsiyasi. 10 dekabr 2019 yil. Olingan 7-noyabr 2020.
- ^ "Health practitioner information on voluntary assisted dying".
- ^ "Euthanasia machine, Australia, 1995-1996".
- ^ "Moniteur Belge - Belgisch Staatsblad". fgov.be.
- ^ "Moniteur Belge - Belgisch Staatsblad". fgov.be.
- ^ Adams, M.; Nys, H. (1 September 2003). "Comparative Reflections on the Belgian Euthanasia Act 2002". Medical Law Review. 11 (3): 353–376. doi:10.1093 / medlaw / 11.3.353. PMID 16733879.
- ^ Hamilton, Graeme (10 December 2015). "Is it euthanasia or assisted suicide? Quebec's end-of-life care law explained". Milliy pochta. Toronto, Ontario. Olingan 5 yanvar 2016.
- ^ Karter Kanadaga qarshi (Bosh prokuror), 2015 S.C.C. 5, [2015] 1 S.C.R. 331.
- ^ Bill C-14, An Act to amend the Criminal Code & to make related amendments to other Acts (medical assistance in dying), 1st Sess., 42nd Parl., 2015–2016 (assented to 2016‑06‑17), S.C. 2016, c. 3.
- ^ Sog'liqni saqlash Kanada (Oktyabr 2017), Second Interim Report on Medical Assistance in Dying in Canada (PDF), Ottawa: Health Canada, ISBN 9780660204673, H14‑230/2‑2017E‑PDF.
- ^ "Euthanasia & Physician-Assisted Suicide (PAS) around the World - Euthanasia - ProCon.org". euthanasia.procon.org. Olingan 7 dekabr 2016.
- ^ a b v Zeldin, Wendy (17 August 2011). "China: Case of Assisted Suicide Stirs Euthanasia Debate". Kongress kutubxonasi.
- ^ McDougall & Gorman 2008
- ^ Uayting, Raymond (2002). Tabiiy o'lish huquqi: yigirma uch asrlik munozaralar. Westport, Konnektikut. pp.41.
- ^ Martin, Sabrina (19 February 2015). "Colombia to Finalize Euthanasia Law in March". PanAm Post. Olingan 22 iyul 2015.
- ^ Nielsen, Morten Ebbe Juul; Andersen, Martin Marchman (27 May 2014). "Bioethics in Denmark" (PDF). Cambridge Quarterly of Healthcare Ethics. 23 (3): 326–333. doi:10.1017/S0963180113000935. PMID 24867435.
- ^ a b McDougall & Gorman 2008, p. 84
- ^ McDougall & Gorman 2008, p. 86
- ^ "Germaniya Jinoyat kodeksi". Germaniya Federal Adliya vazirligi. Olingan 9 iyul 2013.
- ^ a b v d e Wolfslast, Gabriele (2008). "Physician-Assisted Suicide and the German Criminal Law". Giving Death a Helping Hand. International Library of Ethics, Law, and the New Medicine. 38. pp. 87–95. doi:10.1007/978-1-4020-6496-8_8. ISBN 978-1-4020-6495-1.
- ^ "Germaniya Jinoyat kodeksi". Germaniya Federal Adliya vazirligi. Olingan 9 iyul 2013.
- ^ "BGH Urteil vom 05.07.1983 (1 StR 168/83)". ejura-examensexpress.de. Arxivlandi asl nusxasi 2009 yil 24 fevralda. Olingan 22 avgust 2009.
- ^ "Germaniya Jinoyat kodeksi". Germaniya Federal Adliya vazirligi. Olingan 9 iyul 2013.
- ^ a b "Statistiken".[ishonchli manba? ]
- ^ a b Hurst, Samia A; Mauron, Alex (1 February 2003). "Assisted suicide and euthanasia in Switzerland: allowing a role for non-physicians". BMJ. 326 (7383): 271–273. doi:10.1136/bmj.326.7383.271. PMC 1125125. PMID 12560284.
- ^ a b "Assisted Suicide Laws Around the World - Assisted Suicide".
- ^ "Germaniya o'z joniga qasd qilish bo'yicha professional yordamni bekor qildi". Olingan 26 fevral 2020.
- ^ "Iceland". alzheimer-europe.org.
- ^ "Ireland's Health Services - Ireland's Health Service". Irlandiyaning sog'liqni saqlash xizmati. Olingan 15 noyabr 2017.
- ^ "Luxembourg strips monarch of legislative role". Guardian. London. 2008 yil 12-dekabr. Olingan 9 iyul 2013.
- ^ "Luxembourg becomes third EU country to legalize euthanasia". Tehran Times. Arxivlandi asl nusxasi 2011 yil 13 iyunda.
- ^ "Netherlands, first country to legalize euthanasia" (PDF). Jahon sog'liqni saqlash tashkiloti. 2001.
- ^ "Euthanasia is legalised in Netherlands". Mustaqil. 2001 yil 11 aprel.
- ^ a b McDougall & Gorman 2008, p. 80
- ^ "SCA overturns right-to-die ruling". Yangiliklar24. 2015 yil 6-dekabr. Olingan 6 dekabr 2015.
- ^ Schwarzenegger, Christian; Summers, Sarah J. (3 February 2005). "Hearing with the Select Committee on the Assisted Dying for the Terminally Ill Bill" (PDF). House of Lords Hearings. Syurix: Syurix universiteti Yuridik fakulteti. Arxivlandi asl nusxasi (PDF) 2011 yil 7-iyulda. Olingan 1 iyul 2009. (PDF)
- ^ "Inciting and assisting someone to commit suicide (Verleitung und Beihilfe zum Selbstmord)". Swiss Criminal Code (nemis tilida). Zürich: Süisse: Article 115. 23 June 1989.
- ^ Uayting, Raymond (2002). Tabiiy o'lish huquqi: yigirma uch asrlik munozaralar. Westport, Konnektikut. pp.46.
- ^ Christian Schwarzenegger and Sarah Summers of the University of Zurich's Faculty of Law (3 February 2005). "Hearing with the Select Committee on the Assisted Dying for the Terminally Ill Bill" (PDF). House of Lords, Zurich. Arxivlandi asl nusxasi (PDF) 2011 yil 7-iyulda. Olingan 1 iyul 2009.CS1 maint: mualliflar parametridan foydalanadi (havola)
- ^ "Swiss vote backs assisted suicide". BBC yangiliklari. 15 May 2011.
- ^ Andorno, Roberto (30 April 2013). "Nonphysician-Assisted Suicide in Switzerland" (PDF). Cambridge Quarterly of Healthcare Ethics. 22 (3): 246–253. doi:10.1017/S0963180113000054. PMID 23632255.
- ^ Lundin, Ley (2009 yil 2-avgust). "YOUhanasia". Jinoiy ma'lumot. Olingan 9 iyul 2013.
- ^ "The Suicide Tourist - FRONTLINE - PBS". pbs.org.
- ^ del Uruguay, Republica Oriental. "Penal Code of Uruguay". Urugvay parlamenti. Arxivlandi asl nusxasi 2015 yil 30-iyulda. Olingan 12 avgust 2015.
- ^ Huxtable, RichardHuxtable, Richard (2007). Euthanasia, Ethics and the Law: From Conflict to Compromise. Abingdon, Buyuk Britaniya; New York: Routledge Cavendish. ISBN 9781844721061.
- ^ "Yordam uchun o'lim haqidagi qonun loyihasi - eng so'nggi". BBC News Online.
- ^ "DPP publishes interim policy on prosecuting assisted suicide: The Crown Prosecution Service". cps.gov.uk. 23 September 2009. Archived from asl nusxasi 2009 yil 27 sentyabrda.
- ^ "A Critical Consideration of the Director of Public Prosecutions Guidelines in Relation to Assisted Suicide Prosecutions and their Application to the Law". halsburyslawexchange.co.uk. Arxivlandi asl nusxasi 2012 yil 6 martda. Olingan 4 iyun 2012.
- ^ "Dignity in Dying Poll" (PDF). Populus. 2015. Arxivlangan asl nusxasi (PDF) on 17 June 2015.
- ^ James Gallagher & Philippa Roxby (11 September 2015). "Yordam berish to'g'risida qonun: deputatlar" o'lish huquqi "to'g'risidagi qonunni rad etishdi". BBC yangiliklari.CS1 maint: mualliflar parametridan foydalanadi (havola)
- ^ "End of Life Assistance (Scotland) Bill (SP Bill 38)". Shotlandiya parlamenti. 2010 yil 21 yanvar. Olingan 12 iyun 2011.
- ^ "Margo MacDonald's End of Life Assistance Bill rejected". BBC News Online. 1 dekabr 2010 yil.
- ^ "About Us – Assisted Dying Coalition".
- ^ Lisa Aliferis (10 March 2016). "California To Permit Medically Assisted Suicide As of 9 June". Milliy radio.
- ^ "Arxivlangan nusxa". Arxivlandi asl nusxasi 2009 yil 29 iyunda. Olingan 2 iyul 2009.CS1 maint: nom sifatida arxivlangan nusxa (havola)
- ^ "Maine". Qadr bilan o'lim. Olingan 13 iyun 2019.
- ^ a b "State-by-State Guide to Physician-Assisted Suicide - Euthanasia - ProCon.org". procon.org.
- ^ a b "Oregon Public Health Division – 2013 DWDA Report" (PDF). Oregon shtatidagi sog'liqni saqlash boshqarmasi. Olingan 28 noyabr 2014.
- ^ Sullivan, Nora. "Vermont Legislature Passes Assisted Suicide Bill." Charlotte Lozier Institute RSS. Charlotte Lozier Institute, 15 May 2013. Web. 2013 yil 4-dekabr.
- ^ "Arxivlangan nusxa". Arxivlandi asl nusxasi 2014 yil 15-yanvarda. Olingan 14 yanvar 2014.CS1 maint: nom sifatida arxivlangan nusxa (havola)
- ^ Richardson, Valeri. "New Mexico court strikes down ruling that allowed assisted suicide". Washington Times. Olingan 12 avgust 2015.
- ^ "Assisted Suicide Laws in the United States | Patients Rights Council". www.patientsrightscouncil.org. Olingan 17 oktyabr 2017.
- ^ Health, Washington State Department of. "Death with Dignity Act :: Washington State Department of Health". www.doh.wa.gov. Olingan 12 noyabr 2016.
- ^ "Washington v. Glucksberg | Vacco v. Quill". www.adflegal.org. Olingan 12 noyabr 2016.
- ^ "Case Brief: Washington v. Glucksberg, 521 U.S. 702". www.studentjd.com. Olingan 12 noyabr 2016.
- ^ linderd. "Washington v Glucksberg". law2.umkc.edu. Olingan 12 noyabr 2016.
- ^ "The Brittany Fund | About". thebrittanyfund.org. Olingan 4 noyabr 2016.
Tashqi havolalar
- Asch DA, DeKay ML (September 1997). "Euthanasia among US critical care nurses. Practices, attitudes, and social and professional correlates". Med Care. 35 (9): 890–900. doi:10.1097/00005650-199709000-00002. JSTOR 3767454. PMID 9298078.CS1 maint: ref = harv (havola)
- McDougall, Jennifer Fecio; Gorman, Martha (2008). Zamonaviy dunyo muammolari: Evtanaziya. Santa Barbara, Kaliforniya: ABC-CLIO.CS1 maint: ref = harv (havola)
- "What is Physician-Assisted Suicide?". Shimoli-g'arbiy universiteti. 17 Iyul 2014. Arxivlangan asl nusxasi 2006 yil 11-iyulda. Olingan 30 iyul 2014.
- "Who Has the Right to a Dignified Death? / The Death Treatment (When should people with a non-terminal illness be helped to die?) Letter from Belgium - RACHEL AVIV". Nyu-Yorker. 2015 yil 22-iyun.
- "Uning hayotining so'nggi kuni". The New York Times jurnali. 2015 yil 17-may.
